This week's roundup:
- In Focus: Medicaid Managed Care Spending Tops $420 Billion in 2021

- California Awards Medi-Cal Managed Care Contracts to Three Health Plans

- District of Columbia Medicaid Managed Care Contract Awards Await Mayor’s Recommendations

- Florida Medicaid Providers to Pay Long-Term Care Staff $15 Per Hour

- Illinois Enacts Legislation to Increase Nursing Home Pay

- Iowa Awards Medicaid Managed Care Contracts to Two Health Plans

- Louisiana Awards Single, Statewide PBM Contract to Magellan

- Louisiana Medicaid Begins Using State Directed Payment Model for Hospitals

- Mississippi Medicaid Managed Care Bidders File Protests

- Nebraska Delays Medicaid Managed Care Awards to September 23

- New Hampshire Releases Adult Medicaid Dental Managed Care RFP

- New York Removes Barrier to Home Care M&A Activity With New Licensure Process

- CMS Awards $98.9 Million to Navigators to Assist in 2023 Exchange Open Enrollment

- 8.8 Million Medicaid Beneficiaries Received LTSS in 2019, CMS Report Finds

- Medicare Advantage Accounts for Nearly Half of All Medicare Beneficiaries, KFF Analysis Finds

- Walgreens Boots Alliance Completes Acquisition of 55 Percent Stake in CareCentrix

