Arkansas
Arkansas Lawmakers File Bill to Extend Postpartum Medicaid Coverage From 60 Days to 12 Months. The Arkansas Democrat-Gazette reported on November 21, 2022, that Arkansas lawmakers filed several health bills ahead of the legislative session that starts in January 2023, including one (HB 1010) that would extend postpartum Medicaid coverage from 60 days to 12 months. Other bills would require Arkansas Medicaid to cover depression screenings of pregnant women (HB 1011), authorize Medicaid to reimburse for nonemergency transportation from a beneficiary’s home to a healthcare facility (HB 1009), and modify the coverage of continuous glucose monitors (HB 1008). Read More
Arkansas Medicaid Looks to Expand Access to Behavioral, Mental Health Services. The Northwest Arkansas Democrat-Gazette reported on November 20, 2022, that the Arkansas Department of Human Services is readying changes to the state’s Medicaid program aimed at expanding behavioral and mental health care services. The changes include reimbursing providers for more preventive care and screenings, allowing clinicians to provide more oversight, and efforts to reduce the labor shortage. The proposals come from a task force created by state lawmakers in 2021 to study issues around mental health. The changes need to be approved by the Arkansas Legislative Council. Read More
California
California Medicaid Cannot End AIDS Healthcare Foundation Contract, Judge Rules. Bloomberg Law reported on November 29, 2022, that a federal judge issued a preliminary injunction blocking California from terminating its Medicaid contract with the AIDS Healthcare Foundation (AHF), which provides healthcare coverage and care to Medi-Cal beneficiaries with AIDS and HIV. The lawsuit stems for a California Department of Health Care Services decision to allow its contract with AHF to expire at the end of 2021 after AHF sent a letter to its members saying it would not be able to operate in 2022 unless the state increased funding. Read More
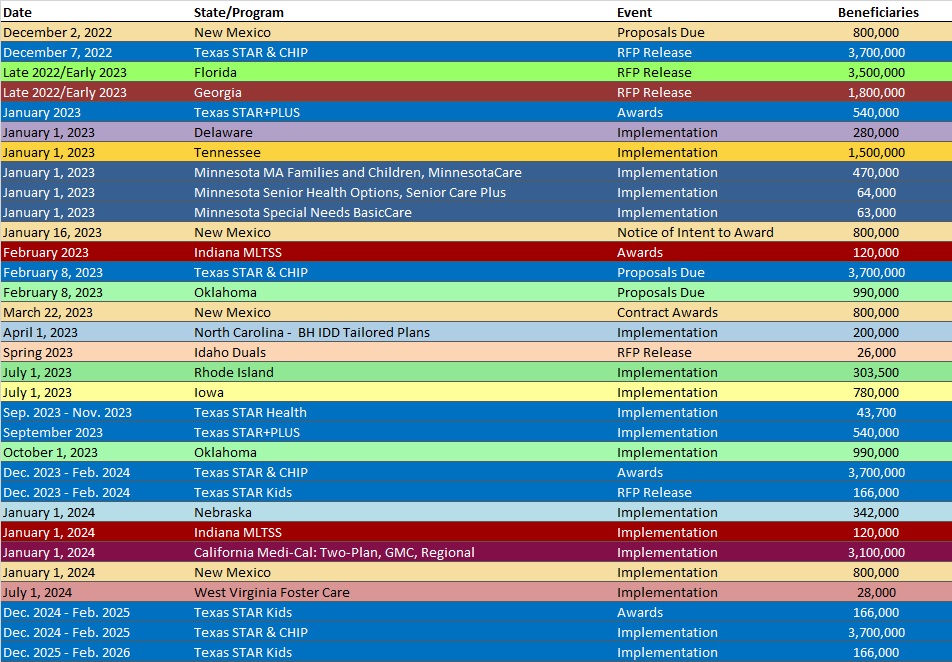
California Seeks Federal Approval to Limit Medicaid Managed Care Choice in Metro, Urban Counties. The Centers for Medicare & Medicaid Services announced on November 18, 2022, that California submitted an amendment to the CalAIM Section 1115 waiver demonstration that would limit choice of Medicaid managed care plans in metro, large metro, and urban counties. The move is aimed at helping counties involved or interested in County Organized Health System or Single Plan managed care models. The new models would be implemented on January 1, 2024. Public comments will be accepted through December 18, 2022. Read More
Delaware
Delaware Medicaid Requests Additional $70 Million in Fiscal 2024 Budget for PHE Unwinding. Delaware Public Media reported on November 26, 2022, that the Delaware Department of Health and Social Services (DHSS) is requesting an additional $70 million in its preliminary fiscal 2024 budget proposal for one-time Medicaid costs associated with the unwinding of the public health emergency. DHSS will use the additional funding to educate beneficiaries about changes in benefits and to implement federal requirements during the unwinding process. Read More
Florida
Florida Medicaid Secretary Is Stepping Down. Health News Florida/News Service of Florida reported on November 22, 2022, that Florida Agency for Health Care Administration (AHCA) Secretary Simone Marstiller is stepping down, effective December 30. Marstiller has led AHCA since February 2021. Read More
Florida Releases Medicaid Managed Care Data Books Ahead of Procurement Process. Florida Politics reported on November 22, 2022, that the Florida Agency for Health Care Administration released data books for the upcoming statewide Medicaid managed care (SMMC) procurement, including both the Managed Medical Assistance Program Data Book and the Long-Term Care Program Data Book. By state law, data books must be released 90 days before issuing an invitation to negotiate. The state will host a public meeting on January 5, 2023, to address questions. Read More
Georgia
Georgia to Implement Medicaid Expansion Work Requirements in July 2023. The Georgia Virtue reported on November 29, 2022, that Georgia will implement work requirements for its Medicaid expansion program in July 2023. The expansion program, known as Pathways to Coverage, will require 80 hours of work or volunteering per month in order to qualify for coverage. Read More
