This week's roundup:
- In Focus: New HMA Analysis: Options for Improving California’s Substance Use Disorder Treatment System
- Arizona Extends ALTCS-EPD Program Contracts for Another Year
- Colorado Announces Intent to Award Regional Accountable Entity ACC Phase III Contracts
- New Hampshire Receives Federal Approval for Mobile Crisis Intervention Teams
- Pennsylvania Lawmakers, Advocates Look to Reverse Medicaid Dental Policy
- Washington Marketplace Insurance Rates to Increase Nearly 11 Percent in 2025
- Hospitals File Lawsuit Against HHS Over Medicare Advantage Calculation in DSH Payments
- Medicare Health Plan Ratings Drop for NCQA’s 2024 Equity Measures
- Cigna Sues FTC Over PBM Drug Pricing Report
- More News Here
In Focus
New HMA Analysis: Options for Improving California’s Substance Use Disorder Treatment System
In recognition of National Recovery Month this September, our In Focus section spotlights a new report from Health Management Associates, Inc. (HMA), Substance Use Disorder in California: A Focused Landscape Analysis. Published in August 2024 with support from the California Health Care Foundation, this analysis provides valuable insights into California’s substance use disorder (SUD) treatment system and offers actionable recommendations for improvement that can be applicable for other states.
The SUD Landscape in California
SUDs continue to be a significant issue both nationally and in California. In 2022, approximately 9 percent of Californians ages 12 and older met the criteria for SUD, compared with 16.5 percent nationally in 2021. The prevalence of SUD is also on the rise: in 2015, 8.1 percent of Californians ages 12 and older met SUD criteria, rising to 8.8 percent in 2022. Of the Californians struggling with SUD, only 10 percent received treatment for their condition, compared with 6 percent nationally in 2021. Overall, 81 percent of US adults who received care for SUD reported struggling to access necessary services.
California’s public behavioral health system siloes specialty mental health (MH) services, mild-to-moderate MH services, and SUD treatment services, resulting in a fragmented and inconsistent system that struggles to effectively support people with co-occurring conditions.
County plans administer specialty behavioral health (BH) services. They all have memorandums of understanding with the state’s Department of Health Care Services that are separate from the state arrangements to provide physical healthcare services. BH programs vary significantly across the state because counties operate them differently, with key variations in access policies, quality monitoring, services, and programming. Mild-to-moderate (non-specialty) MH benefits are administered by Medicaid managed care plans. Much of the state’s SUD treatment is operated by the Drug Medi-Cal Organized Delivery System (DMC-ODS).
Barriers to Care: Key Findings
System barriers prevent many Californians with SUD from accessing adequate care. Interviewees received a pre-interview questionnaire to determine the factors they believe have the greatest impact on access to SUD treatment. According to 11 out of 14 respondents, lack of access to housing and residential services is a “huge barrier” to SUD treatment.
Other barriers to care access, ranked in order, include limited access to food, transportation, and other social drivers of health (SDOH), SUD provider shortages, stigma against people with SUD, disparities in service availability across racial/ethnic groups and other populations, and complex referral and intake processes.
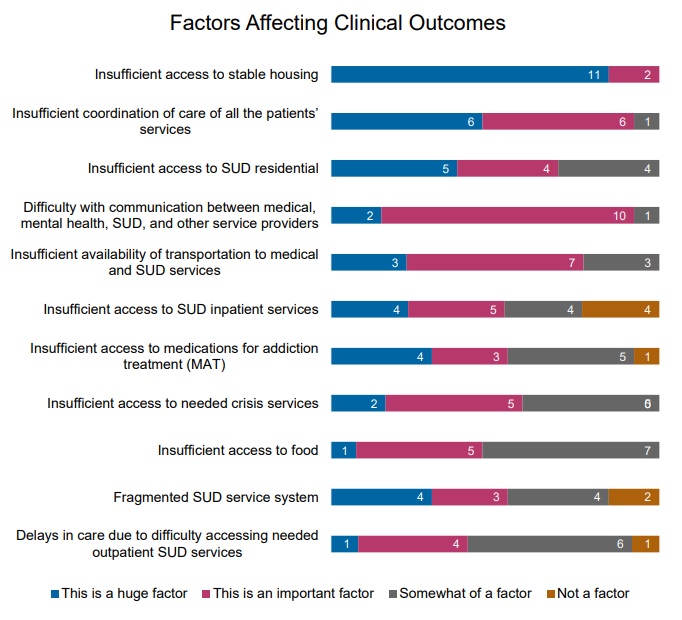
Respondents also identified factors that could negatively affect clinical outcomes for people with SUD. Insufficient access to stable housing ranked first, followed by inadequate care coordination, and limited access to residential SUD treatment. Respondents ranked 11 factors as follows:
Figure 1: Factors Leading to Reduced Outcomes, Ranked from a List of 11
Service gaps pose another significant barrier to people accessing SUD treatment, and some populations are more likely to encounter challenges than others. According to the respondents, by various population groups, Latine/Hispanic populations, African American/Black populations, and Native American/Alaska Native populations are most likely to experience SUD service gaps. By age, people who are 19−25 years old (transition-age youth) and adults ages 26−65 are most likely to face service gaps.
