HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: The PHE is Continuing—What’s Next for Medicaid?

- Illinois Expands Medicaid Hospital Assessment Program

- Kansas Governor Vetoes Bill to Delay Reprocurement of KanCare Contracts Until January 2023

- Medicaid Expansion News: Michigan, Missouri, North Carolina

- Medicaid Eligibility Redeterminations News: Montana, Virginia, MACPAC

- New Hampshire Governor to Sign Medicaid Adult Dental Legislation

- New Jersey Governor Proposes Expanding Medicaid Coverage to Undocumented Children

- Rhode Island to Restart Medicaid Managed Care Procurement Process

- Texas Proposes Medicaid Plan Case Management for Children, Pregnant Women

- Health Plans Call For Public Reporting of Private Equity Acquisitions

- Home Health Aides Can Have Health Premiums, Union Dues Deducted from Medicaid Paychecks

- Humana Joins Welsh, Carson, Anderson & Stowe in Primary Care Joint Venture

- Medicaid Managed Care Plan Leaders to Address Strategies, Opportunities, Concerns at HMA Conference, October 10-11

- HMA Welcomes New Colleagues

In Focus
The PHE is Continuing—What’s Next for Medicaid?
On May 16, 2022, no announcements were made concerning the impending end of the COVID-19 Public Health Emergency (PHE) declaration. What does this mean for state Medicaid programs and stakeholders, including consumers? When will the PHE declaration expire?
Today’s In Focus is the latest in our series discussing Medicaid’s preparations for the end of the PHE. HMA experts Erin Henderlight, Beth Kidder, Jane Longo, Rebecca Mendoza, and Andrea Maresca address these and other questions intertwined in the unprecedent “unwinding” work ahead for the Medicaid program.
The silence from the U.S. Department of Health and Human Services on May 16th means the Biden Administration is highly likely to sign another extension of the COVID-19 PHE declaration by July 15th. It is most likely that the PHE will then be renewed, for the maximum 3-month extension, to October 13th. While the Secretary could make an announcement to end the PHE before the full three months, the current experience with COVID-19 variants and fraught political climate make this scenario unlikely.
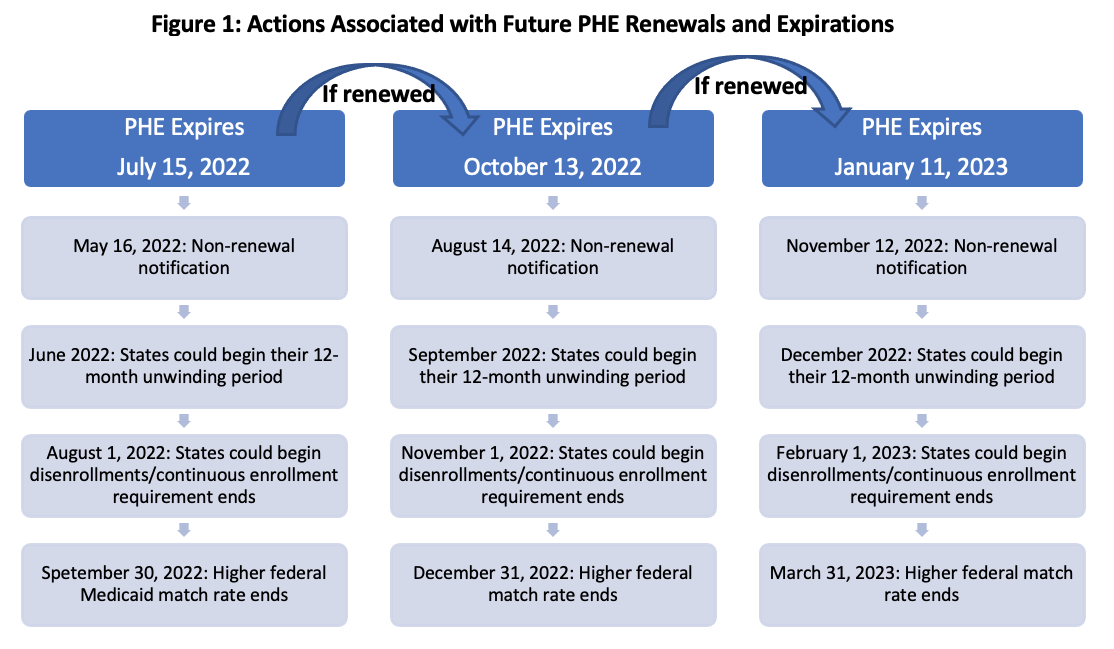
Beyond July, the Administration could continue to sign additional extensions of the PHE for the maximum three months permitted by statute. Regardless of the end date, the Administration committed to notify states and stakeholders 60 days before the scheduled end date.[i] Figure 1 describes key dates associated with potential future extensions of the COVID-19 PHE.
An extension of the COVID-19 PHE in July would provide more time to plan for its imminent end. HMA’s experts are working with stakeholders to use this additional time to develop and implement plans and improve processes to manage the PHE unwinding activities.
What Should States and Medicaid Stakeholders Do Now?
Although an extension cannot address the myriad of challenges for states and stakeholders, the following are some of the top-of-mind issues we are continuing to work with states, health plans, providers, community workers, and other stakeholders to address.
Operational and systems readiness. States and stakeholders now have more time to analyze, develop, and implement changes that will support more efficient eligibility and enrollment operations during and after the PHE unwinding period. Examples of high impact activities to support this function include:
- Stakeholders can continue to strengthen partnerships and processes to provide assistance to Medicaid enrollees and minimize unnecessary loss of coverage by eligible individuals.
- States, health plans, and other stakeholders can further solidify the operational plans for sharing member contact information files to prepare for renewals and redeterminations.
- States and stakeholders can also make on-line functionality mobile friendly and update workflow management systems.
Workforce. Training and retaining the eligibility workforce are among the most significant challenges for state and local governments. Stakeholders engaging with consumers may face similar challenges with their outreach and assistors. Strategies to alleviate some of these constraints include:
- State agencies could automate certain processes such as hand-offs to the Marketplace program.
