HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Biden Administration Encourages States to Apply for Medicaid Reentry 1115 Demonstration for Individuals in Carceral Settings

- Arizona Requests Additional $3.3 Billion in Fiscal 2023 for Medicaid Managed Care Payments

- Redeterminations News: California, Georgia, Indiana, Missouri, Nebraska, Pennsylvania

- Colorado Enacts Legislation Eliminating Medicaid Co-pays for Pharmacy, Outpatient Services

- Illinois Health Benefits Program for Immigrant Seniors, Adults Is Expected to Enroll 98,500

- Maryland Releases Medicaid Managed Care External Quality Review RFP

- Washington Requests Medicaid Coverage for Former Foster Youth, Continuous CHIP Enrollment for Children Up to Age Six

- U.S. Senators Introduce Legislation to Ban PBM Spread Pricing

- Kaiser Permanente to Acquire Geisinger Health

In Focus
Biden Administration Encourages States to Apply for Medicaid Reentry 1115 Demonstration for Individuals in Carceral Settings
This week our In Focus section reviews guidance from the Centers for Medicare & Medicaid Services (CMS), released on April 17, 2023, encouraging states to apply for the new Medicaid Reentry Section 1115 Demonstration Opportunity. The demonstration is aimed at helping improve care for individuals in carceral settings prior to their release.
Background
The United States has approximately 1.9 million individuals incarcerated nationwide. Studies have shown higher rates of mental illness and physical health care needs in incarcerated populations compared to the general population, as well as associations between jail incarceration and increases in premature death rates from infectious diseases, chronic lower respiratory disease, drug use, and suicide.
CMS states that formerly incarcerated individuals with physical and mental health conditions and substance-use disorders (SUDs) typically have difficulty succeeding upon reentry due to obstacles present immediately at release, such as high rates of poverty and high risk of poor health outcomes. These individuals tend to face barriers in obtaining housing, education, employment, and health care access upon release. They often do not seek outpatient medical care and are at significantly increased risk for emergency department (ED) use and hospitalization.
Purpose and Goals
After collecting feedback from stakeholders, including managed care organizations, Medicaid beneficiaries, health care providers, the National Association of Medicaid Directors, and other representatives from local, state, and federal jail and prison systems, CMS designed the Reentry Section 1115 Demonstration Opportunity. The services covered under this demonstration opportunity should aim to improve access to community resources that address the health care and health-related social needs of the carceral population, with the aims of improving health outcomes, reducing emergency department visits, and inpatient hospital admissions for both physical and behavioral health issues once they are released and return to the community.
The purpose of this demonstration opportunity is to provide short-term Medicaid enrollment assistance and pre-release coverage for certain services to facilitate successful care transitions. The full goals, as quoted from CMS, are as follows:
- “Increase coverage, continuity of coverage, and appropriate service uptake through assessment of eligibility and availability of coverage for benefits in carceral settings just prior to release
- Improve access to services prior to release and improve transitions and continuity of care into the community upon release and during reentry
- Improve coordination and communication between correctional systems, Medicaid systems, managed care plans, and community-based providers
- Increase additional investments in health care and related services, aimed at improving the quality of care for beneficiaries in carceral settings and in the community to maximize successful reentry post-release
- Improve connections between carceral settings and community services upon release to address physical health, behavioral health, and health-related social needs
- Reduce all-cause deaths in the near-term post-release
- Reduce number of ED visits and inpatient hospitalizations among recently incarcerated Medicaid beneficiaries through increased receipt of preventive and routine physical and behavioral health care”
CMS encourages states to engage with individuals who were formerly incarcerated when contemplating the design and implementation of their proposal. CMS also encourages states to design a broadly defined demonstration population that includes otherwise eligible, soon-to-be former incarcerated individuals. States have the flexibility to target population, such as individuals with specific conditions, but are encouraged to be mindful of undiagnosed conditions. States should have a plan to ensure incarcerated individuals will be enrolled in Medicaid upon their release, applying for Medicaid no later than 45 days before the day of release.
Reentry Section 1115 Demonstration Opportunity
To receive approval for the demonstration, the state proposal must include in the pre-release benefit backage:
- Case management to assess and address physical and behavioral health needs and health-related social needs;
- Medication-assisted treatment (MAT) services for all types of SUD as clinically appropriate, with accompanying counseling; and
- A 30-day supply of all prescription medications that have been prescribed for the beneficiary at the time of release, provided to the beneficiary immediately upon release from the correctional facility.
