HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Bolstering the Youth Behavioral Health System: Innovative State Policies to Address Access & Parity

- California Releases Mobile Crisis Intervention Services RFI

- California Exchange Plans Must Resubmit 2023 Rates to Reflect Impact of Inflation Reduction Act

- Florida Medicaid Enrollment to Increase 5.5 Percent, Surplus to Top $1.25 Billion in Fiscal 2023

- Georgia Can Reinstate Medicaid Expansion Work Requirements, Federal Judge Rules

- Nebraska Awards Maxmius Contract for MMIS Provider Services Module

- New York Legislators Introduce Bill to Ease Burden of Medicaid Provider Audits, Recoveries

- North Carolina Healthy Opportunities Pilot Struggles to Gain Traction

- Ohio Counties Win $600 Million in Damages in Opioid Lawsuit

- Oregon Health Plan to Use Tech Platform to Connect Medicaid Members to Social Services

- Texas Dual Eligible Demonstration Shows Cost Reductions, Study Finds

- Utah Releases Medicaid Dental Managed Care RFP

- U.S. Senate Panel Investigates Medicare Advantage, Part D Marketing Tactics

- Sonas Home Health Care Acquires Focus Forward Skilled Care

- Wakely, An HMA Company, White Paper: 2021 Supplemental Claims Impact

In Focus
Bolstering the Youth Behavioral Health System: Innovative State Policies to Address Access & Parity
This week, our In Focus section highlights an HMA Issue Brief, Bolstering the Youth Behavioral Health System: Innovative State Policies to Address Access & Parity, published in August 2022. The brief examines policies aiming to advance access and availability of behavioral health services (encompassing mental health and substance use disorders) for youth. Below we explore opportunities for states to adopt levers to ensure access to the full continuum of children’s behavioral health services. States should consider developing a multi-faceted strategy to address accessibility issues including:
- A policy mechanism for insurance coverage and funding for infrastructure, support and services across behavioral health, child welfare and Medicaid
- A robust delivery system for provision of services
- Comprehensive benefit design
- A mechanism to monitor network adequacy, access, and parity
The COVID-19 pandemic has exacerbated rates of depression, anxiety, and other behavioral health issues among youth – with suicide now the second leading cause of death among ages 10-12. Pre-pandemic, 1 in 5 children experienced a mental health condition every year and only 54 percent of non-institutionalized youth enrolled in Medicaid or CHIP received mental health treatment. Between March 2020 to October 2020, mental health–related emergency department visits increased 24 percent among youth ages 5 to 11 and 31 percent among ages 12 to 17, compared with 2019 emergency department visits.
Youth covered by Medicaid and the State Children’s Health Insurance Program (CHIP), and the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) of the Medicaid Act require state Medicaid agencies to provide enrollees under age 21 with access to periodic and preventive screenings, and services that are necessary to “correct or ameliorate” medical conditions, including other additional health care services such as behavioral health conditions. It remains the responsibility of states to determine medical necessity on a case by-case basis. As of 2020, states are mandated to submit a CHIP state plan amendment to demonstrate compliance with the new behavioral health coverage provisions. However, behavioral health services are not a specifically defined category of benefits in federal Medicaid law and coverage of many services is at state discretion. The 2008 Mental Health Parity and Equity Act (MHPAEA) requires that Medicaid managed care and private health insurers who do reimburse for behavioral health services provide behavioral health benefits to cover mental health and substance use services that is no more restrictive than the coverage generally available for medical and surgical benefits. While MHPAEA was designed to reduce inequities in coverage between behavioral and physical health services, it does not reduce inequities in reimbursement as payers are not required to cover behavioral health services.