Georgia Renews Physician, Hospital Directed Payment Programs for Fiscal 2023. The Georgia Department of Community Health announced on November 21, 2022, renewal of the state’s Physician Directed Payment Program (PDPP) and Hospital Directed Payment Program (HDPP) for fiscal 2023. PDPP provides state directed payments to eligible physicians and practitioners who are affiliated with a government teaching hospital, and HDPP provides additional Medicaid funding to eligible public hospitals. Read More
Idaho
Idaho Delays Medicaid Behavioral Health Plan Contract Award. Health Payer Specialist reported on November 21, 2022, that Idaho has delayed the award announcement of the new Medicaid behavioral health plan contracts to the end of December, after an initial delay to November. The state received bids from incumbent UnitedHealth Group/Optum, as well as Elevance/Beacon Health and Centene/Magellan Healthcare. Read More
Louisiana
Louisiana Legislative Task Force Studies Rural Health Disparities. The Center Square Louisiana reported on November 18, 2022, that the Louisiana House Health and Welfare Committee heard hearings on the struggles faced by rural healthcare providers across the state, with testimony including comments on staffing shortages and access to transportation and care. A legislative taskforce has been created to study rural health disparities and report to the legislature by March 1, 2023. Read More
Michigan
Michigan to Cover Doula Services for Medicaid Beneficiaries in 2023. The Detroit News reported on November 27, 2022, that Michigan will cover doula services provided to Medicaid beneficiaries in 2023. Doulas must be enrolled as Medicaid providers and listed on the Michigan Department of Health and Human Services Doula Registry. The state will also create a division to support doula workers. Read More
Minnesota
Minnesota Awards $7 Million to HCBS Service Providers for Seniors. The Minnesota Department of Human Services announced on November 29, 2022, $7 million in grants to 57 organizations for home and community-based services (HCBS) for seniors through the state’s Live Well at Home program. Funding will go toward caregiver support, help with housekeeping, modifications to prevent falls, and accessible gardens. Read More
Mississippi
Mississippi Rural Hospitals Are At Risk of Closing. The Associated Press reported on November 22, 2022, that 54 percent of Mississippi’s rural hospitals are at risk of closing, with COVID-19 and labor costs contributing to the financial strain, according to Daniel Edney, MD, state health officer for the Mississippi Department of Health. Edney made the comments at a hearing for state senators. Read More
Mississippi Medicaid Managed Care Enrollment Falls As State Shifts Members to FFS During Public Health Emergency. Mississippi Today reported on November 17, 2022, that Mississippi has shifted tens of thousands of Medicaid members from managed care to fee-for-service during the pandemic. The shift is aimed at beneficiaries who have technically lost Medicaid eligibility or have failed to update their eligibility information. From June 2021 to September 2022 Medicaid managed care enrollment in the state decreased by 26 percent. Read More
Montana
Montana Faces Lawsuit Concerning Hiring of Medicaid Director. The Daily Montanan reported on November 16, 2022, that Disability Rights Montana filed a lawsuit in state court seeking information on the hiring of Mike Randol as Montana’s Medicaid and health services executive director. Previously, Randol oversaw Medicaid programs in Iowa and Kansas, which both use managed care models. The Montana Department of Public Health and Human Services has declined to provide materials related to the hiring, including his resume and interview questions. Read More
New Mexico
New Mexico Lawmakers Eye Assistance for Medicaid Members Who Lose Coverage After End of Public Health Emergency. The Albuquerque Journal reported on November 16, 2022, that the New Mexico legislature is considering a request to allocate $92 million from the state’s health care affordability fund to reduce insurance costs for individuals purchasing Exchange plans and to expand coverage options. The request is aimed at helping a projected 80,000 individuals who are expected to lose Medicaid coverage at the end of the public health emergency (PHE).
