This week's roundup:
- In Focus: What You Need to Know about CMS’s Proposed Changes to Medicaid Managed Care Rules

- Alabama Releases Integrated Care Network Program RFP

- Arkansas Proposes Medicaid Work Requirements for Expansion Program

- Florida Legislature Passes Bill to Regulate PBMs

- Florida House Passes Bill to Create Pilot Program Providing Medicaid Managed Care Coverage to Individuals with IDD

- Georgia Enacts Law to Create State-based Insurance Exchange

- Louisiana Candidates for Governor Promise to Keep Medicaid Expansion

- Mississippi Medicaid Beneficiaries Are No Longer Responsible for Copays

- Nevada Expands Dental Services for Medicaid Beneficiaries with IDD

- Nevada Releases Baseline Medicaid Enrollment Report Ahead of Redeterminations

- New York to Gradually Redirect Medicaid Funding from Counties

- Tennessee Medicaid to Cover Cost of Diapers for First Two Years

- Washington Publishes Plan to Remove Barriers to Access for Health, Human Services Benefits

- Medicare Advantage Enrollment Surpasses Traditional Medicare in January

- Centene to Sell Apixio to New Mountain Capital

- BCBS-MI, BCBS-VT to Pursue Affiliation

In Focus
What You Need to Know about CMS’s Proposed Changes to Medicaid Managed Care Rules
This week, our In Focus section reviews CMS’s proposed changes to the federal Medicaid managed care access, finance, and quality regulation (CMS-2439-P). A future In Focus will take a closer look at the proposed changes to the federal Medicaid access to care regulation (CMS-2442-P), which also has significant implications for state Medicaid programs.
On April 28, 2023, the Centers for Medicare & Medicaid Services (CMS) unveiled two significant and related proposed rules addressing Medicaid managed care access, finance, and quality requirements. Together these proposed rules signal a new era of accountability and transparency in the Medicaid program. They also strengthen beneficiaries’ role in influencing the policies and administration of state Medicaid programs.
Table 1 identifies a few of the key themes and issues addressed in the Medicaid managed care proposed rule. The deadline for submitting comments to CMS is July 3, 2023.
Table 1. Medicaid Managed Care Proposed Rule: Snapshot of Proposed Changes
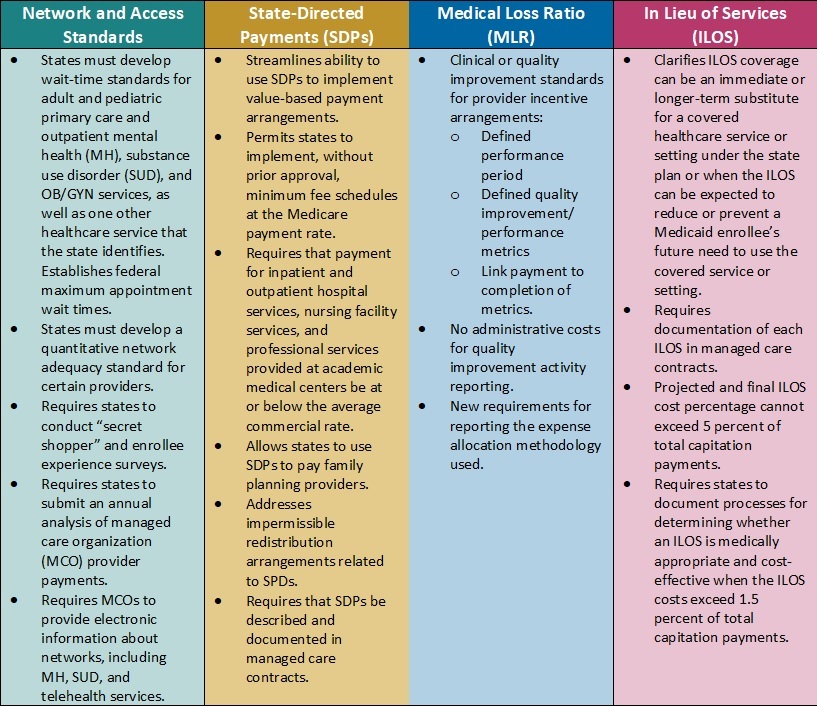
Key Themes and Considerations
Payment Ceilings May Accelerate Value-Based Payment Arrangements. Current federal regulations allow states to direct managed care organizations (MCOs) to pay providers according to specific rates or methods. States have used these directed payment arrangements to set minimum payment rates for certain types of providers or to require participation in value-based payment (VBP) initiatives.
In the proposed rule, CMS calls for establishing an upper limit for these payments. Specifically, the agency plans to limit the projected total payment rates to the average commercial rate (ACR) for inpatient and outpatient hospital services, nursing facility services, and qualified practitioner services at academic medical centers that states include in state-directed payment (SDP) arrangements. The ACR limit, in concert with the proposed SDP documentation and reporting, is among the most significant and complex proposed changes in the rule.
Considerations: The proposed changes represent a strong federal regulatory push to accelerate movement to VBP in Medicaid, which provides states with new levers to drive value in their Medicaid delivery systems. It also means that MCOs, providers, and other stakeholders will need to navigate and help inform the policies and contractual arrangements that will flow from the pending changes. For example, states may need to reflect on the following considerations:
- Whether the proposals will require them to reduce reimbursement
- Whether they will need to develop new value-based arrangements through SDPs and how these policies will be structured
- What outcomes they might need to prioritize
- How transparency in reporting provider-level payments could affect non-federal funding and SDP initiatives