Ambitious efforts are underway to prioritize behavioral health services for youth. The Department of Health and Human Services (HHS) recently called for states to prioritize and maximize efforts to strengthen youth mental health. The American Academy of Pediatrics (AAP), American Academy of Child and Adolescent Psychiatry (AACAP) and Children’s Hospital Association declared a national emergency in children’s mental health. In addition, passage of the Bipartisan Safer Communities legislation includes significant funding for mental health screening, expansion of community behavioral health center (CCBHC) model; improving access to mental health services for children, youth, and families through the Medicaid program and CHIP; increasing access to mental health services for youth and families in crisis via telehealth; and investments to expand provider training in mental health, supporting suicide prevention, crisis and trauma intervention, and recovery.
Click here to read the Issue Brief.
For questions, please contact:
Caitlin Thomas-Henkel
Uma Ahluwalia
Devon Schechinger
Debbi Witham
HMA Roundup
California
California Releases Mobile Crisis Intervention Services RFI. Open Minds reported on August 23, 2022, that the California Department of Health Care Services released a request for information (RFI) regarding implementation of community-based mobile crisis intervention services for Medicaid enrollees experiencing substance use disorder or mental health crises. Implementation is expected to begin January 2023, following submission of a Medi-Cal state plan amendment. RFI responses will be accepted until September 2, 2022. Read More
California Extends Medicaid Coverage to Immigrants Over Age 25 Through 2023. KCRA reported on August 22, 2022, that California will extend Medicaid coverage to low-income adults aged 26 and older, regardless of immigration status, through the end of 2023. The policy, announced by Governor Gavin Newsom, will act as bridge until a new law takes effect in January 2024 offering Medicaid coverage to this population. California already covers individuals aged 25 and under, regardless of immigration status. Read More
Exchange Plans Must Resubmit 2023 Rates to Reflect Impact of Inflation Reduction Act. Health Payer Specialist reported on August 19, 2022, that the Covered California Exchange asked health plans to resubmit 2023 rates to take into consideration the impact of the Inflation Reduction Act, which continues enhanced premium subsidies. Initial premium submissions indicated a six percent increase for 2023, or about 100 basis points higher than without the continuation of enhanced subsidies. Read More
Medicaid Plan, Providers to Pay $70.7 Million to Resolve False Claims Allegations. The U.S. Department of Justice announced on August 18, 2022, that Ventura County Medi-Cal Managed Care Commission (doing business as Gold Coast Health Plan) and three healthcare providers have agreed to pay a total of $70.7 million to settle alleged false claims submissions in 2014 and 2015. The providers are Ventura County/Ventura County Medical Center, Dignity Health, and Clinicas del Camino Real. Read More
Florida
Medicaid Enrollment to Increase 5.5 Percent, Surplus to Top $1.25 Billion in Fiscal 2023. Florida Politics reported on August 22, 2022, that Florida Medicaid enrollment is projected to increase 5.5 percent to 5.36 million in fiscal 2023, assuming continuation of the public health emergency, according to the state’s Social Services Estimating Conference. The state is also expected to end fiscal 2023 with a surplus of more than $1.25 billion in Medicaid general funds. Assuming the public health emergency ends in fiscal 2023, the forecast predicts Medicaid enrollment will decrease by 7.1 percent in fiscal 2024. Read More
Georgia
Georgia Can Reinstate Medicaid Expansion Work Requirements, Federal Judge Rules. The Associated Press reported on August 20, 2022, that a federal judge reinstated work requirements for Georgia’s Medicaid expansion demonstration, known as Pathways to Coverage. The Biden administration revoked approval of the work requirements in December 2021, and the state filed a lawsuit to reinstate them in January 2022. There are an estimated 50,000 uninsured Georgians who would be eligible for the demonstration in the first two years. Georgia Governor Brian Kemp has said full Medicaid expansion would cost the state too much money. Read More
Nebraska
Health Plan Contributes $500,000 to Local Organizations Addressing Social Issues in Nebraska. Medica announced on August 18, 2022, it has allocated $500,000 to organizations in Nebraska that address social issues including child and maternal health, education and workforce development, health equity, foster youth, health and housing, and tribal organizations. Read More
Nebraska Awards Maxmius Contract for MMIS Provider Services Module. Maximus announced on August 17, 2022, it has been awarded a contract by the Nebraska Department of Health and Human Services for the state’s Medicaid Management Information System (MMIS) provider module. Maximus, which was selected by the National Association of State Procurement Officers ValuePoint for an MMIS-Provider Services Module Master Services Agreement, has partnered with Nebraska since 2015. The new contract will run for six years. Read More