New York
New York Allocates $3.3 Million to Increase Access to Youth Mental Health Services. New York Governor Kathy Hochul announced on November 18, 2022, awards of $3.3 million in federal funding for community-based healthcare providers to serve children and youth who are dually diagnosed with mental illness and a developmental disability or substance use disorder. The funding, made available through the American Rescue Plan Act, was allocated to more than 80 organizations. Read More
New York Makes $194 Million in Medicaid Overpayments from 2021-22, Audit Finds. The Gotham Gazette reported on November 17, 2022, that New York made more than $194 million in Medicaid overpayments from March 2021 to March 2022 after state officials failed to make sure beneficiaries were enrolled in the correct coverage, according to a state audit. The audit urges the Department of Health (DOH) to review and recover the overpayments as well as to move eligible recipients from coordinated care plans to cheaper fee-for-service coverage. The recommendations are nonbinding. DOH has 180 days to respond. Read More
North Dakota
North Dakota Attorney General to Seek Additional State Funds to Expand Medicaid Fraud Unit. Valley News Live reported on November 28, 2022, that North Dakota Attorney General Drew Wrigley will ask lawmakers for additional funding to expand the state’s Medicaid fraud unit. The unit, which is about 25 percent state-funded and 75 percent federally funded, has a budget of $1.2 million per biennium. Read More
Oklahoma
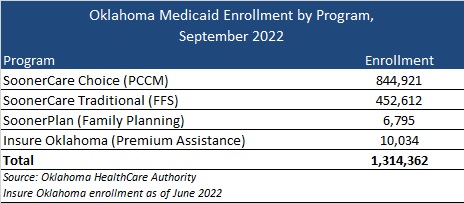
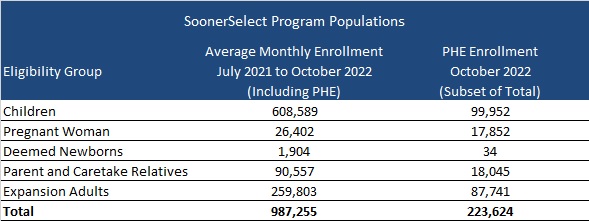
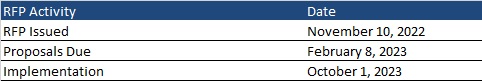
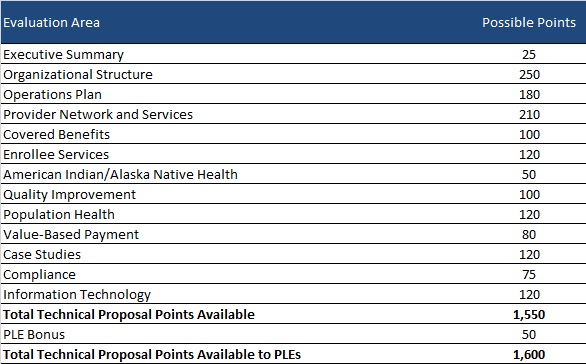
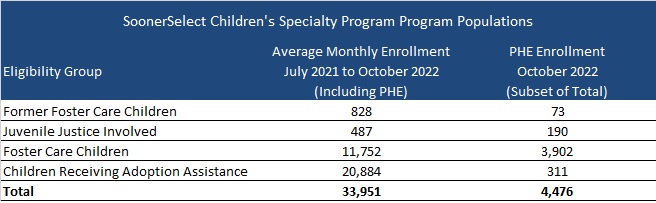
Oklahoma Releases SoonerSelect Children’s Specialty Program RFP Covering Foster Kids. The Oklahoma Health Care Authority released on November 10, 2022, a request for proposals (RFP) for the state’s SoonerSelect Children’s Specialty Program, which covers medical, behavioral, and pharmacy services for current and former foster children, justice-involved children, and children receiving adoption assistance. The state intends to award one contract, effective October 1, 2023, through June 30, 2024, with five, one-year renewal options. Read More
Oregon
Oregon Waiver Amendment Proposes Continuous Medicaid Coverage for Certain Beneficiaries Until State Establishes Basic Health Program. The Centers for Medicare & Medicaid Services announced on November 30, 2022, that Oregon submitted an amendment to its Section 1115 substance use disorder demonstration requesting continuous Medicaid enrollment for individuals from 138 to 200 percent of poverty until the state establishes a Basic Health Program (BHP). The state approved development of the BHP to protect some 55,000 Medicaid members in this population who would likely lose coverage after the end of the public health emergency. The federal comment period is open until December 30. Read More
Oregon Announces 30 Percent Pay Increase for Medicaid Behavioral Health Providers. The Portland Business Journal reported on November 16, 2022, that the Oregon Health Authority announced an average 30 percent pay increase for Medicaid behavioral health providers in fee-for-service and through coordinated care organizations. Providers serving children requiring intensive psychiatric treatment will receive the highest rate increases at 37 percent. Read More
Oregon Per Person Medicaid Costs Grew 32 Percent from 2013-19, Report Finds. The Oregon Health Authority reported in November 2022, that Medicaid costs grew by about 32 percent per person from 2013 to 2019, according to the state’s Health Care Cost Trends: Price and Utilization report. The report also found that per person Medicare Advantage costs grew by almost 58 percent during the same time period. Cost growth in both Medicaid and Medicare Advantage was mostly driven by a rise utilization. Read More
Tennessee
Tennessee Expects 350,000 Medicaid Members to Lose Coverage After Public Health Emergency Ends. WPLN News reported on November 27, 2022, that Tennessee anticipates roughly 350,000 Medicaid enrollees will lose coverage when the federal public health emergency (PHE) is lifted. The state has set up a PHE unwinding website to assist with the Medicaid redetermination process. Read More