In Focus
Medicaid Managed Care Spending Tops $420 Billion in 2021
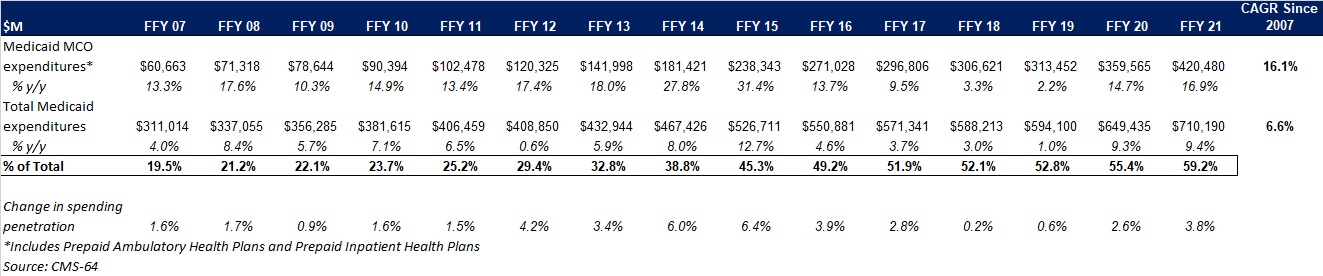
This week, our In Focus section reviews preliminary 2021 Medicaid spending data collected in the annual CMS-64 Medicaid expenditure report. After submitting a Freedom of Information Act request to the Centers for Medicare & Medicaid Services (CMS), HMA received a draft version of the CMS-64 report that is based on preliminary estimates of Medicaid spending by state for federal fiscal year (FFY) 2021. Based on the preliminary estimates, Medicaid expenditures on medical services across all 50 states and six territories in FFY 2021 was nearly $710.2 billion, with over 59 percent of the total now flowing through Medicaid managed care programs. In addition, total Medicaid spending on administrative services was $30.8 billion, bringing total program expenditures to $741 billion.
Total Medicaid Managed Care Spending
Total Medicaid managed care spending (including the federal and state share) in FFY 2021 across all 50 states and six territories was $420.5 billion, up from $359.6 billion in FFY 2020. This figure includes spending on comprehensive risk-based managed care programs as well as prepaid inpatient health plans (PIHPs) and prepaid ambulatory health plans (PAHPs). PIHPs and PAHPs refer to prepaid health plans that provide only certain services, such as dental services or behavioral health care. Fee-based programs such as primary care case management (PCCM) models are not counted in this total. Below we highlight some key observations:
- Total Medicaid managed care spending grew 16.9 percent in FFY 2021. The rate of growth has been increasing since the COVID-19 pandemic. Prior to 2020, the rate had decelerated since FFY 2016.
- Managed care spending growth was due in large part to the COVID-19 pandemic and the resulting higher Medicaid enrollment.
- In terms of dollars, the increase in Medicaid managed care spending from FFY 2020 to FFY 2021 was $60.9 billion, compared to $46.1 billion from FFY 2019 to FFY 2020.
- Medicaid managed care spending has increased at a compounded annual growth rate (CAGR) of 16.1 percent since FFY 2007, compared to a 6.6 percent growth in total Medicaid spending.
- Compared to FFY 2020, Medicaid managed care spending as a percent of total Medicaid spending in FFY 2021 increased by 3.8 percentage points to 59.2 percent.
Figure 1: Medicaid MCO Expenditures as a Percentage of Total Medicaid Expenditures FFY 2007-2021 ($M)
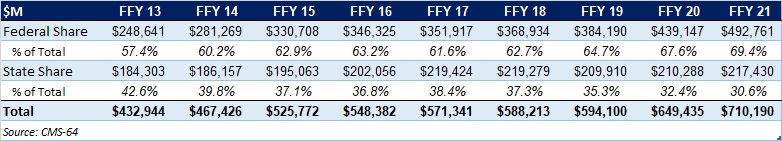
As the table below indicates, 69.4 percent of FFY 2021 spending came from federal sources, which is 12 percentage points higher than the pre-Medicaid expansion share in FFY 2013, and 1.8 percentage points higher than FFY 2020.
Figure 2: Federal vs. States Share of Medicaid Expenditures, FFY 2013-2021 ($M)
State-specific Growth Trends
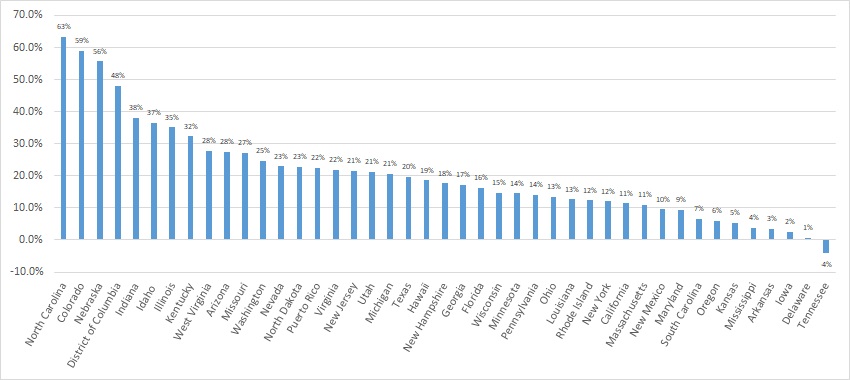
Forty-five states and territories report managed care organization (MCO) spending on the CMS-64 report, including Alaska, which utilizes a PIHP/PAHP model exclusively. Oklahoma is expected to implement a Medicaid managed care program in 2023. Of the remaining 44 states and territories that contract with risk-based MCOs, average MCO spending in FFY 2021 increased 17.6 percent. On a percentage basis, North Carolina experienced the highest year-over-year growth in Medicaid managed care spending at 63.3 percent due to the implementation of its risk-based Medicaid managed care program. Among states with more mature programs, Colorado experienced the fastest growth in FFY 2021 at 59 percent, followed by Nebraska at 55.6 percent.
The chart below provides additional detail on Medicaid managed care spending growth in states with risk-based managed care programs in FFY 2021.
Figure 3: Medicaid Managed Care Spending Growth on a Percentage Basis by State FFY 2020-21
Source: CMS-64; *Note: Not all states are included in the table.
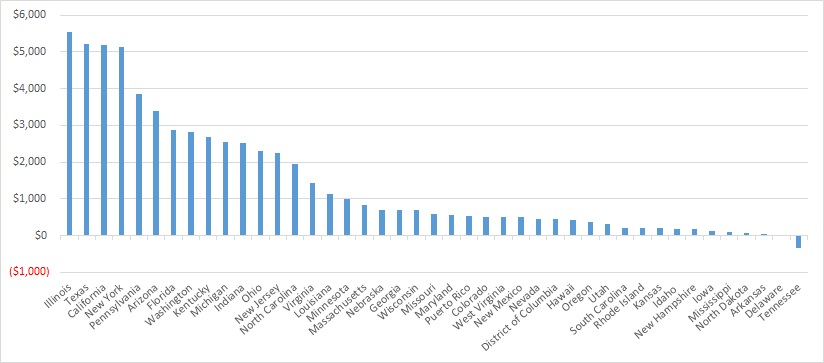
Looking at year-over-year spending growth in dollar terms, Illinois experienced the largest increase in Medicaid managed care spending at $5.5 billion. Other states with significant year-over-year spending increases in dollar terms included Texas ($5.2 billion), California ($5.2 billion), and New York ($5.1 billion). The chart below illustrates the year over year change in spending across the states.
Figure 4: Medicaid Managed Care Spending Growth on a Dollar Basis by State FFY 2020-21 ($M)