Updated Approach to in Lieu of Services (ILOS) Facilitates Whole-Person Care. In January 2023, CMS issued a State Medicaid Director Letter (SMDL#23-001) advising states of the option to use the ILOS authority in Medicaid managed care programs to reduce healthcare inequities and address unmet health-related social needs (HRSNs), such as housing, food insecurity, and intimate partner violence. The proposed Medicaid managed care rule would expand upon and codify in regulation that guidance.
Considerations: Although the ILOS proposal adds reporting requirements and guardrails to address fiscal accountability, overall, the updated policy signals CMS’s willingness to support innovative state approaches to meet a continuum of beneficiary needs, including HRSNs that affect the social drivers of health. Notably, CMS advises that the substitution of an ILOS for a state plan service or setting should be cost-effective but does not need to be budget-neutral. States also can specify that an ILOS can be an immediate or longer-term substitute for a state plan service or setting.
States could pursue a variety of options under CMS’s revised ILOS framework. State Medicaid agencies and their partners can collaborate on ILOS strategies that will allow them to make further progress toward reducing healthcare inequities, as well as fulfill their quality strategy goals and objectives.
New Standards for Medical Loss Ratio Strengthen Link to Performance Improvement. Existing federal regulations require Medicaid managed care plans to report their medical loss ratio (MLR) to states annually, and, in turn, states must submit a summary of those reports to CMS. Many state MCO contracts require plans to comply with provider incentive and bonus policies; however, MCOs infrequently make incentive payments contingent on the provider meeting quantitative clinical or quality improvement standards.
Consistent with the healthcare sector’s transition toward value-based care, CMS proposes to strengthen the link between an MCOs incentive payment to a provider and the provider meeting defined quality improvement or performance metrics. Additionally, contractual language between MCOs and providers will need to more explicitly identify the dollar amounts tied to successful completion of these metrics. Only incentive payments based on quality improvement will be considered incurred claims when plans calculate their MLR; administrative costs cannot be included in quality improvement activity reporting.
Considerations. The proposed requirements are expected to add more transparency to negotiations between Medicaid MCOs and providers. MCOs will retain flexibility to determine the quality improvement or quantitative performance metrics, which carry more weight and accountability in CMS’s revised regulatory framework.
Network Adequacy Requirements Strengthen Link to Access and Rates. CMS also proposes policies that the agency believes will help strengthen Medicaid enrollees’ access to services. For example, the rule would require states to develop wait-time standards for adult and pediatric primary care and outpatient mental health, substance use disorder (SUD), and OB/GYN services, with CMS establishing federal minimum appointment wait times. States also will need to develop a quantitative network adequacy standard, beyond wait times, for certain providers.
Notably, CMS also plans to require states to submit an MCO-level analysis of MCO-to-provider payments. This analysis may provide more insights about the relationship between rates and access to certain types of providers and services. It may also improve alignment in access policies across delivery systems.
Considerations: States and MCOs should expect to need more sophisticated analysis of provider capacity at state and local market levels. This information will be critical in developing network adequacy standards and determining where additional provider support may be necessary. Expanded and new strategies may be needed to ensure compliance with the federal rules and resulting changes to state policies.
What’s Next
Many of CMS’s proposals track closely with many recent recommendations from federal commissions and oversight entities, including the Medicaid and CHIP Payment and Access Commission (MACPAC) and Government Accountability Office (GAO), which may indicate a greater likelihood that CMS will finalize those policies. If they are finalized largely as proposed, the rule will further the Biden Administration’s directional imprint on the Medicaid program.