Nevada
Nevada Committee Approves Use of ARPA Funding to Expand Mental Health Services for Children. The Nevada Appeal reported on August 17, 2022, that the Nevada Interim Finance Committee unanimously approved the use of American Rescue Plan Act (ARPA) funding to expand mental health services for children in the state. After 2025, when the federal funds run out, it will cost the state $28 million per year to continue the services. Read More
New York
New York Finds John Hancock Prematurely Terminated Long-Term Care Coverage for Some Members. New York announced on August 18, 2022, that John Hancock Life & Health Insurance Company will return $21.6 million to consumers and $2.2 million to the state Medicaid program for prematurely terminating coverage for certain members between February 2001 and July 2019. John Hancock will also pay a $2.5 million dollar penalty. Read More
Legislators Introduce Bill to Ease Burden of Medicaid Provider Audits, Recoveries. Spectrum News reported on August 18, 2022, that New York Senator Peter Hackman (D-Peekskill) and Assemblyman Richard Gottfried (D-Manhattan) introduced legislation to ease the burden of Medicaid provider audits and recoveries, which in some cases have resulted in large fines for clerical errors even when no fraud of abuse was found. The bill would give providers two months to address non-compliance issues before recovering overpayments. The bill would also prevent repeat reviews or audits within three years, unless new information is brought forward. Read More
North Carolina
North Carolina Selects KPMG, Red Hat Platform to Integrate Medicaid Software Systems. KPMG announced on August 17, 2022, that North Carolina will use a technology platform from KPMG and Red Hat to help integrate the state’s various Medicaid software systems. Read More
Healthy Opportunities Pilot Struggles to Gain Traction. The Mountaineer reported on August 18, 2022, that the North Carolina Healthy Opportunities Pilot, which is using $650 million in Medicaid funds to address social determinants of health, has struggled to gain traction in areas beyond providing free food. Aspects of the programs that have been delayed or face problems include attempts to address domestic violence and affordable housing. The program covers at least 29 interventions, including up to $1,250 per month in housing move-in support, $5,000 in annual home remediation services, and $150 in healthy food. Read More
Northern Mariana Islands
Northern Mariana Islands Seeks Medicaid Contracts with Guam Pharmacies. The Saipan Tribune reported on August 23, 2022, that the Commonwealth of the Northern Mariana Islands (CNMI) state Medicaid agency is hoping to execute contracts with pharmacies in Guam, which currently do not accept CNMI Medicaid. The issue impacts CNMI Medicaid members seeking treatment in Guam. Read More
Ohio
Ohio Counties Win $600 Million in Damages in Opioid Lawsuit. The Associated Press reported on August 17, 2022, that Lake and Trumbull counties in Ohio were awarded $306 million and $344 million in damages, respectively, over 15 years from CVS, Walgreens and Walmart pharmacies in an opioids lawsuit, according to a ruling from U.S. District Judge Dan Polster. Pharmacy chains Rite Aid and Giant Eagle reached undisclosed settlements with the counties before trial. Read More
Oregon
Oregon Health Plan to Use Tech Platform to Connect Medicaid Members to Social Services. Trillium Community Health Plan announced on August 19, 2022, that it will use the Connect Oregon technology platform to help Medicaid members connect with community organizations that address social determinants of health in Lane, western Linn, western Douglas, Clackamas, Multnomah, and Washington counties. Connect Oregon is powered by technology company Unite Us. Read More
Pennsylvania
Pennsylvania Sees Number of Medicaid Dentists Decrease by 13.5 Percent in 2020, Report Finds. Pennsylvania News reported on August 21, 2022, that Pennsylvania has seen a 13.5 percent decrease in dentists serving Medicaid from 2019 through 2020, according to a report from the Pennsylvania Coalition for Oral Health. During this time period, the state’s Medicaid enrollment increased by 6.6 percent. Low pay is likely a contributing factor to the decrease. Read More
Texas