Source: CMS-64; *Note: Not all states are included in the table.
The percentage of Medicaid expenditures directed through risk-based Medicaid MCOs increased by more than five percentage points in 14 states from FFY 2020 to FFY 2021. The managed care spending penetration rate rose 13.4 percentage points in the District of Columbia, 9.7 percentage points in Indiana, 9.5 percentage points in Nebraska, 9.2 percentage points in North Carolina, and 9.1 percentage points in Illinois.
Figure 5: Medicaid MCO Expenditures as a Percentage of Total Medicaid Expenditures in States with a 5 percent or Greater Increase from FFY 2020 to FFY 2021 ($M)
Source: CMS-64
The table below ranks the states and territories by the percentage of total Medicaid spending through Medicaid MCOs. Iowa reported the highest percentage at 97.2 percent, followed by Puerto Rico at 95 percent, and Hawaii at 94.4 percent.
We note that in many states, there are certain payment mechanisms which may never be directed through managed care, such as supplemental funding sources for institutional providers and spending on retroactively eligible beneficiaries. As a result, the maximum achievable penetration rate in each state will vary and may be below that achieved in other states. The Medicaid managed care spending penetration rate is greatly influenced by the degree to which states have implemented managed long-term services and supports (MLTSS) programs.
Figure 6: Medicaid MCO Expenditures as a Percent of Total Medicaid Expenditures, FFY 2016-2021
Non-MCO Expenditures
Despite the rapid growth in Medicaid managed care over the last 10 years, program spending still represented approximately 59 percent of total Medicaid expenditures in FFY 2021. So where is the remaining fee-for-service (FFS) spending (approximately $291 billion) going? First, as noted above, there are many states/territories with Medicaid managed care programs in which certain beneficiaries or services are carved-out of the program, and these are typically associated with high-cost populations. The total amount of non-MCO spending in the 44 states with risk-based managed care in FFY 2021 was $260.4 billion. Assuming an average “full penetration” of 85 percent of total Medicaid spending, then HMA estimates that an additional $221 billion in current FFS spending could shift to a managed care model just in the states that already employ managed care for a subset of services and/or beneficiaries.
Thirteen states/territories did not utilize a comprehensive risk-based managed care model in FFY 2020. In general, the 13 states/territories that do not utilize managed care today are smaller states. Oklahoma, with $5.3 billion in Medicaid spending is expected to shift to risk-based Medicaid managed care in 2023. Total Medicaid spending across all 13 non-managed care states/territories was $29.8 billion. The 13 states/territories that did not employ a risk-based comprehensive Medicaid managed care model in FFY 2021 were Alabama, Alaska, American Samoa, Connecticut, Guam, Maine, Montana, Northern Mariana Islands, Oklahoma, South Dakota, Vermont, Virgin Islands, and Wyoming.
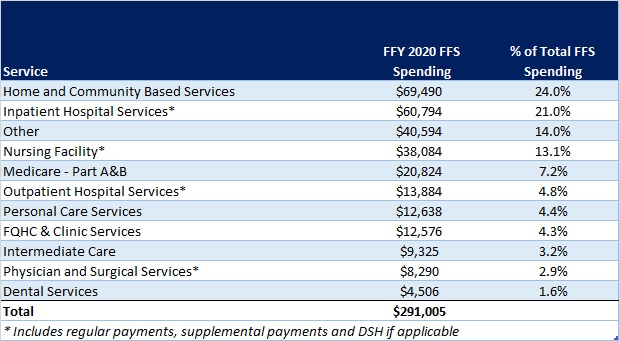
In terms of spending by service line, the largest remaining FFS category is home and community-based services at $69.5 billion, which accounts for 24 percent of FFS spending. Inpatient hospital services represent 21 percent of FFS spending at $60.8 billion.
Figure 7: Fee-for-Service Medicaid Expenditures by Service Line, FFY 2021
While the CMS-64 report provides valuable detail by service line for all FFS expenditures, it does not capture how spending directed to Medicaid MCOs is allocated by category of service. Therefore, it is not possible to calculate total MCO spending by service line, a challenge that will only intensify as more spending runs through MCOs.
HMA Roundup
California
California Awards Medi-Cal Managed Care Contracts to Three Health Plans. The California Department of Health Care Services announced on August 25, 2022, its intent to award contracts for the state’s Medi-Cal managed care program to Anthem/Blue Cross of California Partnership Plan, Centene/Health Net Community Solutions, and Molina Healthcare of California. Contracts will run from January 1, 2024, through December 31, 2028. The awards can be appealed through September 1, 2022. Read More