Opportunities to Support Improvements in SUD Care
Findings and recommendations to enhance support for individuals are informed by surveys and interviews conducted with SUD stakeholders from across the state. Recommendations highlighted in the report include:
- Investments in the workforce. By addressing the shortage of licensed clinicians and implementing peer support workers into the care continuum, the state would increase access to care. Many stakeholders have positioned themselves to meet SUD needs, but they cannot do so without an adequate workforce. Furthermore, the workforce would benefit from strengthening culturally responsive training in evidence-based practices.
- Expansion of residential treatment services and housing options. There is a growing need, especially among transition-age youth, for residential treatment and SUD recovery housing.
- Increased access to and training around harm reduction. Although stigma around harm reduction has decreased, training and access remains a barrier. Respondents highlighted the need to better manage contingencies, make methadone more accessible, establish safe consumption sites, expand medication assisted treatment for SUD and AUD, and improve the availability of Narcan.
- MH and SUD treatment integration. Offering concurrent MH and SUD treatment with the same providers can help improve access to care for people with co-occurring conditions and minimize duplication.
- Improved care coordination. Respondents suggested funding formal care coordination positions—a recommendation that is consistent with the national movement toward the coordinated care model applied in certified community behavioral health centers.
- Improved data literacy. Behavioral health organizations need support and technical assistance to learn how to track and use data to support continuous quality improvement.
What to Watch
The overarching challenges facing California’s recovery system are present in other states. These states can adapt the strategies discussed in this report to address their own SUD concerns. In California, as in other states, an important aspect of addressing SUD treatment involves strategic allocation of opioid settlement dollars. These funds, resulting from legal settlements with opioid manufacturers and distributors, are expected to play a significant role in improving the state’s SUD treatment infrastructure, especially when considered alongside available federal funding, demonstrations, and regulatory flexibilities.
Connect With Us
The upcoming HMA event, Unlocking Solutions in Medicaid, Medicare, and Marketplace, will offer more opportunities to engage with leaders from various sectors who are advancing solutions to improve access to care and reducing access disparities. Throughout the conference, federal and state officials, community leaders, and national experts will shed light on the challenges and solutions to these issues.
For more information on the report, contact report authors Charles Robbins, Principal, Marc Avery, MD, Principal, Serene Olin, PhD, Principal, Emma Clark, PhD, Consultant, Rachel Johnson-Yates, Associate Principal, and Brittany Doughty, Consultant.
HMA Roundup
Arizona
Arizona Extends ALTCS-EPD Program Contracts for Another Year. Health Payer Specialist reported on September 12, 2024, that Arizona has extended its Long Term Care System/Elderly & Physically Disabled (ALTCS-EPD) program contracts with incumbents Banner-University Family Care, Mercy Care Plan, and UnitedHealthcare through September 30, 2025. The decision comes after the state faced protests over the awarded contracts from Centene/Health Net Access and UnitedHealthcare Community Plan. Contracts were scheduled to go live October 1. The state is expected to soon provide additional information and finalize updated contracts.
Colorado
Colorado Announces Intent to Award Regional Accountable Entity ACC Phase III Contracts. The Colorado Department of Health Care Policy and Financing announced on September 11, 2024, its intent to award the Regional Accountable Entity contracts for Accountable Care Collaborative (ACC) Phase III to incumbents Rocky Mountain Health Plans, Northeast Health Partners, Colorado Community Health Alliance, and Colorado Access. Contracts begin on July 1, 2025, and run for seven years. Incumbent Health Colorado was not awarded a contract. Denver Health will continue to operate under Colorado Access’ region.