In addition to these three services states may include other important physical and behavioral health services to cover on a pre-release basis, such as family planning services and supplies, behavioral health or preventive services, including those provided by peer supporters/community health workers, or treatment for Hepatitis C. CMS is also open to states requesting Section 1115 expenditure authority to provide medical supplies, equipment, and appliances.
The Reentry Section 1115 Demonstration opportunity is not intended to shift current carceral health care costs to the Medicaid program. CMS will not approve state proposals to receive federal Medicaid matching funds for any existing carceral health care services funded with state or local dollars unless the state agrees to reinvest the total amount of new federal matching funds received into activities or initiatives that increase access to or improve the quality of health care services for individuals who are incarcerated.
CMS also expects states to refrain from including federal prisons as a setting in which demonstration-covered prerelease services are provided under the opportunity.
States with approved demonstrations will need to submit an implementation plan, a monitoring protocol, quarterly/annual monitoring reports, a mid-point assessment report, an evaluation design, and interim/summative evaluation reports.
California
California became the first state to receive approval for a Section 1115 waiver amendment earlier this year to provide limited Medicaid services to incarcerated individuals for up to 90 days immediately prior to release. The approval period runs through December 31, 2026, timed with the expiration of the CalAIM Medi-Cal waiver demonstration. California’s reentry demonstration initiative aims to provide health care interventions at earlier opportunities for incarcerated individuals to reduce acute services utilization and adverse health outcomes. The state anticipates it will increase coverage and continuity of coverage for eligible beneficiaries, improve care transitions for beneficiaries as they reenter the community, and reduce morbidity and mortality in the near-term post-release.
Pre-release services include comprehensive care management, physical and behavioral clinical consultation, lab and radiology, MAT, community health worker services, and medications and durable medical equipment. A care manager will be assigned to eligible individuals to establish a relationship, understand their health needs, coordinate vital services, and make a plan for community transition, including connecting the individual to a community-based care manager they can work with upon their release. Additionally, all counties implementing Medi-Cal application processes in jails and youth correctional facilities will “suspend” the Medicaid status while an individual is in jail or prison, so that it can be easily “turned on” when they enter the community.
On April 6, 2023, HMA held a webinar titled, “Medicaid authority and opportunity to build new programs for justice-involved individuals.” A replay can be watched here. HMA will announce additional webinars on the topic.
HMA Roundup
Alaska
Alaska Senate Approves Bill to Extend Postpartum Medicaid Coverage. The Anchorage Daily News reported on April 19, 2023, that the Alaska Senate approved a bill (Senate Bill 58) to extend postpartum Medicaid coverage from 60 days to 12 months, effective July 1, 2024. The extended coverage would impact about 1,600 individuals annually. A House version of the same bill advanced out of committee for a full House vote. Read More
Arizona
Arizona Requests Additional $3.3 Billion in Fiscal 2023 for Medicaid Managed Care Payments. The Sierra Vista Herald reported on April 25, 2023, that the Arizona Health Care Cost Containment System requested an additional $3.3 billion to continue making payments to Medicaid managed care plans through the end of fiscal 2023. The agency said it cannot make May and June payments without the additional funds, which include state dollars and authorization to spend federal matching funds. Meanwhile, Arizona lawmakers and Governor Katie Hobbs are still working to develop a fiscal 2024 budget, after Hobbs vetoed an early version. Read More
California
California Releases Baseline Medicaid Enrollment Report Ahead of Redeterminations. California released on April 20, 2023, a baseline Medicaid enrollment report ahead of eligibility redeterminations, showing 15.8 million members as of March 31, 2023. Total pending applications received between March 1, 2020, and March 31, 2023, were 220,999.