Centene Plans to Appeal CA Medi-Cal Managed Care Awards. Centene Corporation announced on August 25, 2022, that it will appeal the California Medi-Cal managed care awards after its Health Net plan failed to win contracts in Los Angeles, Sacramento and Kern counties. Health Net was awarded contracts in Amador, Calaveras, Inyo, Mono, San Diego, San Joaquin, Stanislaus, Tulare, Tuolumne counties. Health Net has been serving California for 25 years. Read More
Community Health Group to Protest Medicaid Managed Care Awards. Health Payer Specialist reported on August 29, 2022, that Community Health Group has begun the process of protesting California’s recently awarded Medi-Cal managed care contracts. Community Health, an incumbent plan in San Diego County, was not awarded a new contract. Read More
Blue Shield of California to Appeal Medi-Cal Managed Care Awards. Blue Shield of California Promise Health Plan announced on August 30, 2022, that it plans to appeal the California Medi-Cal managed care awards after failing to win a contract. Blue Shield of California has been serving Medi-Cal beneficiaries in San Diego and Los Angeles counties for more than 25 years. Read More
District of Columbia
Medicaid Managed Care Contract Awards Await Mayor’s Recommendations. The Washington Informer reported on August 24, 2022, that the fate of the District of Columbia’s Medicaid managed care contract awards is waiting for District of Columbia Mayor Muriel Bowser to submit formal recommendations to the DC Council for approval. The bids submitted by AmeriHealth Caritas and Anthem/Amerigroup have been accepted for potential contract awards. Other bidders are CareFirst Blue Cross Blue Shield Community Health Plan and MedStar Family Choice. CareFirst, MedStar, and AmeriHealth have all taken the procurement process to the Contract Appeals Board for review. The Medicaid managed care contracts are worth about $3 billion and serve approximately 230,000 residents. Read More
Florida
Medicaid Providers to Pay Long-Term Care Staff $15 Per Hour. Florida Politics reported on August 30, 2022, that the Florida legislature has appropriated $600 million to increase hourly wages to $15 for Medicaid long-term care providers in nursing homes and intermediate care facilities by October 1. The rate applies to both fee-for-service and managed care covered services. Effective January 1, 2023, direct care workers who are not paid the $15 minimum hourly wage may file a lawsuit against their employer. Read More
Illinois
Illinois Enacts Legislation to Increase Nursing Home Pay. WGN reported on August 29, 2022, that Illinois Governor JB Pritzker signed legislation directing more than $700 million annually to increase pay at nursing homes. Certified Nursing Assistants can receive pay increases of up to $6.50 per hour over six years. Read More
Iowa
Iowa Awards Medicaid Managed Care Contracts to Two Health Plans. The Iowa Department of Human Services announced on August 31, 2022, its intent to award Medicaid managed care contracts for Iowa Health Link, the state’s Medicaid managed care program consisting of traditional Medicaid, Iowa Health and Wellness Plan, and Children’s Health Insurance Program (known as Healthy and Well Kids in Iowa (Hawki)), to Anthem/Amerigroup and Molina Healthcare. CVS/Aetna Better Health, CareSource, and UCare also submitted bids. Centene/Iowa Total Care will continue to serve the Medicaid population but did not need to participate in the RFP process because its contract runs through June 30, 2023, with one two-year option. Contract implementation is scheduled for July 1, 2023, and the anticipated contract length is four years, with one two-year option. Read More
Kentucky
Kentucky Announces Public Comment Period for Renewal of Acquired Brain Injury Long Term Care Waiver. The Kentucky Department for Medicaid Services announced on August 26, 2022, a public comment period for the renewal of the state’s 1915(c) Home and Community Based Services Acquired Brain Injury Long Term Care waiver, which expires in 2022. No major changes are being made to the waiver in the renewal application. A summary of the application will be available by September 2, with the public comment period running through October 2. Read More
Louisiana
Louisiana Awards Single, Statewide PBM Contract to Magellan. The Louisiana Department of Health announced on August 30, 2022, that Magellan Medicaid Administration was awarded a single, statewide pharmacy benefit management (PBM) contract serving 1.8 million Medicaid managed care enrollees that will run for three years with two one-year renewal options. The contracts were initially anticipated to be implemented on July 1, 2022. Previously, each of the state’s contracted Medicaid plans contracted with a separate PBM. MedImpact Healthcare Systems and CaremarkPCS also submitted proposals. Read More