- All stakeholders can update staffing models to support the anticipated volume of workload.
- Stakeholders should also be planning new staff training and refresher trainings, for eligibility workers and other staff who engage with Medicaid members.
Communications and outreach strategies. Working with individuals managing through complex life circumstances requires new or refreshed strategies. The months ahead will be an important time to:
- Assess relationships with trusted community partners.
- Test messaging and develop effective campaigns to engage members and trusted partners.
- Where permissible, pilot texting programs, implement opt-in for texting reminders, and improve texting capabilities to ensure two-way functionality to make the process more consumer friendly.
Marketplace collaboration and smoothing consumer transitions. Guidance from the Centers for Medicare and Medicaid Services (CMS) describes the variety of ways states can partner and engage their Medicaid health plans.[ii] One critical area that needs additional attention is the education and process for “handing off” Medicaid enrollees to the Marketplace. Some state marketing and insurance rules present barriers to smooth transitions. Potential strategies to address these challenges include:
- Stakeholders as well as state and local agencies can update and strengthen training on Marketplace requirements and processes for workers who will be engaging with consumers.
- State leaders can identify and pilot more consumer-friendly systems and processes. For example, state agencies could pilot changes to streamline health plan marketing rules designed to ease consumer transitions between coverage programs.
- State leaders and health plans can collaborate on materials and consistent messaging to support Medicaid and CHIP members transitioning to the Marketplace.
- State based marketplaces can offer special enrollment periods to help ease consumer transitions and smooth out the workload for assistors and program administrators.
Looking Ahead: Expect the Unexpected
Several recent developments make extensions of the PHE past July increasingly likely.
Notably, Administration officials and public health experts have begun discussing a potentially significant wave of COVID-19 infections and deaths this fall and winter, driven by new omicron subvariants.
Further, ending the PHE will inevitably lead to some otherwise eligible individuals losing Medicaid coverage and others to experience challenges in reconnecting with coverage. These are not favorable headlines for elected officials approaching November’s mid-term elections.
Another variable is the potential for Congress to make changes to law which links certain Medicaid policies to the PHE declaration. We cannot yet rule out the possibility that Congress could uncouple the PHE declaration from the higher federal Medicaid match rate and continuous coverage requirement (similar to a proposal incorporated in the House-passed Build Back Better Act).
Looking longer term, we are working with states and stakeholders to consider how they will assess the impact of their outreach and assistance and temporary policies. Collecting and analyzing this information as the work is underway can provide important information about effective strategies, unexpected challenges, and help with real time problem solving.
The near-term planning efforts and the operational and system transformations are applicable to the special circumstances surrounding the PHE unwinding. However, the vast majority are applicable as policymakers, state agencies, and stakeholders consider the future for consumer experiences and efficiencies for program administrators.
Please contact HMA experts Erin Henderlight, Beth Kidder, Jane Longo, Rebecca Mendoza and Andrea Maresca with questions and for more information about our work with clients to address these issues.
Related posts:
HMA Experts Lay Out Scenarios for Transitioning from COVID-19 Public Health Emergency
[i] https://www.medicaid.gov/resources-for-states/downloads/unwinding-gov-ltr-05102022.pdf
[ii] Overview of Strategic Approach to Engaging Managed Care Plans to Maximize Continuity of Coverage as States Resume Normal Eligibility and Enrollment Operations MARCH 2022 UPDATE: https://www.medicaid.gov/resources-for-states/downloads/health-plan-strategy.pdf
HMA Roundup
Georgia