Colorado
Colorado Enacts Legislation Eliminating Medicaid Co-pays for Pharmacy, Outpatient Services. The Colorado Department of Health Care Policy & Financing announced on April 20, 2023, that Governor Jared Polis signed legislation (SB23-222) eliminating co-pays for Medicaid beneficiaries for pharmacy and outpatient health care services. The bill is a companion to a resolution in the state’s fiscal 2024 budget that would eliminate most co-pays, including inpatient, primary care, specialty, lab, radiology, and more. Co-pays would still be required for non-emergency care received in an emergency room. Read More
Florida
Florida House Committee Approves Bill to Increase Regulation of PBMs. Health News Florida reported on April 24, 2023, that the Florida House Appropriations Committee approved a bill aimed at strengthening regulation of pharmacy benefit managers (PBMs). HB 1509 would increase the Office of Insurance Regulation’s authority over PBMs, prevent spread pricing, place restrictions on PBMs with affiliated pharmacies, and stop PBMs from requiring patients to receive prescriptions by mail. The bill now heads to the Health & Human Services Committee before going to the full House. A separate Senate version (SB 1550) of the bill has already passed in the Senate. Read More
Georgia
Georgia Launches Marketing Campaign to Raise Awareness of Medicaid Redeterminations. Capitol Beat News Service reported on April 25, 2023, that Georgia launched a marketing campaign to raise awareness of the Medicaid eligibility redeterminations process. The campaign includes materials available in multiple languages and self-service kiosks in public libraries. The fiscal 2023 mid-year budget also included funding to hire additional case managers to assist with the process. Read More
Illinois
Illinois Health Benefits Program for Immigrant Seniors, Adults Is Expected to Enroll 98,500, Cost $990 Million in Fiscal 2024. The Capitol News Illinois reported on April 21, 2023, that the Health Benefits for Immigrant Seniors and Adults program, which provides healthcare to individuals not eligible for Medicaid due to citizenship status, will cost $990 million in state fiscal year 2024, according to a presentation by the Illinois Department of Healthcare and Family Services. The department estimates 98,500 individuals will be enrolled. Read More
Indiana
Indiana Expects Net Reduction of 400,000 Medicaid Members by May 2024. The Indiana Family and Social Services Administration said on April 19, 2023, that it expects net Medicaid enrollment to decline by 400,000 through May 2024. Costs are expected to rise due to the phasing out of the enhanced federal Medicaid matching funds.
Maryland
Maryland Releases Medicaid Managed Care External Quality Review RFP. The Maryland Department of Health released on April 20, 2023, a request for proposals (RFP) for an external quality review organization for the state’s HealthChoice Medicaid managed care program. Proposals are due May 30. The contract will run for five years. Current incumbent is Qlarant. Read More
Missouri
Missouri Estimates Up to 200,000 Medicaid Beneficiaries Will Lose Coverage During Redeterminations. KTTN News reported on April 26, 2023, that up to 200,000 Medicaid beneficiaries in Missouri could lose coverage during eligibility redeterminations, according to the state Department of Social Services. The state is encouraging individuals to update contact information so they receive renewal forms. The first round of renewal forms will be sent out the first week of May. Individuals who no longer qualify for Medicaid coverage will be referred to the Exchange. Read More
Montana
Montana Senate Passes $15 Million Budget Amendment to Increase Medicaid Provider Reimbursement Rates. The Longview News-Journal reported on April 25, 2023, that the Montana Senate passed a state budget amendment (House Bill 2) to increase Medicaid provider reimbursement rates by $15 million. The House will vote on the amendment next. The funding is expected to be matched by $29.5 million in federal funds.