Louisiana to Host Provider Webinars to Outline Medicaid Managed Care Changes. The Louisiana Department of Health announced on August 30, 2022, that it will host provider webinars to outline changes to the state’s Medicaid managed care contracts, effective January 2023. The webinars will be held on September 2, 7, and 15, 2022. Read More
Medicaid Begins Using State Directed Payment Model for Hospitals. KTAL News reported on August 26, 2022, that Louisiana Medicaid has begun utilizing a state directed payment model for compensating hospitals that provide care for Medicaid beneficiaries. The new model, which was approved by the Centers for Medicare & Medicaid Services, became effective on July 1, 2022. Read More
Maine
Medicaid Enrollment Tops 388,300 as of May 2022. The Maine Department of Health and Human Services reported on August 25, 2022, that 388,318 individuals were enrolled in the state’s MaineCare and CubCare Medicaid programs as of May 2022. As of July 1, 2022, there were 95,419 individuals enrolled in MaineCare Medicaid expansion. Read More
Mississippi
Medicaid Managed Care Bidders File Protests. Health Payer Specialist reported on August 24, 2022, that UnitedHealthcare and Anthem/Amerigroup Mississippi have filed protests after not being awarded contracts for Mississippi’s Medicaid managed care program. The winning bidders were Centene/Magnolia Health Plan, Molina Healthcare, and TrueCare in partnership with CareSource. The state Medicaid division will announce whether it will reconsider the awards at the next meeting of its Public Procurement Review Board. The scoring system results showed TrueCare was highest with 821 points, followed by Magnolia with 792, Molina with 726, UnitedHealthcare with 715, and Amerigroup with 710. Read More
Missouri
Missouri Submits Serious Mental Illness 1115 Waiver Application. The Missouri Department of Social Services submitted on August 8, 2022, an application for a five-year, Section 1115 waiver to reimburse institutions for mental disease for acute inpatient stays by Medicaid eligibles ages 21 to 64 with serious mental illness. The start date would be no later than October 1, 2022. The federal comment period will be open through September 30, 2022. Read More
Nebraska
Nebraska Delays Medicaid Managed Care Awards to September 23. The Nebraska Department of Health and Human Services (DHHS) announced on August 30, 2022, that it will delay its Medicaid managed care award announcement by one month to September 23, 2022, to interview each of the five bidders who responded to the state’s request for proposals. DHHS received bids from incumbents Centene/Nebraska Total Care, Anthem/Healthy Blue, and UnitedHealthcare, as well as nonincumbents Medica Community Health Plan and Molina Healthcare of Nebraska. The interviews will be conducted the week of September 12. Read More
New Hampshire
New Hampshire Releases Adult Medicaid Dental Managed Care RFP. The New Hampshire Department of Health and Human Services released on August 25, 2022, a request for proposals (RFP) for a Medicaid dental managed care organization to serve approximately 88,000 adults. The program will be implemented on April 1, 2023, and run through March 31, 2026, with an additional two-year option. Proposals are due September 30. Read More
New York
New York Removes Barrier to Home Care M&A Activity With New Licensure Process. Crain’s New York Business reported on August 30, 2022, that New York removed a barrier to merger and acquisition activity in the home care market by allowing agencies to apply for a new license following changes in ownership. The process, released by the New York State Department of Health, also outlines a pathway for new home care agencies to get licensed. New York has gone without a licensure application since 2018. Read More
Legislature Passes Bill to Limit Damages from Medicaid Billing Audits. Crain’s New York Business reported on August 25, 2022, that the New York Legislature passed a bill aimed a limiting damages from Medicaid claims audits. The bill would require the state to notify Medicaid providers if their compliance program is unsatisfactory and give them 60 days to submit a correction plan. A coalition of 45 groups sent a letter urging Governor Kathy Hochul to sign the bill. Read More