Georgia Extends Medicaid Postpartum Coverage to One Year; Governor Vetoes HIV Coverage. Now Habersham reported on May 17, 2022, that Georgia Governor Brian Kemp signed legislation extending Medicaid postpartum coverage to one year from 60 days. However, Kemp vetoed language in the 2023 budget that would expand Medicaid eligibility to individuals living with HIV. Read More
Illinois
Illinois Expands Medicaid Hospital Assessment Program. WIFR reported on May 17, 2022, that Illinois Governor JB Pritzker signed legislation to extend and expand the state’s Hospital Assessment Program, a Medicaid provider tax. The program was created in 2020 to provide additional Medicaid funding to areas of the state impacted most by COVID-19. Read More
Kansas
Kansas Governor Vetoes Bill to Delay Reprocurement of KanCare Contracts Until January 2023. The Topeka Capital-Journal reported on May 13, 2022, that Kansas Governor Laura Kelly vetoed a bill that would delay the process of procuring new Medicaid managed care contracts until January 2023. The state legislature is expected to override the veto. Read More
Michigan
Michigan Medicaid Expansion Membership Tops 1 Million. Michigan Governor Gretchen Whitmer announced on May 16, 2022, that enrollment in Michigan’s Medicaid expansion program, the Healthy Michigan Plan, topped 1 million for the first time. The state implemented Medicaid expansion in 2014. Read More
Michigan Expands Behavioral Health Home Initiative to 5 More Counties. State of Reform reported on May 12, 2022, that the Michigan Department of Health and Human Services expanded its Behavioral Health Home (BHH) initiative to five counties in two Prepaid Inpatient Health Plan regions: CMH Partnership of Southeast Michigan and Detroit Wayne Integrated Health Network. Services in the expanded areas began on May 1. Read More
Minnesota
Minnesota Announces Availability of $3 Million in Rural HCBS Provider Grants. The Minnesota Department of Human Services announced on May 16, 2022, the availability of $3 million in grants for home and community-based services (HCBS) providers and organizations serving the elderly and individuals with disabilities in rural and underserved communities. Maximum grant amount is $50,000. Applications are due by June 13. Read More
Missouri
Missouri Budget Appears on Track for Governor’s Signature with $2.5 Billion in Medicaid Expansion Funding. The St. Louis Post-Dispatch reported on May 9, 2022, that Missouri’s fiscal 2023 budget, which includes $2.5 billion in funding for Medicaid expansion, appears to be on track for Governor Mike Parson’s signature. The budget, which was recently passed by the state legislature, also includes $925 million to increase payments to providers serving nursing home patients, individuals with developmental disabilities, and home-care programs. Read More
Montana
Montana to Launch Outreach Campaign to Help Medicaid Beneficiaries Stay Enrolled After PHE Ends. The Montana Department of Public Health and Human Services announced on May 11, 2022, an outreach campaign to help Montana Medicaid and Healthy Montana Kids beneficiaries stay enrolled after the end of the public health emergency (PHE). Read More
Nebraska
Nebraska Hospitals Spend $737 Million on Charity Care in 2020, Report Says. The Lincoln Journal Star reported on May 12, 2022, that Nebraska hospitals spent $737 million on charity and unreimbursed care in 2020, the highest amount since 2016, according to a report from the Nebraska Hospital Association. Nebraska hospitals spent another $186 million writing off bad debt. Total spending on non-traditional benefits to support community health was $1.4 billion. Read More
New Hampshire
Governor to Sign Medicaid Adult Dental Legislation. The New Hampshire Bulletin reported on May 13, 2022, that New Hampshire Governor Chris Sununu is expected to sign legislation expanding Medicaid dental coverage to 85,000 adults in the state. The legislation was recently passed by the state House and Senate. Funding for the first three years would come from a $21 million settlement the state reached with Centene over Medicaid pharmacy benefit management costs. Read More
New Jersey