Nebraska
Nebraska Expects 40,000 to 80,000 Medicaid Beneficiaries to Lose Coverage Following Eligibility Redeterminations. The Nebraska Examiner reported on April 25, 2023, that the Nebraska Department of Health and Human Services began processing Medicaid eligibility redeterminations on March 1 for beneficiaries with an April or May renewal date. The state is estimating 40,000 to 50,000 individuals will lose coverage, with April being the first month beneficiaries will be disenrolled. The state is encouraging everyone to update their contact information so they receive renewal materials. Read More
New York
New York Nursing Homes File Lawsuit Over Law Requiring 70 Percent of Revenue be Spent on Care. The Center Square reported on April 17, 2023, that 132 New York nursing homes filed a lawsuit in the state Supreme Court alleging that a provision of a law requiring public and private residential health care facilities to spend a minimum of 70 percent of their total operating revenue on care, and at least 40 percent of revenue on resident-facing staffing, is unconstitutional. The lawsuit seeks a temporary injunction barring the state from enforcing penalties against providers. The provision comes from a 2021 law requiring nursing homes with profits over a 5 percent cap to turn those funds over to a state-managed fund. Read More
North Carolina
North Carolina House Introduces Bill to Increase Access to Behavioral Health Services. WRAL News reported on April 25, 2023, that North Carolina House Representatives introduced a bill to increase access to behavioral health services using some of the additional federal funding the state will receive for expanding Medicaid. The bill includes $225 million for improving access to behavioral health services, $200 million for a statewide behavioral health crisis system, and $50 million for telehealth programs and a centralized bed registry. Read More
House Committee Advances Bill to Allow BCBS-NC to Keep Surplus Funds Instead of Returning to Policyholders. The Associated Press reported on April 25, 2023, that the North Carolina House Health Committee advanced a bill that would allow not-for-profit Blue Cross Blue Shield of North Carolina to transfer surplus funds to a holding company instead of returning it to policyholders. Current state law requires companies to refund certain funds to policyholders or to lower premium rates. The House Insurance Committee will debate the bill next. Read More
North Dakota
North Dakota Legislature Overrides Veto of Bill to Enhance Choice in Health Plan Provider Networks. KXNET reported on April 17, 2023, that the North Dakota Legislature voted to override Governor Doug Burgum’s veto of a bill (House Bill 1416) that says a health plan may not obstruct an individual’s choice by excluding a provider from their panel who is both within their coverage area and qualified to meet the terms and conditions of participation in the plan. The bill now goes to the Senate for a vote. Read More
Ohio
Ohio House Proposes Budget With Increases In Medicaid Funding for Nursing Homes, Home Care, Assisted Living. Cleveland.com reported on April 24, 2023, that the Ohio House is working on a proposed budget that would raise home care worker wages to $18 an hour and increase Medicaid assisted living waiver funding by 48 percent. The budget would also allow nursing homes to adjust cost reimbursement figures for inflation more frequently and offers an add-on payment to facilities that put Medicaid patients in private rooms. Read More
Oklahoma
Oklahoma Senate Overrides Veto of Bill Requiring $600 Million Surplus to be Spent on Normal Medicaid Operations. KOSU reported on April 20, 2023, that the Oklahoma Senate voted to override Governor Kevin Stitt’s veto of a bill (Senate Bill 1130) that requires a $600 million surplus to be spent on normal Medicaid operations. The Governor wanted to save the money for long-term health policy investments. The House has not voted on the override yet. Read More
Pennsylvania
Pennsylvania Could Disenroll Up to 617,000 Medicaid Members During Redeterminations. The Daily Item reported on April 22, 2023, that about 617,000 Medicaid beneficiaries in Pennsylvania could lose coverage following eligibility redeterminations, according to state officials. Another 598,000 had not completed a renewal application. Read More
Texas
Texas House Advances Bill to Extend Postpartum Medicaid Coverage. The Texas Tribune reported on April 20, 2023, that the Texas House advanced a bill (House Bill 12) to extend postpartum Medicaid coverage from 60 days to 12 months. The House will take a final vote before the bill moves to the Senate. The House passed a similar bill in the last session, but the Senate decreased coverage to six months and the bill stalled. Read More
Utah
Utah Requests Section 1115 Amendment to Increase Premium Reimbursements for Children Under the UPP. The Centers for Medicare & Medicaid Services announced on April 19, 2023, that Utah submitted an amendment request for its Section 1115 Medicaid Reform waiver to increase the maximum reimbursement allowable for children under the Utah Premium Partnership for Health Insurance Program (UPP). The amendment would also allow the state to make changes through the administrative rulemaking process instead of a demonstration amendment. The federal comment period is open until May 19. Read More
Washington
Washington Requests Medicaid Coverage for Former Foster Youth, Continuous CHIP Enrollment for Children Up to Age Six in Waiver Amendment. The Washington State Health Care Authority announced on April 20, 2023, that it has opened the public comment period on a draft Section 1115 waiver amendment to authorize Medicaid coverage for former foster care youth and continuous enrollment for the Children’s Health Insurance Program (CHIP) for children through six years of age. The public comment period is open through May 22.