Washington
Centene Reaches $33 Million Medicaid PBM Settlement in Washington. Reuters reported on August 24, 2022, that the Washington Attorney General has reached a $33 million settlement with Centene over claims that the company failed to pass through Medicaid pharmacy rebate savings to the state. Centene owes $19 million to the state of Washington, $13 million to the federal government, and $1 million to the whistleblower who brought the lawsuit. Read More
Wyoming
Legislators to Introduce Bill to Extend Medicaid Postpartum Coverage to 12 Months. Cowboy State Daily reported on August 30, 2022, that the Wyoming joint Labor, Health and Social Services committee will move forward with drafted legislation that would expand Medicaid postpartum coverage to 12 months through a state plan amendment, after the committee voted 6-5 on the draft bill. The state currently offers 60 days of Medicaid postpartum coverage. Read More
National
Medicare Shared Savings Program Saves Medicare $1.66 Billion in 2021, CMS Says. The Centers for Medicare & Medicaid Services announced on August 30, 2022, that the Medicare Shared Savings Program saved Medicare $1.66 billion in 2021 compared to spending targets. This is the fifth consecutive year that the program has generated overall savings, according to CMS. Read More
Individuals in DE, NE Join CT Lawsuit Over Wrongful Medicaid Disenrollment. CT News Junkie reported on August 29, 2022, that disabled and elderly Medicaid members in Delaware and Nebraska have joined a lawsuit over alleged wrongful termination of Medicaid coverage and are seeking nationwide, class-action status. The original lawsuit, filed on behalf of Medicaid members in Connecticut, involves a federal rule allowing disenrollment of Medicaid members who are also enrolled in a Medicare Savings Program and certain non-citizens, which plaintiffs say violates the continuous eligibility provision of the public health emergency. Read More
CMS Awards $98.9 Million to Navigators to Assist in 2023 Exchange Open Enrollment. The Centers for Medicare & Medicaid Services (CMS) awarded on August 26, 2022, $98.9 million in grants to 59 navigator organizations for the 2023 Exchange open enrollment period. The funding includes $12.5 million to support additional outreach, education, and enrollment activities to help eligible individuals transition from Medicaid and the Children’s Health Insurance Program to the Exchange. Open enrollment for 2023 runs from November 1, 2022, through January 15, 2023. Read More
8.8 Million Medicaid Beneficiaries Received LTSS in 2019, CMS Report Finds. The Centers for Medicare & Medicaid Services (CMS) reported on August 26, 2022, that 8.8 million Medicaid beneficiaries across 51 states received long-term services and supports (LTSS) in 2019. The report, which tallied both fee-for-service and managed care members, found that 7.4 million received home and community-based services (HCBS), 1.7 million received institutional services, and 300,000 received both. Read More
Medicaid, CHIP Enrollment Approaches 89 Million, Medicare Tops 64 Million as of May 2022. The Centers for Medicare & Medicaid Services (CMS) announced on August 25, 2022, that Medicaid and Children’s Health Insurance Program (CHIP) enrollment was nearly 89 million as of May 2022, up almost 678,000 from April 2022. Medicare enrollment was 64.6 million, including 29.7 million enrolled in a Medicare Advantage plan. About 12 million were dually eligible and counted in the enrollment totals for both programs. Read More
Medicare Advantage Accounts for Nearly Half of All Medicare Beneficiaries, KFF Analysis Finds. Kaiser Family Foundation (KFF) reported on August 25, 2022, that 48 percent of eligible Medicare beneficiaries (28.4 million out of 58.6 million) are enrolled in a Medicare Advantage (MA) plan. In 2007, MA accounted for 19 percent of the entire Medicare population, KFF said. UnitedHealthcare and Humana combined account for 46 percent of all MA enrollees nationwide. Read More
Industry News
Walgreens Boots Alliance Completes Acquisition of 55 Percent Stake in CareCentrix. Walgreens Boots Alliance announced on August 31, 2022, that it completed the acquisition of a 55 percent stake in CareCentrix for approximately $330 million. CareCentrix is a home care coordination company that serves more than 19 million members nationwide. Read More