Within the proposed rules described above, CMS identifies numerous areas where stakeholder input would be beneficial. States, MCOs, providers, and other interested stakeholders should analyze the proposals and consider submitting comments to CMS on the feasibility, potential impact, and, where applicable, alternatives to the proposed changes. Stakeholders also may use this time to begin planning for 2024 and determining what resources and tools they may need to prepare for implementation of the final regulations, as well as how their approach may vary based on state-specific factors.
For questions about the rule and how HMA’s team of experts can support your organization’s response, please contact Andrea Maresca, Joe Moser, and Patrick Tigue.
HMA Roundup
Alabama
Alabama Releases Integrated Care Network (ICN) Program RFP. The Alabama Medicaid Agency released on April 28, 2023, a request for proposals (RFP) for a vendor to provide for its primary care case management program, which serves more than 23,000 Medicaid long-term services and support (LTSS) beneficiaries. The current incumbent is Alabama Select Network. Proposals are due on June 15 and contract implementation is scheduled for October 1. Read More
Arkansas
Arkansas Proposes Medicaid Work Requirements for Expansion Program. ACHI reported on April 27, 2023, that Arkansas published a proposed amendment to implement work requirements for its Arkansas Health and Opportunity for Me (ARHOME) 1115 waiver, which serves the state’s Medicaid expansion population. Non-compliant individuals will not lose coverage, but they will be moved from a Provider-owned Arkansas Shared Savings Entity to fee-for-service coverage. The state is looking to implement the changes on January 1, 2024. Public comments will be accepted through May 23. Read More
Colorado
Colorado Legislature Passes Bill to Extend Continuous CHIP Coverage to Children 3 and Under. KDVR reported on May 1, 2023, that the Colorado House and Senate passed a bill (House Bill 1300) to extend continuous Children’s Health Insurance Program (CHIP) coverage to children three years and younger for two years. The bill will also extend coverage for one year to individuals who recently finished a prison sentence. Additionally, it will require a study on the costs and benefits of extending continuous coverage to other groups, including children under six, individuals who are unhoused, and individuals on probation. It now goes to Governor Jared Polis for his signature. Read More
Florida
Florida Legislature Passes Bill to Regulate PBMs. Health News Florida reported on May 3, 2023, that the Florida legislature passed a bill (SB 1550) to tighten regulation of pharmacy benefit managers (PBMs), prevent spread pricing, place restrictions on PBMs with affiliated pharmacies, and prevent PBMs from requiring patients to receive prescriptions by mail. The bill now goes to Governor Ron DeSantis for his signature. Read More
Florida House Passes Bill to Create Pilot Program Providing Medicaid Managed Care Coverage to Individuals with Developmental Disabilities. Health News Florida reported on April 28, 2023, that the Florida House passed a bill (HB 831) to create a pilot program to provide Medicaid managed care coverage to individuals with developmental disabilities. The pilot program would be implemented in Miami-Dade, Monroe, Hardee, Highlands, Hillsborough, Manatee, and Polk counties. If the bill is passed, the state will request federal approval by September 1, with enrollment to begin in January 2024. The Senate will take up its own version of the bill (SB 1084). Read More
Georgia
Georgia Enacts Law to Create State-based Insurance Exchange. The Associated Press reported on May 2, 2023, that Georgia Governor Brian Kemp signed legislation (Senate Bill 65) that allows the state to create its own health insurance Exchange. The state is hoping for implementation in November, but federal rules require states to spend 15 months developing a state-based Exchange so it could be pushed to 2024. There are currently nearly 900,000 Georgians who received Exchange coverage through the federal Healthcare.gov site. Read More
Iowa