Wisconsin
Wisconsin Assembly Passes Bill Requiring Medicaid Eligibility Redeterminations Every Six Months. Wisconsin Health News reported on April 26. 2023, that the Wisconsin Assembly passed a bill requiring Medicaid beneficiaries to go through eligibility redeterminations every six months. Governor Tony Evers vetoed a similar bill in 2022. Read More
National
Medicaid, Medicare Spent $82.4 Billion on Supplemental Payments to Acute Care Providers in 2020, Report Finds. Health Payer Intelligence reported on April 26, 2023, that Medicaid spent $71.7 billion on supplemental payments to acute care providers in 2020, while Medicare spent $10.7 billion, according to a brief from the Urban Institute and Robert Wood Johnson Foundation. Nearly 36 percent of Medicaid spending came from managed care plans, and 44 percent came from fee-for-service, primarily consisting of disproportionate share hospital payments and upper payment limit payments. Read More
U.S. Senators Introduce Legislation to Ban PBM Spread Pricing. Modern Healthcare reported on April 25, 2023, that U.S. Senators Bernie Sanders (D-VT) and Bill Cassidy (R-LA) introduced the Pharmacy Benefit Manager (PBM) Reform Act of 2023, which would ban spread pricing, require PBMs to pass the full value of rebates on to customers, disclose drug prices, and report how much money they receive from pharmaceutical company copay assistance programs. The two also introduced legislation to get generic drugs to market faster. Sanders is chair of the Senate Health, Education, Labor and Pensions Committee; Cassidy is ranking member. Read More
600,000 Medicaid Beneficiaries Would Lose Coverage if Work Requirements are Implemented, CBO Says. The Congressional Budget Office (CBO) said on April 25, 2023, that a House bill (HR 2811) to implement Medicaid work requirements would result in about 600,000 adult Medicaid beneficiaries losing coverage. CBO also projects that about 15 million beneficiaries would be subject to work requirements per year, and the federal government would save an estimated $109 billion over 10 years. The U.S. Department of Health and Human Services released a separate report projecting that about 21 million beneficiaries would be subject to the requirements. Read More
U.S. Representatives Introduce Bill to Expand In-home Medicare Benefits. Fierce Healthcare reported on April 24, 2023, that U.S. Representatives Adrian Smith (R-NE) and Debbie Dingell (D-MI) introduced a bill to extend access to various home care services delivered to Medicare beneficiaries. The bill includes at least 12 hours per week of personal care services plus funding for in-home testing, dialysis, and primary care. Read More
HHS Releases Rule to Allow Medicaid, Exchange Coverage for ‘Dreamers’. The U.S. Department of Health and Human Services (HHS) released on April 24, 2023, a proposed rule that would make Deferred Action for Childhood Arrivals (DACA) recipients, aka, “Dreamers,” eligible for Medicaid and Exchange coverage. The proposed effective date is November 1, 2023. The expansion would benefit approximately 580,000 individuals. Read More
Six States Receive Federal Approval to Extend Continuous Medicaid Eligibility. The Kaiser Family Foundation reported on April 24, 2023, that six states (Kansas, Massachusetts, New Jersey, New York, Oregon, and Washington) received federal approval for Section 1115 waivers that allow them to extend continuous Medicaid eligibility beyond what is allowed under federal law. New Mexico has also submitted a request, but it is still pending. Read More
AHIP Launches Campaign Targeting Prescription Drug Prices. Modern Healthcare reported on April 24, 2023, that AHIP launched an advertising campaign targeting pharmaceutical companies over high prescription drug costs. The campaign will air on television and social media through the end of 2023. Read More
