LANSING, MICHIGAN – Health Management Associates (HMA) announced today that Donna Checkett, current Aetna vice president for Medicaid growth, will join the independent national healthcare research and consulting firm as vice president of business development on Feb. 6. Checkett will lead new business strategy for HMA.
338 Results found.

Michigan Medicaid Managed Care Results Announced
In previous editions of The Michigan Update (most recently in August) we have reported on the Michigan Department of Health and Human Services’ (MDHHS) release of a Request for Proposals (RFP) to re-procure its Medicaid managed care contracts. The RFP was released in early May with bidder responses due in early August. This procurement is for at least five years, with the possibility of up to three one-year extensions. The total cost of the procurement for five years is estimated to be $35 billion. On October 13, 2015 the State of Michigan announced the much anticipated results of the re-procurement.
Since the prices paid to the contracted HMOs are set by the state, the health plan selection was based solely on technical scores. The HMOs were required to bid on entire regions, which were configured differently than in the past. The reconfiguration required a number of the HMOs to expand their service areas to meet the “entire region” requirement. The new regional configuration appears in the map below:
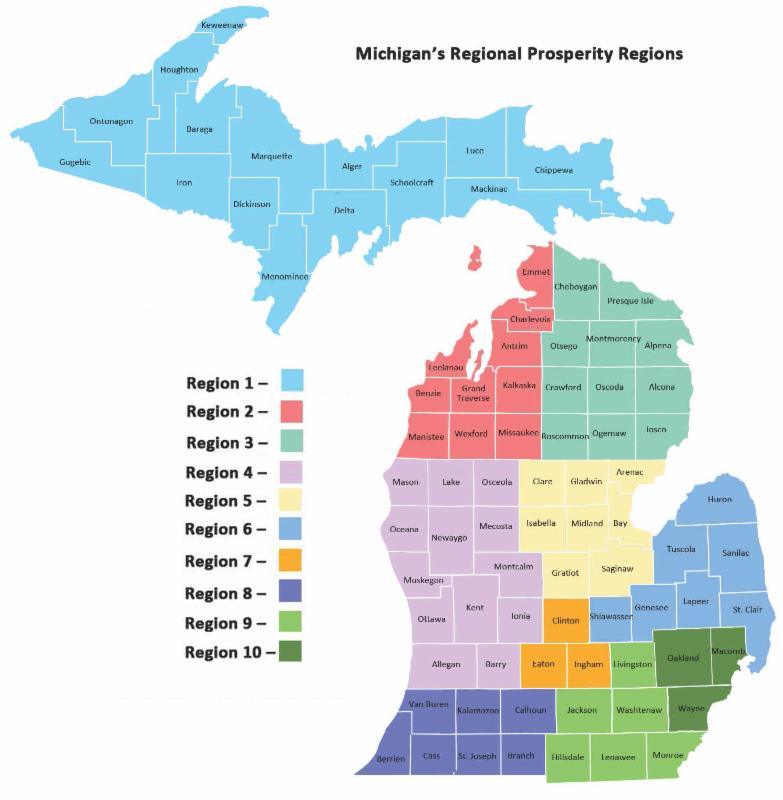
Note: Region 2 and Region 3 were required to be bid together.
The RFP included a proposed number of HMOs that would be awarded contracts for each of these regions. To minimize disruptions for Medicaid enrollees, in each region (other than the Upper Peninsula) the number of plans selected was one more than the proposed maximum number of awards for that region. Proposals from the HMOs were evaluated based on demonstrated competencies and also statements of their proposed approaches to many new initiatives related to population health, care management, behavioral health integration, patient-centered medical homes, health information technology and payment reform.
Not every HMO was successful in each region for which it submitted a bid. Two plans were not successful in any region. One is Sparrow PHP, which is an incumbent plan in Region 7. The other is MI Complete Health (Centene/Fidelis SecureCare) which is not currently a Medicaid plan in any part of the state but does have an Integrated Care Organization contract to serve dual Medicare/Medicaid enrollees in Macomb and Wayne counties as part of Michigan’s dual eligible demonstration.
The following table indicates the regions for which each bidding HMO was and was not successful. In addition, the numerical values show the rank of that plan based on their evaluation scores among the successful bidders for each region. If an HMO is a current contractor for all counties in a region, their result is shaded green. If the HMO is a current contractor for some but not all counties in a region, their result is shaded yellow. The number of Medicaid enrollees currently served in each of the regions, eligible through both “traditional” Medicaid and the Healthy Michigan Plan, appear in the bottom row on the table; across all regions, this is more than 1.6 million Medicaid enrollees.
Technical Evaluation Results
|
|
Region 1
|
Region 2
|
Region 3
|
Region 4
|
Region 5
|
Region 6
| Region 6 |
Region 8
|
Region 9
|
Region 10
|
|
Aetna Better Health
(CoventryCares)
|
|
|
|
|
No
|
|
|
Yes – 4
|
Yes – 4
|
Yes – 7
|
|
Blue Cross Complete
|
|
|
|
Yes – 3
|
|
Yes – 5
|
Yes – 3
|
|
Yes – 3
|
Yes – 5
|
|
HAP Midwest Health Plan
|
|
|
|
|
|
Yes – 6
|
|
|
No
|
No
|
|
Harbor Health
Plan
|
|
|
|
|
|
|
|
|
|
Yes – 8
|
|
McLaren Health
Plan
|
|
Yes – 3
|
Yes – 3
|
Yes – 4
|
Yes – 3
|
Yes – 3
|
Yes – 2
|
Yes – 3
|
Yes – 6
|
Yes – 4
|
|
Meridian Health Plan of MI
|
|
Yes – 1
|
Yes – 4
|
Yes – 5
|
Yes – 2
|
Yes – 4
|
No
|
Yes – 5
|
Yes – 5
|
Yes – 3
|
|
MI Complete Health
(Centene/Fidelis)
|
|
|
|
|
|
|
|
|
No
|
No
|
|
Molina Healthcare
of MI
|
|
Yes – 4
|
Yes – 1
|
Yes – 1
|
Yes – 1
|
Yes – 2
|
Yes – 1
|
Yes – 1
|
Yes – 1
|
Yes – 2
|
|
Priority Health Choice
|
|
No
|
No
|