Florida
Florida to Submit Managed Medical Assistance Section 1115 Demonstration Amendment. The Florida Agency for Health Care Administration announced on September 17, 2024, that it will submit an amendment to the Centers for Medicare & Medicaid Services that will align its Managed Medical Assistance (MMA) Section 1115 demonstration program with changes resulting from the state’s recent re-procurement of Medicaid managed medical care and dental plans. The changes include expanding the Behavioral Health and Supportive Housing Assistance pilot program, enhancing the MMA enrollment process, and transitioning certain services from MMA to the dental program. These changes will allow all members of a family who are enrolled in Medicaid to receive services under a single plan that provides MMA, Long-Term Care, and specialty product benefits. The public comment period will be open for a 30-day period.
Iowa
Iowa Fails to Conduct Timely Nursing Home Inspections, Audit Finds. The Daily Iowan reported on September 16, 2024, that Iowa conducted inspections for nursing homes certified to accept Medicare or Medicaid every 17.1 months on average, which is four months longer than the federal mandate, according to a report by State Auditor Rob Sand. The report found that 85.4 percent of Iowa’s 403 certified nursing homes did not meet the frequency of inspections standard set by the Centers for Medicare & Medicaid Services on at least one of the past three inspections. Additionally, roughly 45 percent of Iowa’s nursing homes that reported staffing information do not meet the federal standard of total nursing staff levels.
Maine
Maine to Submit Rate Amendments for HCBS Demonstrations. The Maine Department of Health & Human Services announced on September 12, 2024, that it plans to submit rate amendments for its Medicaid section 1915(c) Home and Community Based Services (HCBS) demonstrations. The four waivers include the Intellectual Disabilities or Autism Spectrum Disorder Waiver; HCBS for Adults with Other Related Conditions; HCBS for Members with Brain Injury; and Support Services for Adults with Intellectual Disabilities or Autism Spectrum Disorder. Public comments will be accepted through October 11.
Michigan
Michigan Partners with 10 Agencies to Create Adult Crisis Stabilization Units. The Michigan Department of Health and Human Services announced on September 17, 2024, that it is partnering with 10 behavioral health agencies across the state to create Adult Crisis Stabilization Units (CSUs), as part of a $32 million investment included in the fiscal 2023 budget. Adult CSUs are being developed throughout nine counties including Clinton, Eaton, Genesee, Ingham, Kalamazoo, Kent, Macomb, Oakland, and Wayne. Two agencies, Network180 and Detroit Wayne Integrated Health Network Crisis Care Center, have already begun providing CSU services to their communities.
Mississippi
Mississippi NEMT Provider is Three Times Over Limit for Late, Missed Rides in July. Mississippi Today reported on September 17, 2024, that Mississippi’s Medicaid Non-Emergency Medical Transportation (NEMT) provider, Modivcare, indicated that five percent of scheduled rides were late and one percent were missed in July, according to the company’s first report to the Division of Medicaid. The company’s contract states that no more than two percent of scheduled rides should be late or missed each day, making them three times over the allowable limit. Modivcare began its three-year, $96.5 million contract with the state in June 2024.
Nevada
Nevada Seeks to Eliminate Health Care Disparities by 2028 in Proposed Medicaid Quality Strategy. The Nevada Division of Health Care Financing and Policy (DHCFP) released on September 16, 2024, a draft Medicaid quality strategy for 2025-27. The strategy outlines DHCFP’s goals for improving Nevada Medicaid and Nevada Check Up members’ health outcomes by December 31, 2027, such as increasing preventive services and evidence-based practices; reducing opioid and prescription drug misuse; and reducing or eliminating health disparities. DHCFP is seeking public comments on the draft, which will be accepted for a 30-day period.
New Hampshire
New Hampshire Receives Federal Approval for Mobile Crisis Intervention Teams. The Centers for Medicare & Medicaid Services announced on September 12, 2024, that it has approved New Hampshire’s Medicaid State Plan amendment to implement community-based mobile crisis intervention teams for Medicaid members experiencing a behavioral health crisis. New Hampshire is the 20th state, along with the District of Columbia, to implement community-based mental health and substance use disorder services under the American Rescue Plan.
New York
New York Legislature Passes Bill Providing Medicaid Reimbursement for Creative Arts Therapists. Spectrum News reported on September 12, 2024, that a New York bill to allow Medicaid reimbursement for creative arts therapists is waiting to be delivered to Governor Kathy Hochul after being passed by the Legislature.