45 Percent of Medicaid Beneficiaries with IDD Have Additional Health Condition, GAO Study Finds. The U.S. Government Accountability Office (GAO) reported on April 24, 2023, that 45 percent of Medicaid beneficiaries with intellectual or developmental disabilities (IDD) had an additional health condition, such as an anxiety disorder or high blood pressure, according to a GAO study. The study also found that Medicaid paid between $51,000 and $70,000 for beneficiaries with IDD, which is two to five times more than the average for all Medicaid beneficiaries with disabilities. The study used 2019 Medicaid data from Colorado, Florida, Georgia, Indiana, Oklahoma, and South Dakota. Read More
House Committee to Consider Legislation Requiring Site Neutral Medicare Payments for Outpatient Services. CQ reported on April 21, 2023, that the U.S. House Energy and Commerce Committee will hold a hearing on April 26 to discuss draft legislation that would require site neutral Medicare payments for some outpatient services. Medicare currently pays hospitals more than physicians’ offices and surgical centers. Read More
HHS Releases Ownership Data of All Medicare-certified Hospice and Home Health Agencies. The U.S. Department of Health and Human Services (HHS) released on April 20, 2023, the ownership data of all Medicare-certified hospice and home health agencies on the Centers for Medicare & Medicaid Services website in an effort to increase transparency. Detailed ownership information will be available for more than 6,000 hospices and 11,000 home health agencies. Data elements include practice location addresses, national provider identifier, CMS certification number, information about each owner such as whether it is an organization or an individual, any associated mergers/acquisitions, changes in ownership, and more. Data is expected to be released on a quarterly basis. Read More
Medicaid Scammers Seize on Redeterminations Process. Modern Healthcare reported on April 20, 2023, that Medicaid scammers have seized on the redeterminations process, asking individuals to send money or lose their coverage. States urge individuals who think they have been scammed to contact their attorney general. Read More
DOD Upholds Tricare West Region Contract Award to TriWest. Military.com reported on April 20, 2023, that the U.S. Department of Defense (DOD) upheld its award of Tricare’s western region contract to TriWest. Health Net Federal Services, the current incumbent, filed a protest against the awards. Humana Military was awarded the contract for the eastern region. Read More
U.S. House Republicans Propose Medicaid Work Requirements. Fierce Healthcare reported on April 20, 2023, that the U.S. House Republicans released a plan to address the national debt, which includes Medicaid work requirements. The plan does not include cuts to Medicare. The plan is unlikely to pass in the Senate. Read More
CHCS Announces State Medicaid Learning Collaborative on Diabetes Care. The Center for Health Care Strategies announced on April 12, 2023, an opportunity for State Medicaid Agencies to participate in a learning collaborative called Accelerating Access to Continuous Glucose Monitors in Medicaid to Improve Diabetes Care. With support from The Leona M. and Harry B. Helmsley Charitable Trust, the Accelerator program is designed to help states transform their approach to addressing diabetes and move the needle on reducing health inequities in Medicaid by increasing access to CGMs. Participating states will be able to direct $75,000 in program funds to leverage expertise and services in support of their proposed project. State applications are due May 31, 2023. Read More
Hispanic and Black, Non-Hispanic Individuals Less Likely to Have Usual Source of Care, MACPAC Finds. The Medicaid and CHIP Payment and Access Commission (MACPAC) published an issue brief in April 2023, that found Hispanic and Black, non-Hispanic individuals were less likely to report having a usual source of care and more likely to cite urgent care or emergency rooms as their usual source, than white, non-Hispanic individuals, based on data from the 2016-2022 Association of American Medical Colleges Consumer Survey of Health Care Access. Overall, 68.1 percent of individuals reported having a usual source of care. Read More
Industry News