LifePoint Health to Acquire Majority Ownership Interest in Springstone. LifePoint Health announced on August 29, 2022, a definitive agreement to acquire a majority interest in the operations of Springstone, a behavioral health provider with 18 behavioral health hospitals and 35 outpatient locations across nine states. Medical Properties Trust will continue to own a majority of Springstone’s real estate as well as a minority stake in Springstone’s operating company. Read More
Cigna to Offer Exchange Plans in IN, SC, TX. Fierce Healthcare reported on August 29, 2022, that Cigna will offer Exchange plans in Indiana, South Carolina, and Texas in 2023, and expand the number of counties it offers plans in Georgia, Mississippi, and North Carolina. Read More
ChristianaCare Health System Calls off Negotiations to Purchase Crozer Health. Fierce Healthcare reported on August 24, 2022, that ChristianaCare Health System called off negotiations to purchase Prospect Medical Holdings’ Crozer Health, citing a change in the economic landscape. Crozer Health, with three hospitals and 4,000 employees, was acquired by Prospect Medical Holdings in 2016. ChristianaCare Health System signed a letter of interest in February. Read More
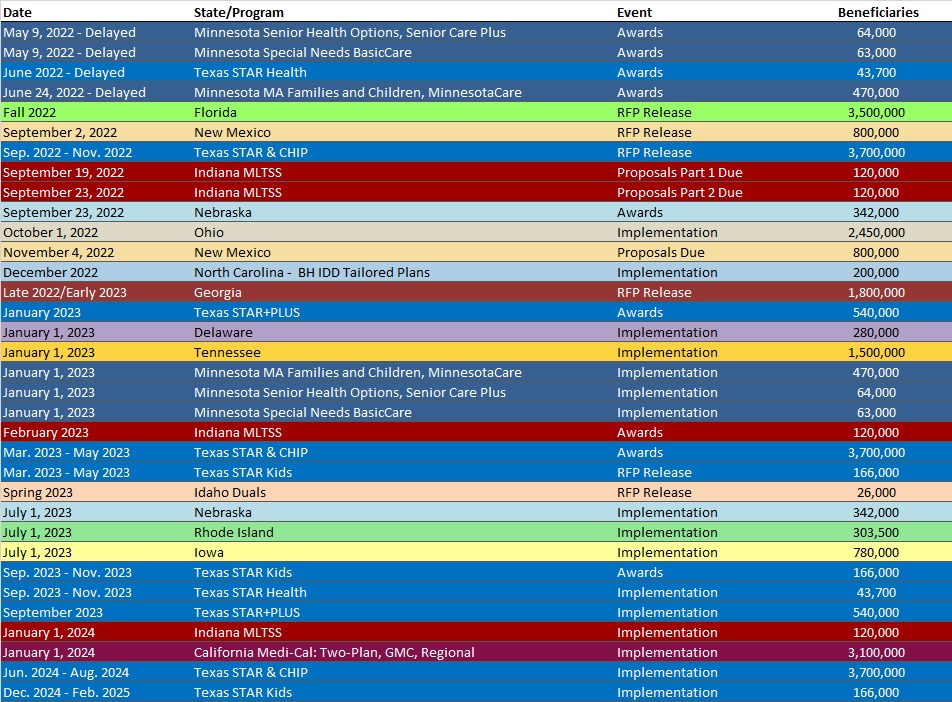
RFP Calendar
HMA News & Events
WAKELY, AN HMA COMPANY, WHITE PAPER
Demystifying the Retrospective Trend Adjustment in Direct Contracting and ACO REACH. Few aspects of CMS’s innovative Global and Professional Direct Contracting (GPDC) model have been the source of as much uncertainty and controversy as the retrospective trend adjustment. In this whitepaper, we pull back the curtains on what the retrospective trend adjustment is and how it’s calculated. We discuss why it exists, as well as the implications for GPDC participants’ benchmarks. We finish the discussion by shedding light on how recently released information by CMS may provide an indicator of what to expect for the rest of 2022 and heading into 2023. Read More
HMA WELCOMES
Lisa Braude, Principal – Boston, MA
With over 20 years of experience leading the development, implementation, and improvement of high-impact public policy, health and human services, and justice projects, Lisa Feldman Braude has advised government and not-for-profit clients on policy development and analysis and system redesign to support statewide healthcare reform initiatives.
Before joining HMA, Lisa provided consulting services related to health policy analysis and system redesign for clients at the University of Massachusetts Medical School, Commonwealth Medicine Health Law & Policy program. While there, her work included policy and project development and management, strategic planning, and data analysis for agencies and initiatives within the commonwealth.
During her career, much of her work has centered on projects that increase health equity and access to care by facilitating policy conversations across multidisciplinary stakeholder representatives and using data-driven strategies to inform decision-making.
She previously served as executive director for strategy and planning, where she provided consultancy, technical assistance, and process implementation support to senior team members in order to facilitate successful implementation and ongoing success of organizational initiatives. She also served as project director for a community hospital where she designed and implemented a program to reduce behavioral health emergency department boarding episodes.
Lisa has experience and expertise directing projects and programs as well as developing and managing grants, drafting and analyzing policy, and providing guidance and consultation to public agencies and nonprofit organizations.
She earned a doctorate in public policy from The George Washington University where she was a senior doctoral fellow with the George Washington Center for Excellence in Public Leadership. Lisa also earned a Master of Arts in sociology from Wayne State University and bachelor’s degree, also in sociology, from Oakland University.
Lisa is a Lean Six Sigma Green Belt in healthcare and has published articles and papers on evidence-based treatment, justice systems improvements, mental health and substance use disorders.
Patrick Burke, MHA, Principal – Chicago, IL
With more than 30 years of managed care experience, Pat Burke has been successful both in the provider and payor spaces. The foundation of his experience is provider network contracting for Medicare Advantage, managed Medicaid and commercial lines of business.