Iowa Senate Passes Bill to Make Medicaid Payer of Last Resort for Medical Services. The Iowa Capital Dispatch reported on April 26, 2026, that the Iowa Senate passed a bill (House File 685) to ensure Medicaid is the payer of last resort for medical services. The bill also implements a 2.5 percent premium tax on managed care plan premiums, which would be reimbursed to Medicaid plans through the capitated rate setting process. Additionally, the bill puts a moratorium on constructing new nursing facilities. The bill now goes back to the House for a vote. Read More
Kentucky
Kentucky Governor Again Proposes Expanding Dental, Vision, Hearing Benefits for Medicaid Beneficiaries. Kentucky Health News reported on April 26, 2023, that Kentucky Governor Andy Beshear has again proposed regulations aimed at expanding dental, vision, and hearing benefits for Medicaid beneficiaries. In March, the Kentucky legislature overrode the Governor’s veto of a bill blocking the expanded benefits. The proposal is open for public comment through the end of May. Read More
Louisiana
Louisiana Candidates for Governor Promise to Keep Medicaid Expansion. The New Orleans Advocate reported on April 26, 2023, that six out of seven of the Louisiana candidates for governor have said they will keep current Governor John Bel Edward’s executive order that expanded Medicaid. The seventh candidate has said it is a possibility. The primary is on October 14, and the new Governor will take office in January 2024. Read More
Mississippi
Mississippi Medicaid Beneficiaries Are No Longer Responsible for Copays. Mississippi Today reported on May 2, 2023, that copays are no longer required for Mississippi Medicaid beneficiaries, effective May 1. Copays will now be made by the state. Read More
Missouri
Missouri House Passes Bills to Extend Postpartum Medicaid Coverage. Missourinet reported on May 2, 2023, that the Missouri House passed two bills (Senate Bills 45 and 90) to extend postpartum Medicaid coverage from 60 days to 12 months. The bills now go back to the Senate. Read More
Nevada
Nevada Expands Dental Services for Medicaid Beneficiaries with IDD. KOLO reported on May 2, 2023, that Nevada will cover expanded dental services for Medicaid beneficiaries with intellectual and developmental disabilities (IDD), using $2.5 million in federal grant and American Rescue Plan Act funds. The expanded services include preventative care, root canals, fillings, and cleanings. Read More
Nevada Releases Baseline Medicaid Enrollment Report Ahead of Redeterminations. Nevada released on February 15, 2023, a baseline Medicaid enrollment report ahead of eligibility redeterminations, showing more than 938,600 members as of January 31, 2023. Total pending applications received between March 1, 2020, and March 31, 2023, were 7,610.
New Hampshire
New Hampshire Disenrolls Nearly 15,000 Medicaid Beneficiaries Following March Redeterminations. The Associated Press reported on April 28, 2023, that New Hampshire disenrolled almost 15,000 Medicaid beneficiaries in its first round of redeterminations in March, or about 70 percent of the total reviewed. Fifty-six percent were then referred to the Exchange for coverage. The state has been conducting a public awareness campaign to encourage individuals to start the redeterminations process in advance. Read More
New York
New York Lawmakers Allocate $1.4 Billion to Financially Struggling Hospitals in Fiscal 2024 Budget. WKBW reported on May 3, 2023, that New York lawmakers passed the state budget for fiscal 2024, which includes $1.4 billion to help hospitals that are struggling financially. The budget also increases Medicaid reimbursement rates for hospitals by 7.5 percent and nursing homes by 6.5 percent. Read More
New York to Provide Adult Medicaid Beneficiaries with Expanded Dental Benefits. The New York Times reported on May 1, 2023, that adult Medicaid beneficiaries in New York will receive expanded dental benefits that include implants, root canals, and replacement dentures after a class-action lawsuit against the state was settled. The suit charged the state with denying beneficiaries medically necessary treatment. Read More
New York to Gradually Redirect Medicaid Funding from Counties. Spectrum News reported on May 1, 2023, that New York will redirect 25 percent of temporary enhanced federal Medicaid funding from counties in fiscal 2024 and 50 percent for fiscal 2025. The gradual shift is part of the proposed state budget, which still needs to be passed. Read More