North Carolina
North Carolina Legislature Approves $377 Million in Medicaid Funding; $81 Million Less than Requested. NC Health News reported on September 12, 2024, that North Carolina’s legislature approved $277 million in recurring funds and an additional $100 million in one-time funds to help the state Department of Health and Human Services (DHHS) cover rising Medicaid costs. DHHS initially requested $458 million to cover inflation costs and make up for the upcoming reduction in North Carolina’s federal Medicaid funding match, which will give the state an estimated $136 million less federal dollars in 2025, compared to 2024. The funding now awaits approval from the governor.
Pennsylvania
Pennsylvania Lawmakers, Advocates Look to Reverse Medicaid Dental Policy. Spotlight PA reported on September 13, 2024, that Pennsylvania lawmakers and advocates are looking to reverse a 2011 policy limiting dental services through Pennsylvania’s Medicaid program. Prior to 2011, Medicaid covered complex procedures, including crowns and root canals. The 2011 policy limited coverage to routine dental exams, cleanings, and fillings, unless the Department of Human Services allows an exception when someone has a life-threatening condition or would require more expensive care later. Two bills in the state’s legislature look to restore the complex procedures, at a minimum.
South Carolina
South Carolina Medicaid Director Robby Kerr to Retire in November. The South Carolina Daily Gazette reported on September 16, 2024, that Robby Kerr, director of the state Department of Health and Human Services, will retire on November 1. Kerr has been the Medicaid director since April 2021, and previously served in the same role from 2003 to 2007. His successor has not been announced.
Texas
Texas Superior HealthPlan Invested $43 Million for Medicaid, CHIP Value-added Services Over Five Years. Superior HealthPlan, a subsidiary of Centene Corporation, announced on September 12, 2024, that it invested $43.3 million to provide Medicaid and Children’s Health Insurance Program (CHIP) value-added services across Texas from 2019 through 2023. Nearly half of the spending was on vision care, totaling $15.5 million. The insurer spent another $12 million on over-the-counter items, $11 million on dental care, and $2.5 million on sports physicals.
Texas Children’s CEO Mark Wallace to Retire; Debra Sukin to Replace. Texas Children’s announced on September 12, 2024, that chief executive Mark A. Wallace will be retiring on October 4. Current president Debra Sukin will begin her new role as president and chief executive on October 5.
Washington
Washington Marketplace Insurance Rates to Increase Nearly 11 Percent in 2025. The Center Square reported on September 16, 2024, that premiums for individual insurance plans available through the Washington Health Benefit Exchange will increase by 10.7 percent on average in 2025. The state’s Office of the Insurance Commissioner attributes the hike to cost of care increases and a growing number of people seeking care.
National
Medicare Health Plan Ratings Drop for NCQA’s 2024 Equity Measures. Modern Healthcare reported on September 16, 2024, that National Committee for Quality Assurance’s (NCQA) ratings on prevention and equity dropped slightly for Medicare insurers in 2024. Medicare plans’ scores decreased to an average of 3.08 stars, from 3.4 stars in 2023. However, patient experience scores increased in 2024, and two Medicare plans achieved 5-star ratings. NCQA ratings measure health equity, preventive care services, treatment, and patient experience on Medicare, Medicaid, and commercial health plans.
Hospitals File Lawsuit Against HHS Over Medicare Advantage Calculation in DSH Payments. Modern Healthcare reported on September 11, 2024, that 80 hospitals from California, Ohio, Pennsylvania, and Texas have filed a lawsuit against the U.S Department of Health and Human Services Department (HHS) over how inpatient care for Medicare Advantage is factored into disproportionate share hospital (DSH) payments. The lawsuit, filed in the U.S. District Court for the District of Columbia, claims the hospitals lost an estimated $3 to $4 billion over a nine-year period by retroactively including MA calculations for payments issued prior to October 1, 2013. The hospitals are seeking a reversal of denied appeals with the Provider Reimbursement Review Board, removal of Medicare Advantage days from DSH calculations, and elimination of the 2023 regulation.
HHS OIG Releases Revised Medicaid Fraud Control Unit Standards. The U.S. Department of Health and Human Services Office of the Inspector General (HHS OIG) released on September 18, 2024, updated Medicaid Fraud Control Unit (MFCU) regulation, which outlines 12 standards for assessing MFCU performance. The standards, which were developed with the National Association of MFCUs, include complying with requirements; maintaining staff; enforcing policy and procedures; maintaining adequate referrals; maintaining case progression, case mix, and case information; cooperating with authorities on fraud cases; making program recommendations to and developing agreements with Medicaid agencies; exercising fiscal control; and administering adequate training. MFCU regulation was last updated in 2012.