Governor Proposes Expanding Medicaid Coverage to Undocumented Children. New Jersey 101.5 reported on May 10, 2022, that New Jersey Governor Phil Murphy wants to allocate $11 million to expand Medicaid eligibility to undocumented children through the second phase of the state’s Cover All Kids initiative. The expansion, included in Murphy’s fiscal 2023 proposed budget, would provide coverage to an estimated 18,000 undocumented individuals. Read More
North Carolina
Governor Proposes Medicaid Expansion in Fiscal 2023 Budget. WCNC reported on May 11, 2022, that North Carolina Governor Roy Cooper included Medicaid expansion in his proposed state budget for fiscal 2023, with funding provided by the federal government and a premium tax. An estimated 600,000 North Carolinians would receive coverage through expansion. Read More
Ohio
Medicaid Director Owned Stock in Managed Care Contract Winners. The Ohio Capital Journal reported on May 17, 2022, that Ohio Medicaid Director Maureen Corcoran owned at least $1,000 in stock of CVS Health/Aetna, Humana, and UnitedHealth Group, which were awarded Medicaid managed care contracts in the past year. Humana and UnitedHealth are two of seven winners of statewide Medicaid managed care contracts. CVS Aetna was awarded a contract for OhioRISE, a managed care program for children with behavioral health needs. Read More
Rhode Island
Rhode Island to Restart Medicaid Managed Care Procurement Process. WPRI reported on May 13, 2022, that the Rhode Island Department of Administration cancelled the current bidding process for $7 billion in state Medicaid managed care contracts and will start over. The state said contract language would need to be updated to reflect federal regulatory changes. The original bids were due in late January, but Tufts Health Plan was disqualified for missing the bid deadline, and Blue Cross Blue Shield of Rhode Island was facing potential disqualification for submission errors. Read More
Texas
Texas Seeks to Transition Medicaid Case Management for Children, Pregnant Women to Managed Care. The Centers for Medicare & Medicaid Services announced on May 16, 2022, that Texas is seeking federal approval to transition Medicaid case management for children and pregnant women from fee-for-service to managed care. The state proposed the change in an amendment to an existing Medicaid 1115 waiver program called the Texas Healthcare Transformation and Quality Improvement Program. The case management system assists eligible children and pregnant women with accessing necessary medical, social, educational, and other services. Public comments will be accepted through June 15. Read More
Virginia
Virginia Launches Outreach Campaign to Help Medicaid Beneficiaries Stay Enrolled After PHE Ends. The Richmond Times-Dispatch reported on May 13, 2022, that Virginia has launched an outreach campaign to keep Medicaid beneficiaries informed about the eligibility redetermination process that will resume after the public health emergency (PHE) ends. Beneficiaries are being told in ads on social media, for example, to make sure their contact information is updated. Additional communications will be made on radio, television, and through mailings to more than 1.1 million households. Read More
National
Health Plans Call For Public Reporting of Private Equity Acquisitions. Modern Healthcare reported on May 17, 2022, that health insurers are calling on Congress to require private equity companies and hedge funds to publicly report healthcare acquisitions, including purchases of ambulance providers, emergency room physician practices, and other specialty groups. In a letter to President Biden and congressional leaders, insurance industry group AHIP also wants increased regulatory scrutiny of the anti-competitive effects of private equity deals. Read More
Lowering Age of Medicare Eligibility to 60 Would Reduce Medicaid Enrollment, CBO Projects. The Congressional Budget Office projected on May 16, 2022, that lowering the age of Medicare eligibility to 60 would reduce the number of individuals with Medicaid as their primary source of coverage by about 1.8 million, with almost all of them enrolling in Medicare. The change would also reduce the number of uninsured individuals and increase the federal deficit by $155 billion over the 2026–2031 period. Read More