Tennessee to Cover Comprehensive Dental Benefits for Medicaid Enrollees in 2023. WPLN News reported on November 21, 2022, that Tennessee will cover comprehensive dental benefits for Medicaid enrollees, beginning January 1, 2023. The change will impact about 600,000 adult Medicaid beneficiaries. Read More
Utah
Utah Legislature Considers Bill to Extend Postpartum Medicaid Coverage from 60 Days to 12 Months. State of Reform reported on November 28, 2022, that the Utah legislature is considering a bill to extend postpartum Medicaid coverage from 60 days to 12 months. Other Medicaid-related bills would raise the eligibility threshold for pregnant women from 144 to 200 percent of poverty, extend Medicaid and Children’s Health Insurance Program eligibility to all children, expand dental services for adults, and expand access to doula services. Read More
Wisconsin
Wisconsin Increases Medicaid Nursing Home Rates to 91 Percent of Costs in Fiscal 2023. The Wisconsin Department of Health Services announced on November 16, 2022, that Medicaid payment rates for nursing homes will increase from 77 percent of costs in fiscal 2022 to 91 percent in fiscal 2023. A significant portion of will go toward direct care nursing and to workforce wages and benefits. Read More
West Virginia
West Virginia to Investigate Fraud in CHIP. West Virginia Public Broadcasting reported on November 29, 2022, that the West Virginia Medicaid Fraud Control Unit will begin investigating potential fraud in the state Children’s Health Insurance Program (CHIP), according to Attorney General Patrick Morrisey. The state has increased the average amount of civil fraud recoveries per year by 268 percent since 2019. Read More
West Virginia Medicaid Plan Names Jason Landers President. Becker’s Payer Issues reported on November 21, 2022, that Jason Landers was named president of Highmark Health Options, the Medicaid division of Highmark Blue Cross Blue Shield West Virginia. Landers previously served as senior vice president of Medicaid at The Health Plan of West Virginia. Read More
Wyoming
Wyoming Joint Legislative Committee Advances Medicaid Expansion Legislation. The Cowboy State Daily reported on November 22, 2022, that the Wyoming Legislature Joint Revenue Committee advanced a Medicaid expansion bill, which would impact about 19,000 adults. This is the eighth Medicaid expansion bill brought before the state legislature in the past two years. Read More
National
CMS Reports $70 Million in Medicare Savings Through Direct Contracting Model in 2021. Fierce Healthcare reported on November 29, 2022, that Medicare saved $70 million in 2021 through its direct contracting model, which pays providers population-based capitated rates, according to data from the Centers for Medicare & Medicaid Services (CMS). The savings were generated by 53 organizations from April through December 2021, with 38 organizations earning $47 million in shared savings. The model has been revamped to address health equity and will transition to the Accountable Care Organization Realizing Equity, Access and Community Health Model in 2023. Read More
CDC Awards Grants Topping $3 Billion to Support Public Health Workforce. Reuters reported on November 29, 2022, that the Centers for Disease Control and Prevention (CDC) is awarding more than $3 billion to state, local, and territory health departments to support public health workforce and infrastructure. Read More
Federal Regulators Propose Rule Aimed At Improving Care Coordination for Substance Use Disorder. Behavioral Health Business reported on November 28, 2022, that federal regulators have proposed a rule aimed at increasing substance use disorder (SUD) care coordination. The change would allow patients to sign a single release for future use of their medical records by providers, while limiting the disclosure of substance use disorder records in court proceedings. The rule is proposed by the U.S. Department of Health and Human Services and the Substance Abuse and Mental Health Services Administration. Read More