Texas Dual Eligible Demonstration Shows Cost Reductions, Study Finds. Open Minds reported on August 18, 2022, that the Texas Dual Eligible Integrated Care demonstration showed a 6.6 percent reduction in per member per month (PMPM) Medicaid costs to $1,141 from 2015 to 2018, according to a controlled study by RTI International. PMPM Medicare costs fell 0.33 percent to $1,492. Read More
Utah
Utah Releases Medicaid Dental Managed Care RFP. The Utah Department of Health and Human Services released on August 15, 2022, a request for proposals for two Medicaid dental managed care organizations to provide full-risk coverage through a Prepaid Ambulatory Health Plan. The awarded contracts will run for five years. The state’s current Medicaid dental contracts, held by Premier Access and MCNA, were awarded in March 2018. Read More
Wyoming
Legislators Draft Bill to Create Upper Payment Limit Program for Psychiatric Treatment Facilities. County 10 reported on August 22, 2022, that a bipartisan Wyoming legislative committee is drafting a bill to establish an upper payment limit (UPL) program with the Centers for Medicare & Medicaid Services (CMS) to increase Medicaid reimbursement for psychiatric residential treatment facilities. UPL is a supplemental payment program. Read More
National
U.S. Senate Panel Investigates Medicare Advantage, Part D Marketing Tactics. Fierce Healthcare reported on August 23, 2022, that a U.S. Senate panel is investigating whether Medicare Advantage (MA) plans engage in misleading marketing and aggressive sales tactics. Senate Finance Committee Chairman Ron Wyden (D-Oregon) has sent letters to 15 state insurance regulators seeking information on any complaints they have received regarding MA and Medicare Part D plan marketing from 2019 through 2022. Lawmakers and regulators are also looking into prior authorization and risk adjustment practices. Read More
OIG to Investigate Skilled Nursing Facility Costs, Medicare Reimbursement Rates. Skilled Nursing News reported on August 23, 2022, that the U.S. Office of the Inspector General (OIG) will launch an investigation into whether skilled nursing facilities are properly reporting related-party costs, according to an update to the OIG’s 2022 work plan. The investigation will also evaluate if Medicare reimbursement rates sufficiently cover beneficiary care. Read More
CMS Awards $25 Million to States, Territories for HCBS Through Money Follows the Person. The Centers for Medicare & Medicaid Services (CMS) announced on August 22, 2022, that it has awarded a total of $25 million in grants to Illinois, Kansas, New Hampshire, American Samoa, and Puerto Rico for the Medicaid Money Follows the Person demonstration, a program aimed at helping move individuals from institutional care to home and community-based services (HCBS). Funds must be used by March 31, 2025. In total, 41 states have now received funding for the program. Read More
CMS Urges States to Tie Medicaid Payments for Nursing Homes to Quality. The Centers for Medicare & Medicaid Services (CMS) issued a bulletin on August 22, 2022, urging states to tie Medicaid payments for nursing homes to quality measures. CMS also encourages states to develop long-term solutions for training and improving staffing and workforce sustainability issues in nursing homes. Read More
Medicaid Enrollment, Spending Higher Than Expected in 2021, CBO Reports. Health Affairs reported on August 19, 2022, that Medicaid enrollment and spending was higher than expected in 2021, according to a report from the Congressional Budget Office (CBO) and the House-Senate Joint Committee on Taxation. Medicaid enrollment for individuals under age 65 was 71.6 million in 2021, compared to a CBO projection of 64 million. CBO said that spending on Exchange plans was also higher than expected, driven by enhanced Exchange subsidies. Read More
CMS Proposes Mandatory, Annual State Reporting of Certain Medicaid/CHIP Data Sets. The Centers for Medicare & Medicaid Services (CMS) proposed on August 18, 2022, that beginning in fiscal 2024, states would be required to annually report measures for three quality data sets for Medicaid and the Children’s Health Insurance Program (CHIP): children’s health, behavioral health, and health home measures. Public comments will be accepted through October 21, 2022. Read More
CMS Urges States to Strengthen Access to Behavioral Health Care for Children. The Centers for Medicare & Medicaid Services (CMS) released on August 18, 2022, a bulletin urging states to better address behavioral health by strengthening prevention and early identification, expanding provider capacity, and increasing integration of behavioral health and primary care. A second bulletin provided strategies and guidance to improve school health services. Read More