HHS Announces $15 Million SAMHSA Nursing Home Behavioral Health Grant. The U.S. Department of Health and Human Services announced on May 16, 2022, the availability of a $15 million, three-year grant to address serious mental illness, serious emotional disturbance, substance use issues, or co-occurring mental health and substance use conditions in nursing homes. The grant, which is offered in partnership with the Substance Abuse and Mental Health Services Administration (SAMHSA), will be used to establish a Center of Excellence to directly consult nursing homes and long-term care facilities to improve behavioral health care. Read More
MACPAC Says Text Messaging Could Be ‘Important Tool’ During Medicaid Eligibility Redeterminations. The Medicaid and CHIP Payment and Access Commission (MACPAC) said on May 16, 2022, that text messages and automated pre-recorded cell phone calls could be an important tool when states resume Medicaid beneficiary eligibility redeterminations at the end of the public health emergency (PHE). MACPAC issued the opinion in a letter to the Federal Communications Commission. Read More
CMS Says Independent Home Health Aides Can Have Health Premiums, Union Dues Deducted from Medicaid Paychecks. Modern Healthcare reported on May 12, 2022, that the Centers for Medicare & Medicaid Services (CMS) issued a rule that state Medicaid agencies can once again allow independent home health aides to deduct healthcare premiums and union dues from their paychecks. The rule is not mandatory, but removes certain barriers put in place in 2019. Read More
Healthcare Groups Urge HHS to Extend PHE Beyond July 16. Fierce Healthcare reported on May 11, 2022, that a group of healthcare advocates, including the American Hospital Association and the American Medical Association, have urged the Biden administration to extend the public health emergency (PHE) beyond July 16. U.S. Health and Human Services (HHS) Secretary Xavier Becerra has said he will give stakeholders 60-days notice of the end of the PHE. Read More
25 Percent of Medicare Patients Experienced Harm During Acute Care Stays, Report Says. Modern Healthcare reported on May 13, 2022, that 25 percent of Medicare recipients who had short-term acute-care hospital stays in 2018 experienced harm, according to a report from the U.S. Office of the Inspector General. This rate is very similar to the 27 percent patient harm reported in 2010. Incidents of harm were related to medication, patient care, procedures and surgeries, and infections. Forty-three percent were preventable, and 74 percent resulted in a prolonged facility stay. Read More
Medicare ACOs Say Challenges of Demonstrating ROI Is Roadblock to Home Health. Modern Healthcare reported on May 12, 2022, that three-quarters of Accountable Care Organizations (ACOs) participating in the Medicare Shared Savings Program do not provide home-based care programs because of the challenges of demonstrating return on investment. According to a survey published in the American Journal of Managed Care, about 25 percent have home care programs, while another 25 percent offer some home visits. Read More
Industry News
24 Hour Home Care Acquires Trusted Life Care. In-home care company 24 Hour Home Care announced on May 16, 2022, the acquisition of California-based Trusted Life Care, a senior home care agency that provides personal care services in Orange and Los Angeles counties. Read More
Humana Joins Welsh, Carson, Anderson & Stowe in Primary Care Joint Venture. Humana and investment firm Welsh, Carson, Anderson & Stowe (WCAS) announced on May 16, 2022, a joint venture to invest an additional $1.2 billion to develop 100 primary care clinics for Medicare members between 2023 and 2025. The two organizations have an existing collaboration to invest up to $800 million to open 67 clinics by early 2023. WCAS will own a majority stake in the joint venture, with clinics operating under the Humana’s CenterWell Senior Primary Care brand. Read More
Advocate Aurora Health, Atrium Health to Merge. Fierce Healthcare reported on May 11, 2022, that Advocate Aurora Health and Atrium Health are merging to form a not-for-profit health system with 67 hospitals in six states. The joint system will operate under the Advocate Health name and serve 5.5 million patients annually, making it one of the largest health systems in the nation. Eugene Woods, president and chief executive of Atrium Health, and Jim Skogsbergh, president and chief executive of Advocate Aurora Health, will serve as co-chief executives immediately following the merger. Read More
RFP Calendar