Kaiser Permanente to Acquire Geisinger Health. Health Payer Specialist reported on April 26, 2023, that Kaiser Permanente will acquire Geisinger Health, which would be rolled into a new, not-for-profit entity called Risant Health. Geisinger’s chief executive Jaewon Ryu, MD, will lead the new entity, which is expected to acquire five or six other health systems over the next five years. Read More
Humana/CenterWell Home Health Acquires Trilogy Home Health. Home Health Care News reported on April 24, 2023, that Humana subsidiary CenterWell Home Health acquired Trilogy Home Health, a Florida-based provider of home health care, personal care, and care coordination services. CenterWell provides home health services to more than 350,000 patients per year with a presence in 38 states. Read More
UnitedHealth Subsidiary LHC Group Acquires Summit Home Care. Becker’s Payer Issues reported on April 20, 2023, that UnitedHealth’s LHC Group is acquiring Summit Home Care, a Delaware-based home health company. The acquisition price was not disclosed. Read More
Cigna/Express Scripts to Increase Reimbursement Rates for Rural Pharmacies. Modern Healthcare reported on April 20, 2023, that pharmacy benefit manager Cigna/Express Scripts will increase reimbursement rates for independent rural pharmacies. The company will also pay independent pharmacies in both rural and urban areas for vaccinations, testing, nutrition counseling, behavioral health screening, and other preventative and routine services. Read More
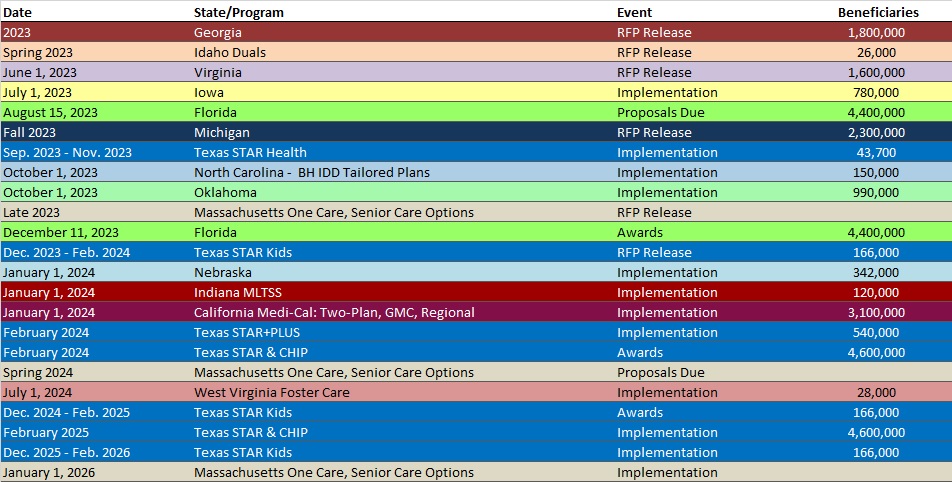
RFP Calendar
HMA News & Events
Wakely, an HMA Company, White Paper:
The End of Medicaid Continuous Coverage: Programmatic and Rate Setting Considerations. Medicaid enrollment grew significantly during the COVID-19 pandemic, primarily because of a moratorium on member redetermination activities required to receive enhanced federal funding. In many cases, the significant growth in Medicaid enrollment also has affected average population acuity (i.e., cost). Significant Medicaid disenrollment in the coming months contributes to budgetary uncertainty for states and may result in somewhat elevated financial risk for contracted health plans. State-specific actions could mitigate this uncertainty to some extent. This paper explores the risk and potential state-specific actions that could mitigate this uncertainty. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arizona Medicaid Managed Care Enrollment is Up 1%, Feb-23 Data
- Illinois Medicaid Managed Care Enrollment is Up 0.7%, Mar-23 Data
- Illinois Dual Demo Enrollment is Down 5.1%, Mar-23 Data
- Kansas Medicaid Managed Care Enrollment is Up 1.2%, Feb-23 Data
- Kansas Medicaid Managed Care Enrollment is Up 1.2%, Mar-23 Data
- Kansas Medicaid Managed Care Enrollment is Up 0.7%, Apr-23 Data
- New York Medicaid Managed Care Enrollment is Flat, Jan-23 Data
- Oregon Medicaid Managed Care Enrollment is Up 1.7%, Mar-23 Data
- South Carolina Medicaid Managed Care Enrollment is Up 1.5%, Mar-23 Data
- South Carolina Dual Demo Enrollment is Down 9.3%, Mar-23 Data
- Wisconsin Medicaid Managed Care Enrollment is Up 1.7%, Mar-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Maryland HealthChoice Program External Quality Review RFP, Apr-23
- Massachusetts MassHealth ACO RFR, Responses, and Award, 2022
- New York Disproportionate Share Hospitals (DSH) Audits RFP, Apr-23
Medicaid Program Reports, Data, and Updates:
- California Plan for Unwinding Continuous Coverage and Baseline Enrollment Report, Apr-23
- Illinois Health Benefits for Immigrant Seniors and Adults Updated Enrollment and Cost Estimates, Mar-23
- Indiana Medicaid Forecast Update, Apr-23
- Maryland HealthChoice Quality Strategy, 2022-24
- Mississippi Medicaid Managed Care Preliminary Rate Certifications, 2023
- North Carolina NEMT Fact Sheets, Mar-23
- North Carolina Tailored Plan Fact Sheets, Apr-23
- Pennsylvania Medicaid Managed Care Organization Outcomes Program Report, 2020-23
- Pennsylvania Statewide Quality Care Assessment Program Report, Dec-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