Inflation Reduction Act Further Delays Elimination of Safe Harbor Protection for Medicare Part D Rebates. Modern Healthcare reported on August 18, 2022, that the Inflation Reduction Act further delays the elimination of safe harbor protections for Medicare Part D rebates until 2032. The change, which would prevent pharmacy benefit managers from keeping Medicare Part D prescription drug rebates, was originally set to take effect in early 2021. Read More
U.S. Senators Introduce Bipartisan Bill to Expand Access to Occupational Therapy Services for Mental Health, SUD. U.S. Senator Maggie Hassan (D-NH) announced on August 17, 2022, the introduction of a bipartisan bill aimed at expanding access to occupational therapy (OT) for individuals with mental health or substance use disorders (SUD). The bill, which is co-sponsored by Senator Tim Scott (R-SC), would help address barriers preventing community-based mental health and recovery service programs from providing occupational therapy services to individuals with SUD and mental health diagnoses. Read More
Senator Urges HHS to Invalidate Rule Requiring States to Terminate Medicaid Coverage for Certain Enrollees. The Connecticut Mirror reported on August 17, 2022, that Connecticut Senate President Pro Tempore Martin Looney (D-New Haven) is urging the U.S. Department of Health and Human Services (HHS) to invalidate a rule from November 2020 that requires states to terminate Medicaid coverage for individuals also enrolled in a Medicare Savings Program and for certain non-citizens. This comes after Disability Rights Connecticut filed a federal lawsuit on behalf of three beneficiaries who claim they were wrongly disenrolled. The rule is an exemption to continuous eligibility requirements during the public health emergency. Read More
Industry News
Sonas Home Health Care Acquires Focus Forward Skilled Care. The Middle Market reported on August 19, 2022, that Sonas Home Health Care acquired Focus Forward Skilled Care, a pediatric home health care provider. Dak Group acted as investment banker and financial advisor to Focus Forward. Read More
Health Plan Foundation Awards $3 Million in Grants to Address Children’s Mental Health, Food Insecurity. The Cigna Foundation announced on August 18, 2022, $3 million in grant awards to organizations across 16 states to address hunger and mental health problems for children returning to school. The grants are a part of a five-year, $25 million initiative to address health issues among children. Read More
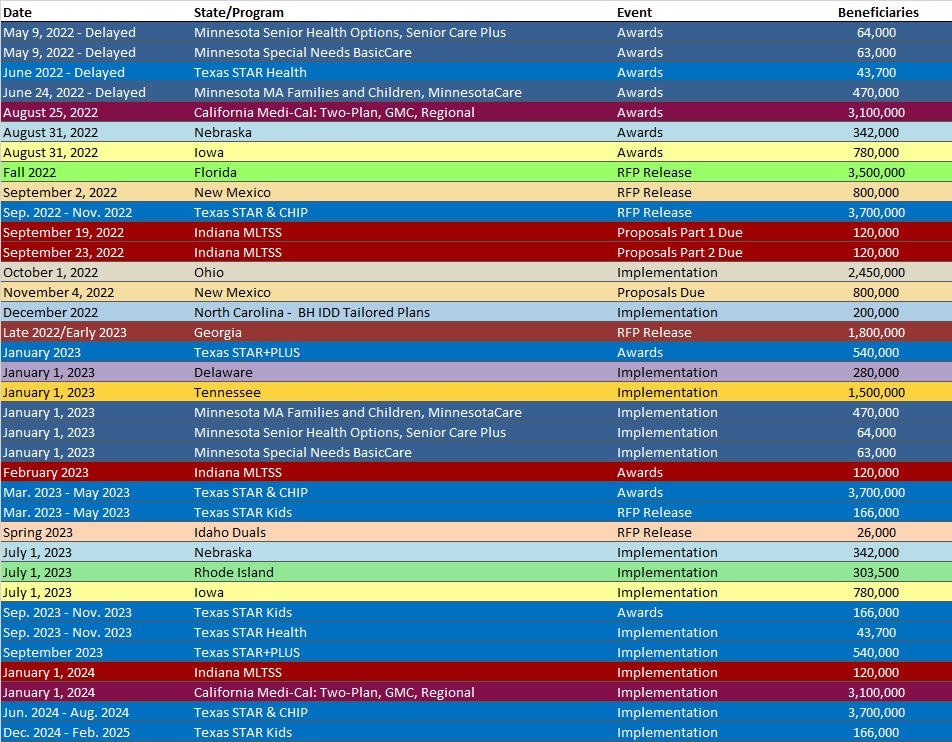
RFP Calendar
HMA News & Events
WAKELY, AN HMA COMPANY, WHITE PAPER
2021 Supplemental Claims Impact. Risk score capture and accuracy through supplemental claims continues to be an industry hot topic. Supplemental files allow issuers to ensure accurate coding for risk scoring, thus impacting risk adjustment transfers in the ACA market. In addition, supplemental files also help issuers mitigate risk adjustment data validation (RADV) audit risk for both “under-coding” and “over-coding” by correcting data within their claims system. Read More
HMA WELCOMES
Bob Kritzler, MD, Principal – Chicago, IL
An accomplished physician executive and experienced NCQA surveyor, Bob Kritzler, MD, has successfully led efforts to improve quality of care and its delivery throughout his career.
Dr. Kritzler has extensive expertise in the areas of quality and accreditation, population health, value-based care and payments, and integrated systems. His experience includes working with academic systems, establishing and improving provider-plan interfaces and advancing health equity.
Prior to joining HMA he owned and operated an independent consultancy providing a variety of services related to utilization, general management, quality, population health service, senior physician and executive mentoring and team development. His clients included payers, health systems, pharma and device companies, and employers.
As executive leader, senior medical director at Aetna Medicaid, Dr. Kritzler led teams charged with creating and implementing the inclusive population health programs for all Aetna Medicaid plans. During his time with Aetna Better Health of Illinois, he co-founded the Duals Center of Clinical Excellence and served as chief medical officer for all the duals plans in Illinois, Ohio, Michigan, and Virginia and advised the D-SNP plans.
During his career, Dr. Kritzler has led small Chicago safety net health plans (Medicaid and Medicare Advantage) to successful accreditation, spearheaded medical management strategy for the health plans owned and managed by Johns Hopkins Medicine and maintained a pediatric endocrine clinical practice. He spent more than 20 years at Kaiser Permanente Mid-Atlantic, where he had several positions including vice president for quality resource management and clinical chief operating officer of the Mid-Atlantic Permanente medical group. In that last role, he co-led the implementation of both an EMR and “advanced open access” scheduling.