HMA Welcomes
Briana Jacob, MBA – Senior Consultant
A solutions-driven healthcare leader with experience in analysis, technical and operational improvements and collaborative leadership, Briana Jacob has led cross-functional teams and developed strategic pathways to increase productivity, improve outcomes and maximize productivity.
As a former chief executive officer/chief operating officer with Acadia Healthcare, she revised policies and procedures to increase efficiency, capacity, and business development to align with strategic rebranding and long-term objectives as well as improved compliance. Her expertise also includes substance use disorder and behavioral health facility development and operations, advocacy and behavioral health market evaluation and strategic planning.
Prior to her executive roles, Briana served as director of business operations, also with Acadia Healthcare. In this role she improved the revenue cycle which reduced outstanding accounts and cut accounts receivable days. She consistently exceeded monthly department cash collection goals and bolstered revenue by increasing upfront cash collections.
In addition to her outcome improvement and strategic leadership, she also has credentialling and patient registration experience as well as a collaborative approach to data collection and completion.
She earned a bachelor’s degree in psychology and English from Oakland University and a Master of Business Administration from Amberton University.
Allie Franklin, LICSW – Principal
Allie Franklin is a licensed clinical social worker with decades of experience in public, private, and non-profit behavioral health, healthcare, and social service organizations. She has led transformations in integrated care through modernizing processes, systems, workflows, policies, and organizational approaches to achieve positive outcomes. She brings a perspective of clinical, operational, and strategic expertise that comes from having worked on the clinical front lines and rising to roles in senior and executive leadership. This gives her the ability to support planning and implementation of solutions from system and organization-wide approaches to day-to-day clinical level work.
Prior to joining HMA, Allie served the as the behavioral health service line administrator for the University of Washington’s Harborview Medical Center, the region’s only Level One Trauma Center. This role encompassed inpatient behavioral healthcare, emergency psychiatric services, a full outpatient clinic, and scattered site integrated behavioral health and primary care. As part of her service line’s Center of Excellence, the Behavioral Health Institute, she managed a project to bring together multiple stakeholders to redesign Washington’s (WA) behavioral health crisis system in preparation for 988 crisis line rollout.
In her role as the associate vice president of clinical operations for a Medicaid managed care organization in Pierce County, WA, Allie led a multi-disciplinary team of executives and community stakeholders through the development and implementation of a detailed plan to integrate mental health services with substance use disorder services into a behavioral health organization. Allie has also served as the chief executive officer for one of Washington state’s two largest suicide hotlines where she led the transformation to meet NCQA call quality standards.
With a passion for whole person wellness, developing high performing teams, and helping clinical staff understand how their work impacts the financial bottom line, Allie has a unique combination of experiences across the care continuum from crisis care and inpatient treatment to outpatient and integrated primary care models. Her perspective, gained from leading on both sides of the payer relationship, gives her the ability to support system transformation to help build approaches that achieve high quality and affordability.
Allie earned a Master of Science in Social Work from the University of Texas at Arlington, a Bachelor of Social Work from Missouri State University and is currently working toward an Executive Master of Health Administration from the University of Central Florida. She also served in the United States Air Force, reaching the rank of Captain, serving as chief of mental health for Columbus Air Force, and as a clinical member of the international critical incident crisis response team.
Allie has published multiple books and articles on grief and grieving, and she is a co-author of a peer reviewed article, Progress Monitoring in an Integrated Health Care System: Tracking Behavioral Health Vital Signs. This article outlines the work her teams led at Group Health Cooperative to develop integrated care models for collaboration between primary care and behavioral health services.
Michele Bosworth, MD – Principal
Dr. Michele Bosworth is a physician leader dedicated to collaboration and strategic approaches to population health through the effective and efficient use of health information technology (HIT) as well as clinical and executive leadership experience.
She joins HMA after serving in various leadership positions with the University of Texas Health Science Center at Tyler (UTHSCT) with her latest role being the founding executive director of the UTHSCT Center for Population Health, Analytics, and Quality Advancement. While there, she achieved maximum financial performance of 1115 Waiver Delivery System Reform Incentive Payment (DSRIP) program, oversaw externally funded programs, and aligned academic, clinical, and community initiatives.
Dr. Bosworth used her Lean Six Sigma Green Belt skillset, experience as a former chief quality officer and expertise in clinical informatics to successfully perform within the DSRIP program. She worked with community partners on 43 measures in chronic disease, maternal and fetal safety, dental, behavioral health, and preventive care to develop, deploy and oversee a population health team. The team, made up of community health workers, medical assistants, and patient service coordinators and led by a registered nurse, performed pre-visit planning with standing delegated orders and scripting, education to manage patient health needs and visit expectations, post-visit behavioral health management, and transitional care management.