Pennsylvania
Pennsylvania House Committee Advances Bill to End Medicaid Mileage Payment Restrictions on Ambulance Transportation. The Daily Item reported on May 1, 2023, that the Pennsylvania House Veteran Affairs & Emergency Preparedness Committee advanced a bill (House Bill 479) that would allow Medicaid to reimburse transportation providers $4 for each mile a patient is transported. Reimbursement is currently not permitted for the first 20 miles. Read More
Tennessee
Tennessee Medicaid to Cover Cost of Diapers for First Two Years. WKRC reported on April 30, 2023, that Tennessee’s TennCare Medicaid program will cover the cost of diapers for the first two years of a child’s life for families enrolled in Medicaid. Read More
BCBS-TN Names Casey Dungan President, CEO of BlueCare. Becker’s Payer Issues reported on April 26, 2023, that BlueCross BlueShield of Tennessee named Casey Dungan as president and chief executive of the BlueCare Division, the company’s Medicaid division serving more than 700,000 beneficiaries, effective May 1. Dungan is currently chief financial officer of BlueCare. Read More
Texas
Texas Bills Would Remove Guarantee for Hospital District-Owned Medicaid Plans. Reform Austin reported on May 1, 2023, that Texas lawmakers are considering two bills (HB 2401 and SB 651), which would remove the guarantee assuring hospital district-owned Medicaid managed care plans contracts with the state. Hospital district-owned Medicaid plans have 11 percent market share. Read More
Virginia
Virginia Projects Nearly 400,000 Medicaid Beneficiaries Will Be Disenrolled During Redeterminations. The Washington Post reported on April 30, 2023, that Virginia projects that about 394,000 Medicaid beneficiaries will be disenrolled during redeterminations. The state is beginning the process in May. Read More
Washington
Washington Publishes Plan to Remove Barriers to Access for Health, Human Services Benefits. The Washington State Health Care Authority published on May 2, 2023, a plan for removing barriers to access health and human services, including Apple Health, the state’s Medicaid program, and Temporary Assistance for Needy Families (TANF). The goal is to share information, proactively refer individuals to benefits they may qualify for, and ultimately allow individuals to seamlessly apply for multiple programs at once. The plan was developed by the Washington State Health and Human Services Enterprise Coalition, which consists of Washington state health and social service agencies. Read More
Wisconsin
Wisconsin Awards $8 Million in Grants to Provide Access to Treatment for Opioid, Stimulant Use Disorders. Wisconsin Health News reported on April 26, 2023, that the Wisconsin Department of Health Services awarded $8 million from a federal grant to three tribal nations and 22 county agencies to provide access to treatment for opioid and stimulant use disorders. An estimated 4,000 individuals will have access to treatment through the funding. Read More
National
Medicaid Beneficiaries with a Certified Nurse Midwife Present During Birth Have Better Health Outcomes, MACPAC Finds. The Medicaid and CHIP Payment and Access Commission (MACPAC) said on May 2, 2023, that Medicaid beneficiaries who had a certified nurse midwife (CNM) present when they gave birth had increased access to prenatal care and improved birth outcomes, according to a MACPAC issue brief. The brief also found that only about nine percent of births covered by Medicaid had a CNM present in 2019. Additionally, less than one percent of Medicaid-covered births occurred in birth centers, even though beneficiaries who gave birth in a freestanding birth center had more prenatal care visits and improved birth outcomes. In 2020, Medicaid covered 42 percent of births nationwide. Read More
GAO Names New MACPAC Members, Vice Chair. The U.S. Government Accountability Office (GAO) announced on May 1, 2023, the appointment of six new members and a vice chair of Medicaid and CHIP Payment and Access Commission (MACPAC). The new members are Timothy Hill, Carolyn Ingram, Patti Killingsworth, Adrienne McFadden, Jami Snyder, and John McCarthy. Robert Duncan, a current member, was named vice chair. Read More