Federal Regulators Propose Rule Aimed At Improving Care Coordination for Substance Use Disorder. Behavioral Health Business reported on November 28, 2022, that federal regulators have proposed a rule aimed at increasing substance use disorder (SUD) care coordination. The change would allow patients to sign a single release for future use of their medical records by providers, while limiting the disclosure of substance use disorder records in court proceedings. The rule is proposed by the U.S. Department of Health and Human Services and the Substance Abuse and Mental Health Services Administration. Read More
Roughly 656,000 Are On Medicaid HCBS Waiting Lists Nationwide, KFF Finds. The Kaiser Family Foundation (KFF) reported on November 28, 2022, that roughly 656,000 individuals nationwide were on waiting lists for Medicaid home and community-based services (HCBS) in 2021. KFF also reported that states are increasing HCBS provider payment rates in response to workforce challenges. Read More
Federal Exchange Enrollment Is Up 17 Percent. The Associated Press reported on November 22, 2022, that nearly 3.4 million people have signed up for health insurance through the federal Exchange, a 17 percent increase compared to a year ago. The increase is driven by enhanced subsidies, which were extended through 2025. Read More
Medicaid Directors Call For 4 Months Notice Before End of Public Health Emergency. McKnight’s Long-Term Care News reported on November 22, 2022, that the National Association of Medicaid Directors (NAMD) is urging Congress to give four months notice before the end of the public health emergency (PHE). NAMD, which made the request in a letter to lawmakers, is also seeking a guarantee that federal guidance on the redetermination period will not change and there will be a continuation of enhanced Medicaid matching funds through the first quarter of redeterminations. Read More
DOJ Readies Appeal Aimed at Blocking UnitedHealth, Change Healthcare Merger. Fierce Healthcare reported on November 21, 2022, that the U.S. Department of Justice (DOJ) has filed a notice of appeal to block the merger of UnitedHealth/Optum and Change Healthcare. New York and Minnesota are expected to join the challenge. The companies completed their merger on October 3, 2022, after a federal judge approved the deal. Read More
Medicare Advantage Plans Overbilled Government by More Than $1,000 Per Patient Per Year, Audits Find. Kaiser Health News (KHN) reported on November 21, 2022, that federal audits show Medicare Advantage (MA) plans overbilled the federal government by an average of more than $1,000 per patient per year from 2011 to 2013. The findings are based on 90 audits encompassing 18,090 MA members. The Centers for Medicare & Medicaid Services has said that it plans to recoup roughly $650 million from MA plans based on extrapolating audit results, pending the release of final extrapolation rules. Read More
90 Percent of Medicaid FFS Claims Are Adequately Documented by Reviewers, OIG Audit Finds. The U.S. Health and Human Services Office of the Inspector General (OIG) reported on November 19, 2022, that 90 percent of a sample of 1,653 Medicaid fee-for-service claims were adequately documented by contractors in 2019 under the Payment Error Rate Measurement (PERM) Program. The remaining 10 percent represented an estimated $6,411 in payments. Read More
62 Percent of Adults with Family Medicaid Enrollment Are Unaware of Upcoming Medicaid Eligibility Redeterminations, Report Says. Fierce Healthcare reported on November 17, 2022, that 62 percent of adults with family Medicaid enrollment know nothing about Medicaid eligibility redeterminations that will follow the end of the public health emergency, according to a report from the Robert Wood Johnson Foundation and the Urban Institute. The report used survey data from June 2022. Read More
Bipartisan Bill Would Allow PACE Enrollees to Select Standalone Part D Coverage. Fierce Healthcare reported on November 16, 2022, that Senators Bill Cassidy (R-Louisiana) and Tom Carper (D-Delaware) introduced legislation that would allow members of Program of All-Inclusive Care for the Elderly (PACE) plans to enroll in standalone Medicare Part D plans. Currently, PACE enrollees must select the program’s Part D offering. The move is aimed at lowering Part D premiums for PACE members. Read More