Dr. Bosworth oversaw the optimal design and use of the electronic health record (EHR) and associated workflows and documentation to promote population health team success. Additionally, her oversight led to continuous alignment with managed care star ratings/HEDIS measures to occur collaboratively.
In addition, Dr. Bosworth implemented food insecurity screening in all primary care clinics, co-developed the Partners in Health program to connect patients with the East Texas Food Bank, and deployed an emergency food box program.
With her experience as a previous chief medical information officer (CMIO) and board certification in clinical informatics, Dr. Bosworth capitalized on ensuring integration of population health programmatic needs with the EHR which subsequently enabled meaningful data for performance improvement. She also facilitated many telehealth initiatives with psychiatry, psychology, and supportive care. Under her leadership as CMIO, she led various EHR implementations, upgrades, and optimization initiatives such as standardization of medication reconciliation, referral management, and Computerized Physician Order Entry (CPOE). Dr. Bosworth developed, deployed, and led the Clinical Informatics Governance and authored associated policies and procedures necessitating optimal and meaningful use of the EHR. Lastly, regulatory accomplishments included maximized performance with Meaningful Use, Merit-based Incentive Payment System (MIPS), and achieving Healthcare Information and Management Systems Society (HIMSS) Level 6.
In the Center for Population Health, Analytics, and Quality Advancement, Dr. Bosworth oversaw a Community Health Worker (CHW) training program as well as multiple externally funded lifestyle change programs including the CDC’s Diabetes Prevention Program, Hypertension workshops, MD Anderson’s Active Living after Cancer, and Smoking Cessation Program, all delivered by CHWs.
She earned a Medical Doctorate at West Virginia School of Medicine in Morgantown, West Virginia, as well as a bachelor’s degree in biology from West Virginia University. She is a fellow of the American Academy of Family Physicians, a diplomat of the American Board of Preventive Medicine in clinical informatics, and a Lean Six Sigma Green Belt.
Tia Cintron, MHA – Managing Principal
Tia Cintron is an experienced and innovative professional with more than 20 years leading health and social service transformation initiatives focused on health equity and access as well as 10 years in residential community housing planning and development.
She has a broad background that includes strategic planning, program design and implementation, and operations management and stakeholder engagement leadership within government programs. In addition, she has worked extensively in Medicaid managed care, community-based organizations, and housing development.
Tia’s leadership has included serving as the founding chief executive officer of the Connecticut Insurance Exchange Marketplace, the founding chief operating officer of a non-profit health plan cooperative, a founding partner in a large-scale community housing development, and a senior advisor for Delivery System Reform Incentive Payment (DSRIP) program developments in both New York and Massachusetts.
Passionate about contributing to impactful community development initiatives, Tia has worked to further value-based healthcare and strengthen integration of social services with primary care to improve conditions for underserved and vulnerable populations.
She considers herself a lifelong learner and is currently working towards a master’s degree in clinical social work from Boston University. Additionally, Tia earned master’s in healthcare administration from San Jose State University and a Bachelor of Science in political science from Portland State University.
Dedicated to improving access to healthcare for low-income populations, Robin Preston has been working in the policy and operations spaces of healthcare for more than 30 years. During her career, she has worked in the private sector and in managed care organizations, including comprehensive and behavioral health, in addition to working as a public servant with the Centers for Medicare and Medicaid Services (CMS).
Robin A. Preston – Regional Vice President
Before joining HMA, she served as associate partner for the Policy and Program Management practice within the IBM Watson Health’s Federal Consulting practice. While there, she served as subject matter expert on contracts covering value-based payment; Medicaid; managed care, including encounter data; home and community-based services (HCBS); and substance use disorder treatment and access.
As a civil servant, Robin spent more than eight years in increasingly more senior roles with CMS where she was instrumental in the implementation of the Affordable Care Act (ACA) at the federal level. She led implementation in 21 states that used managed care as a delivery system and led teams that oversaw Medicaid expansion in several states as well.
In addition, her work with CMS included coordinating federal Medicaid response to crises including natural disasters, Zika healthcare emergency and the Flint, Michigan, water crisis. She managed regional offices and stakeholder relations and served as liaison to several associations and boards.
Prior to her career with CMS, Robin worked for a Medicaid managed care plan and had the opportunity to implement the DC Healthcare Alliance program for uninsured adults in the District of Columbia. She also coordinated the opening of The Bridge Homeless Shelter in Dallas, Texas, with onsite behavioral health services, implemented pay for performance provider incentives for better patient outcomes, and helped plan enrollees navigate the healthcare system.