Pat’s experience includes managing operations of a large fully delegated physician-hospital organization (PHO) in the Chicago market, directing a medical economics team supporting large full-risk arrangements, and independent consulting supporting provider managed care contracting improvements.
Prior to joining HMA, he was chief operating officer (COO) for Meridian Health Plan in Illinois. Over a period of four and a half years as COO, Pat and the local and corporate teams successfully transitioned through two ownership changes and associated system conversions while successfully growing Medicaid membership to over 900,000. Prior to his COO role, he was vice president of network for Missouri Care where he led his team through the state-wide Medicaid expansion, successfully building the strongest provider network in advance of the 2017 implementation and resulting in Missouri Care becoming the largest Medicaid plan within the state of Missouri.
Pat earned a Master of Health Administration from St. Louis University and a bachelor’s degree from the University of Missouri, Columbia.
Samantha Lang, Senior Consultant – New York, NY
Samantha Lang is an experienced public health professional with more than 10 years of experience conducting research, outreach, and providing organizational support. She has practical knowledge of health policy, harm reduction, and the criminal-legal system and is passionate about promoting health equity and patient autonomy.
During her career she has worked in behavioral, reproductive, homecare, senior, and low-income health service environments. She has extensive experience in qualitative research and data collection, policy analysis, outreach and project management.
Before joining HMA, Samantha served as both a research coordinator and a program manager for the HEALing Communities Study based out of Columbia University, a National Institute on Drug Abuse-funded study with the goal of reducing opioid overdose fatalities in 67 communities by 40% in three years. While there, she provided organizational support to community coalitions working to implement study interventions, and project management for the Columbia research team.
Samantha has worked with stakeholders across the substance use disorder sector, from consumers to providers and policy makers. Samantha has also worked with the Health Home program as a patient intake coordinator, and as a research assistant for Gynuity Health Projects with a focus on reproductive healthcare. Her other areas of focus include justice-involved care, health equity work, and projects related to social determinants of health.
Samantha earned a Bachelor of Arts degree from Wesleyan University where she majored in English. She also earned a Master of Public Health from The City University of New York School of Public Health with a concentration in health policy and management.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Maryland Medicaid Managed Care Enrollment Is Up 2.7%, May-22 Data
- Mississippi Medicaid Managed Care Enrollment is Down 11.1%, Jul-22 Data
- Missouri Medicaid Managed Care Enrollment is Up 10.7%, May-22 Data
- New Jersey Medicaid Managed Care Enrollment is Up 2.9%, May-22 Data
- Oklahoma Medicaid Enrollment is Up 4.8%, Apr-22 Data
- Oklahoma Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
Medicaid Financials and Utilization Data:
- MLRs at Mississippi Medicaid MCOs Average 85%, 2021 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- California Medi-Cal Managed Care RFP: Two-Plan, GMC, and Regional Models Proposals, Evaluation, Awards, Aug-22
- Iowa Health Link RFP, Scoring, Awards, and Related Documents, 2022
- Mississippi Pharmacy PDL, Supplemental Rebate, Rate Setting and Programmatic Review and Assessment of Core Components RFP, Award, and Related Documents, 2021-22
- Mississippi Support and Hosting of the Medicaid Eligibility System RFP and Related Documents, 2022
Medicaid Program Reports, Data, and Updates:
- Colorado Medicaid HEDIS Reports, 2013-21
- District of Columbia Medicaid Managed Care Performance Reports, 2019-21
- Idaho Medicaid Facts, Figures, and Trends Reports, 2013-22
- Louisiana CHIP Annual Reports, SFY 2010-21
- Maryland Medicaid Dental Program Chartbook CY 2016-20, Jun-22
- Missouri Section 1115 Serious Mental Illness Waiver Application, Jul-22
- Nebraska DHHS Division of Behavioral Health Annual Reports, FY 2013-21
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.