Dr Kritzler served on the board, culminating as chair, at The Center for Health Value Innovation, one of the key national organizations promoting and funding value-based health plan strategy, from 2006-2014.
Dr. Kritzler earned his Bachelor of Arts from Johns Hopkins University and his Doctor of Medicine from Columbia University, College of Physicians and Surgeons. He completed his pediatric residency at Babies Hospital of New York, (now Morgan Stanley Children’s Hospital) and was a fellow in pediatric endocrinology at The Johns Hopkins University School of Medicine. He also received a certificate for completing the Kaiser Permanente-Stanford University School of Business Executive Program.
Nicole D. Lehman, Senior Consultant – Chicago, IL
Nicole D. Lehman is an experienced healthcare professional specializing in the improvement, development, and growth of multifaceted, high-paced managed care organizations.
She is an expert on implementing regulatory guidance as well as complying with state, federal, and quality audits. She has additional experience in health plan management and developing new policies.
Before joining HMA, Nicole served as the director of behavioral health services for the L.A. Health Care Plan, where she oversaw all department staff and programs including provider outreach, autism services, transgender health, and Institutes for Mental Disease. She was directly responsible for increasing growth utilization across all lines of business, including Medi-Cal/Medicaid, Medicare/Dual Eligible Special Needs Plan, and Cal MediConnect.
Prior to this, Nicole also served as the manager of behavioral health integration for CalOptima. While there, she promoted and measured improvements in health outcomes for behavioral health services.
A leader in the managed health care industry, Nicole has consistently ensured the effectiveness of departmental programs and services by establishing new reporting standards, audit criteria, and quality measures.
Nicole earned an undergraduate degree in psychology from California State University, Fullerton. She completed her Master of Social Work at the University of Southern California.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Alaska Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Arizona Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Kentucky Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Maine Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Massachusetts Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Michigan Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Minnesota Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Mississippi Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Missouri Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Montana Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Nebraska Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- New Jersey Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Ohio Medicaid Fee for Service vs. Managed Care Penetration, 2014-21
- Washington Medicaid Managed Care Enrollment is Up 1.8%, Apr-22 Data
Medicaid Financials and Utilization Data
- MLRs at 10 New York Medicaid MCOs Average 90.3%, 2021 Data
- MLRs Average 89% at Oregon Medicaid MCOs, 2021 Data
- MLRs Average 86.8% at South Carolina Medicaid MCOs, 2021 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- California Mobile Crisis Intervention Services RFI
- Idaho Behavioral Health Plan Optum Contract and Proposal, 2013-21
- Utah Medicaid Dental Services RFP, Aug-22
Medicaid Program Reports, Data, and Updates:
- Florida Medicaid Managed Care HEDIS Scores, 2012-20
- Idaho Medicaid Dental External Quality Reviews, 2019-21
- Idaho Medicaid IBHP External Quality Review Reports, FY 2019-21
- New Jersey Medical Assistance Advisory Council Meeting Materials, Jul-22
- New York Medicaid Pharmacy Managed Care to FFS Transition Presentations, Aug-22
- Oklahoma Health Care Authority Annual Reports, 2014-21
- Texas Benchmarks for Managed Care Organizations Report, Aug-22
- Tennessee Medicaid Quality Assessment and Performance Improvement Strategy Reports, 2013-21
- West Virginia Medicaid Mountain Health Trust Annual Reports, SFY 2011-21
- West Virginia Medicaid Mountain Health Trust EQR Reports, 2009-21
- West Virginia Medical Services Fund Advisory Council Meeting Materials, Feb-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