Robin earned a Bachelor of Science degree from the University of Maryland.
HMA News & Events
Medicaid Managed Care Plan Leaders to Address Strategies, Opportunities, Concerns at HMA Conference in Chicago, October 10-11. Top Medicaid managed care executives from Aetna, AmeriHealth Caritas, Anthem, Centene, Humana, and UnitedHealthcare will discuss key strategies, opportunities, and concerns for Medicaid managed care plans during a keynote Q&A session at the fifth annual HMA conference, October 10-11, 2022, at the Fairmont Chicago, Millennium Park. To register visit https://conference.healthmanagement.com/.
Confirmed speakers to date include (in alphabetical order):
Keynote Q&A: Key Strategies, Opportunities, and Concerns for Medicaid Managed Care
John Barger, National VP, Dual Eligible and Medicaid Programs, Humana, Inc.
Aimee Dailey, President, Medicaid, Anthem, Inc.
Rebecca Engelman, EVP, Medicaid Markets, AmeriHealth Caritas
Brent Layton, President, COO, Centene Corporation
Kelly Munson, President, Aetna Medicaid
Timothy Spilker, CEO, UnitedHealthcare Community & State
Keynote Q&A: State Medicaid Priorities, Challenges – Now and After the Public Health Emergency
Jacey Cooper, Medicaid Director, Chief Deputy Director, California Department of Health Care Services
Allison Matters Taylor, Medicaid Director, Indiana
Dave Richard, Deputy Secretary, North Carolina Medicaid
Jami Snyder, Director, Arizona Health Care Cost Containment System
Keynote Address: Politics and the ‘New Normal’ for U.S. Healthcare
Drew Altman, President and CEO, Kaiser Family Foundation
Featured Speakers
Michael Brodsky, MD, Medical Director, Behavioral Health and Social Services, L.A. Care Health Plan
Cindy Cota, Director of Managed Medicaid Growth and Innovation, Volunteers of America
Daniel Elliott, MD, Medical Director, Christiana Care Quality Partners, eBrightHealth ACO, ChristianaCare Health System
Rebecca Engelman, EVP, Medicaid Markets, AmeriHealth Caritas
Martin Lupinetti, President, CEO, HealthShare Exchange (HSX)
Andrew Martin, National Director of Business Development (Housing+Health), UnitedHealth Group
Todd Rogow, President, CEO, Healthix
Debra Sanchez-Torres, Senior Advisor, Centers for Disease Control and Prevention
Mark Sasvary, Chief Clinical Officer, CBHS, IPA, LLC
Jim Sinkoff, Deputy Executive Officer, CFO, SunRiver Health
Tim Skeen, Senior Corporate VP, CIO, Sentara Healthcare
Courtnay Thompson, Market President, Select Health of SC, an AmeriHealth Caritas Company
Joshua Traylor, Senior Director, Health Care Transformation Task Force
Amanda Van Vleet, Associate Director, Innovation, NC Medicaid Strategy Office, North Carolina Department of Health & Human Services
Shannon Wilson, VP, State Markets East, Priority Health
The overall theme of this year’s conference is How Medicaid, Medicare, and Other Publicly Sponsored Programs Are Shaping the Future of Healthcare in a Time of Crisis. HMA will also host a pre-conference workshop on Sunday, October 9, on important trends and developments in value-based care.
HMA’s last national conference brought together 500 executives from health plans, providers, state and federal government, community-based organizations and others serving Medicaid, Medicare, and other vulnerable populations. Sponsorships and group discounts are available. For additional information, contact Carl Mercurio.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
- Arizona Medicaid Managed Care Enrollment is Up 1.3%, Feb-22 Data
- Kentucky SNP Membership at 64,932, Mar-22 Data
- Maine SNP Membership at 30,261, Mar-22 Data
- Massachusetts SNP Membership at 63,799, Mar-22 Data
- Michigan SNP Membership at 88,576, Mar-22 Data
- Minnesota SNP Membership at 51,325, Mar-22 Data
- Mississippi SNP Membership at 58,868, Mar-22 Data
- Montana SNP Membership at 3,565, Mar-22 Data
- New Jersey SNP Membership at 71,423, Mar-22 Data
- North Dakota SNP Membership at 190, Mar-22 Data
- Washington SNP Membership at 88,757, Mar-22 Data
- West Virginia Medicaid Managed Care Enrollment is Up 2.5%, Apr-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Delaware HCBS for Individuals with Intellectual and Developmental Disabilities RFP, May-22
- Minnesota HCBS Provider Capacity Grants for Rural, Underserved Communities RFP, May-22
- New Hampshire Medicaid System Evaluation RFP, May-22
Medicaid Program Reports, Data and Updates:
- Colorado External Quality Technical Reports for Children’s Health Plan Plus, 2016-21
- Pennsylvania Eligibility Aid, Income-Asset Limits, Citizenship Requirements Documentation, May-22
- Pennsylvania HealthChoices Behavioral Health Rate Development and Certifications, CY 2019-22
- Pennsylvania HealthChoices Physical Health Rate Development and Certification, CY 2019-22
- South Carolina Medicaid Quality Strategy Draft, May-22
- Washington Apple Health Managed Care Children with Chronic Conditions CAHPS Report, 2017-21
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
About HMA
HMA is an independent, national research and consulting firm specializing in publicly funded healthcare and human services policy, programs, financing, and evaluation. We serve government, public and private providers, health systems, health plans, community-based organizations, institutional investors, foundations, and associations. Every client matters. Every client gets our best. With more than 20 offices and over 500 multidisciplinary consultants coast to coast, our expertise, our services, and our team are always within client reach.
Among other services, HMA provides generalized information, analysis, and business consultation services to investment professionals; however, HMA is not a registered broker-dealer or investment adviser firm. HMA does not provide advice as to the value of securities or the advisability of investing in, purchasing, or selling particular securities. Research and analysis prepared by HMA on behalf of any particular client is independent of and not influenced by the interests of other clients.