Medicare Advantage Enrollment Surpasses Traditional Medicare in January. Becker’s Payer Issues reported on May 1, 2023, that for the first time ever, Medicare Advantage enrollment surpassed traditional Medicare, according to a Kaiser Family Foundation analysis of Centers for Medicare & Medicaid Services data. Medicare Advantage had 30.2 million members in January 2023, compared to 29.6 million for traditional Medicare. Read More
Medicaid, CHIP Enrollment Tops 93 Million in January 2023. The Centers for Medicare & Medicaid Services (CMS) announced on April 28, 2023, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) topped 93 million in January 2023, an increase of more than 660,000 from December 2022. Medicare enrollment was more than 65.5 million, up more than 56,000 from December 2022, including nearly 31.6 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. Read More
State Hospitals Work With Medicaid Beneficiaries to Maintain Coverage During Redeterminations. Becker’s Hospital Review reported on April 27, 2023, that state hospitals and health systems are working with Medicaid beneficiaries to keep them enrolled during redeterminations or assist them in finding new coverage. Indiana University Health, for example, has financial counselors available and is hosting community outreach events. Florida-based Memorial Healthcare System is working to educate individuals on the redeterminations process and finding alternative coverage. Read More
28 States Use Medicaid Managed Care to Cover Benefits for Dual Eligibles, KFF Finds. Kaiser Family Foundation (KFF) reported on April 27, 2023, that 28 states use Medicaid managed care to cover some or all benefits for dual eligibles, according to a KFF issue brief. The brief also found that 30 states had Programs of All-Inclusive Care for the Elderly, 29 required enhanced coordination between Medicaid and Dual-Eligible Special Needs Plan, and nine participated in the financial alignment initiative. Read More
U.S. Representatives Introduce Bill to Delay DSH Payment Cuts. Chief Healthcare Executive reported on April 27, 2023, that U.S. Representatives introduced a bill (HR 2665) to delay cuts to the Medicaid disproportionate share hospital (DSH) program from 2024 to 2026. Currently, the DSH program has scheduled cuts of $8 billion per year annually through 2027. Read More
CMS Proposes Rule to Improve Access to Medicaid Services in FFS, Managed Care, HCBS Programs. The Centers for Medicare & Medicaid Services (CMS) released on April 27, 2023, a proposed rule aimed at improving access to services in the Medicaid program across fee-for-service (FFS), managed care, and home and community-based services (HCBS). The rule proposes increased transparency and accountability, standardizing data and monitoring, and having states promote active beneficiary engagement. Read More
CMS Proposes Rule to Address Health Equity for Medicaid, CHIP Managed Care Members. The Centers for Medicare & Medicaid Services (CMS) released on April 27, 2023, a proposed rule aimed at improving access to care, outcomes, and equity among Medicaid and Children’s Health Insurance Program (CHIP) managed care enrollees. The rule proposes addressing standards for timely access to care, reducing the burden for state directed payments and quality reporting requirements, and establishing a rating system for Medicaid and CHIP managed care plans. Read More
Industry News
Centene to Sell Apixio to New Mountain Capital. Centene announced on May 3, 2023, that it has signed a definitive agreement to sell Apixio to New York-based investment firm New Mountain Capital. Apixio is an artificial intelligence platform that helps health plans improve administrative, clinical, and financial outcomes. Terms of the transaction were not disclosed. Read More
CVS Health Completes Acquisition of Oak Street Health. CVS Health announced on May 2, 2023, it had completed the acquisition of Oak Street Health, a primary care provider, for $39 per share in cash, representing an enterprise value of $10.6 billion. CVS entered a definitive agreement to acquire Oak Street Health in February. Read More
BCBS-MI, BCBS-VT to Pursue Affiliation. Blue Cross Blue Shield of Michigan announced on May 1, 2023, an agreement to formally affiliate with Blue Cross and Blue Shield of Vermont. The agreement needs to be approved by state regulators. Read More
Bright Health Considers Selling CA Medicare Advantage Business. Bright Health Group announced on April 28, 2023, that it is considering selling its Medicare Advantage business in California, which consists of Brand New Day and Central Health Plan and serves about 125,000 members. The company is also working on exiting the Exchange. Read More
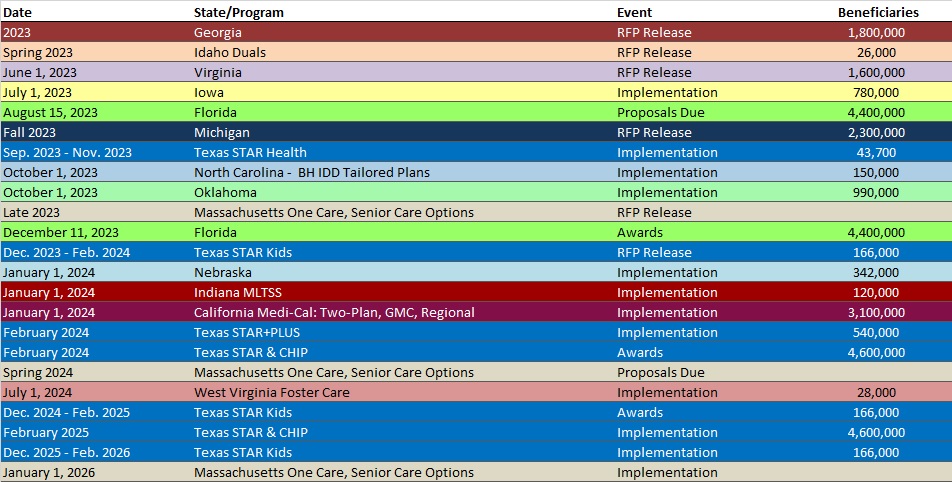
RFP Calendar
HMA News & Events
Upcoming HMA Webinar:
Using 1115 Justice Waivers to Improve Carceral Healthcare Delivery Information. HMA’s 4-part webinar series on 1115 Justice Waivers: Building Bridges of Health for Persons Leaving Carceral Settings, is designed to help plans and other stakeholders improve the long-term health outcomes of individuals. Part 2 will focus on the carceral settings operational healthcare practices, including intake screenings to aid in risk assignment and facilitate community re-entry. Thursday, May 18, 2023, 2 PM ET/11 AM PT. Click here to register.
Wakely, an HMA Company, White Papers:
ACO REACH 2023 Landscape. The Center for Medicare and Medicaid Services has publicly released information on the Accountable Care Organizations (ACOs) participating in the ACO Realizing Equity, Access, and Community Health (ACO REACH) Model in Performance Year 2023. Read More
Wakely 2024 Final HHS-HCC Model Impact. In this paper, we analyze the impact of risk adjustment model changes from the final 2024 HHS HCC risk adjustment model based on 2022 data collected through the WNRAR project. We scored data with the final 2022, 2023, and 2024 HHS HCC risk adjustment models and summarized the impact to risk scores and relative risk of issuers in this paper. Read More
Leavitt Partners, an HMA Company, Announcement:
Amy Comstock Rick Joins Leavitt Partners, an HMA Company. Amy Comstock Rick, former president and chief executive officer (CEO) of the Food and Drug Law Institute (FDLI), joined Leavitt Partners, an HMA Company as a principal on March 20. Rick has over 30 years of experience leading organizations, executing strategy, transforming organizational culture, building consensus, and advocating policies across constituencies. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Georgia Medicaid Managed Care Enrollment is Up 2%, May-23 Data
- Kentucky Medicaid Managed Care Enrollment is Up 1.9%, Apr-23 Data
- Minnesota Medicaid Managed Care Enrollment is Up 1.4%, Feb-23 Data
- Nevada Medicaid Managed Care Enrollment is Up 1.8%, Mar-23 Data
- North Carolina Medicaid Managed Care Enrollment is Up 1.5%, Mar-23 Data
- North Carolina Medicaid Managed Care Enrollment is Up 2%, Apr-23 Data
- South Carolina Medicaid Managed Care Enrollment is Up 2.1%, Apr-23 Data
- West Virginia Medicaid Managed Care Enrollment is Up 0.6%, Jan-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alabama Medicaid Agency Integrated Care Networks RFP, Apr-23
- Mississippi Medicaid FFS Non-Emergency Transportation Brokerage Services IFB, Award, and Related Documents, 2023
- Ohio Medicaid Non-Emergency Transportation Services for Warren County RFP, May-23
- Texas D-SNP Contracts, 2023
Medicaid Program Reports, Data, and Updates:
- Alaska DHSS Annual Medicaid Reform Reports, FY 2016-22
- Alaska Long-Term Forecast of Medicaid Enrollment and Spending, FY 2023-24
- Arkansas Comparison Payment Rate Development for Child and Youth Behavioral Health Individual HCBS Services and New Intensive In-Home Service Presentation, Nov-22
- Arkansas DHS External Quality Review Technical Report, 2020-22
- Hawaii Med-QUEST Home and Community-Based Services Rate Study Presentations, Mar-23
- Hawaii Med-QUEST Home and Community-Based Services Rate Study Report, Dec-22
- Indiana Home and Community-Based Services Spend Plan Overview, Dec-22
- Indiana Medicaid External Quality Review Reports, 2012-22
- Kansas KanCare Program External Quality Review Reports, 2020-23
- Nevada Medicaid COVID-19 Public Health Emergency Unwinding Plan and Baseline Report, Apr-23
- Pennsylvania Medical Assistance Advisory Committee (MAAC) Meeting Materials, Apr-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.