CMS Considers Cybersecurity Policies for Third-party Healthcare Vendors. Modern Healthcare reported on September 13, 2024, that the Centers for Medicare & Medicaid Services (CMS) is assessing the agency’s options to prevent severe disruptions from cyberattacks, like implementing cybersecurity oversight policies for third-party healthcare vendors following the Change Healthcare cyberattack earlier this year. The agency is also working with the U.S. Department of Health and Human Services to enhance accountability and promote cybersecurity practices for healthcare vendors.
ICE Detainer Requests Associated With Lower Medicaid Enrollment, Study Finds. Drexel News reported on September 16, 2024, that individuals living in counties with the highest number of U.S. Immigration and Customs Enforcement (ICE) detainer requests are less likely to enroll in Medicaid, according to a Health Affairs study from Drexel’s Dornsife School of Public Health using data from 2011, 2016, and 2019. The association between detainer requests and lower enrollment was stronger among adults in households with at least one immigrant relative, compared to U.S.-born households. The study suggests that some eligible immigrants might forgo benefits for fear of jeopardizing their own legal status or that of a family member or friend.
MACPAC Meeting Is Scheduled for September 19-20. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on September 13, 2024, that its next meeting will be held on September 19-20. Among the topics for discussion will be recaps of recent rules from the Centers for Medicare & Medicaid Services on access to Medicaid services; timely access to Medicaid home-and community-based services; external quality review in managed care; and juvenile justice.
Industry News
Cigna Sues FTC Over PBM Drug Pricing Report. Health Payer Specialist reported on September 17, 2024, that Cigna’s subsidiary Evernorth, which includes Express Scripts, is suing the Federal Trade Commission (FTC) over a pharmacy benefit manager (PBM) report, calling the report’s conclusion that PBMs raise drug costs defamatory. Express Scripts has demanded the July 2024 report be retracted after claiming the report leans heavily on unverified public comments and ignores documents and data provided by the PBM.
HCSC Approved to Acquire HealthSpring of Florida. Health Payer Specialist reported on September 16, 2024, that Chicago-based Health Care Service Corporation (HCSC) has received regulatory approval for an indirect acquisition of Cigna’s HealthSpring of Florida, a Medicare Advantage plan with more than 47,500 enrollees. HCSC has a pending sale with the Cigna Group to acquire its Medicare business, including Cigna’s Medicare Advantage plan, supplemental benefits, Medicare Part D offerings, and CareAllies, a value-based care management subsidiary for $3.3 billion. The deal is expected to close in early 2025, pending regulatory approval.
Walgreens to Pay $107 Million Over Improper Medicaid, Medicare Prescription Billing Claims. Modern Healthcare reported on September 13, 2024, that Walgreens Boots Alliance will pay a $106.8 million fine to the U.S. Department of Justice over allegations it violated the False Claims Act between 2009 and 2020, billing for Medicare and Medicaid prescriptions that were processed but never collected by patients. Walgreens credited the violation to an error in its electronic pharmacy management system, which it reported to the government and has since corrected. Of the fine paid by Walgreens, $91.8 million will be returned to the federal government and $14.9 will go back to states where lawsuits were filed.
Kaiser Permanente to Close Last Skilled Nursing Facility in November. Modern Healthcare reported on September 11, 2024, that Kaiser Permanente is closing its last skilled nursing facility in November. Patients at the 176-bed nursing home in San Leandro, California will be transitioned to their homes or other skilled nursing facilities in the area.
Three Largest PBMs Target Different Payer Markets, Study Finds. Healthcare Dive reported on September 11, 2024, that the largest pharmacy benefit managers (PBMs) — CVS/Caremark, Cigna/Express Scripts, and UnitedHealth/Optum Rx — provided services for 80 percent of the market in 2023. The analysis performed by the USC Schaeffer Center also found that the PBMs have large shares of across different insurance markets. The study found that Caremark controls 39.2 percent of all PBM services in Medicaid managed care; Express Scripts controls 28 percent of the commercial market; and Optum Rx’s largest share is in Medicare Part D, at 27.7 percent. The PBMs are part of corporations that also operate major insurers in those markets.
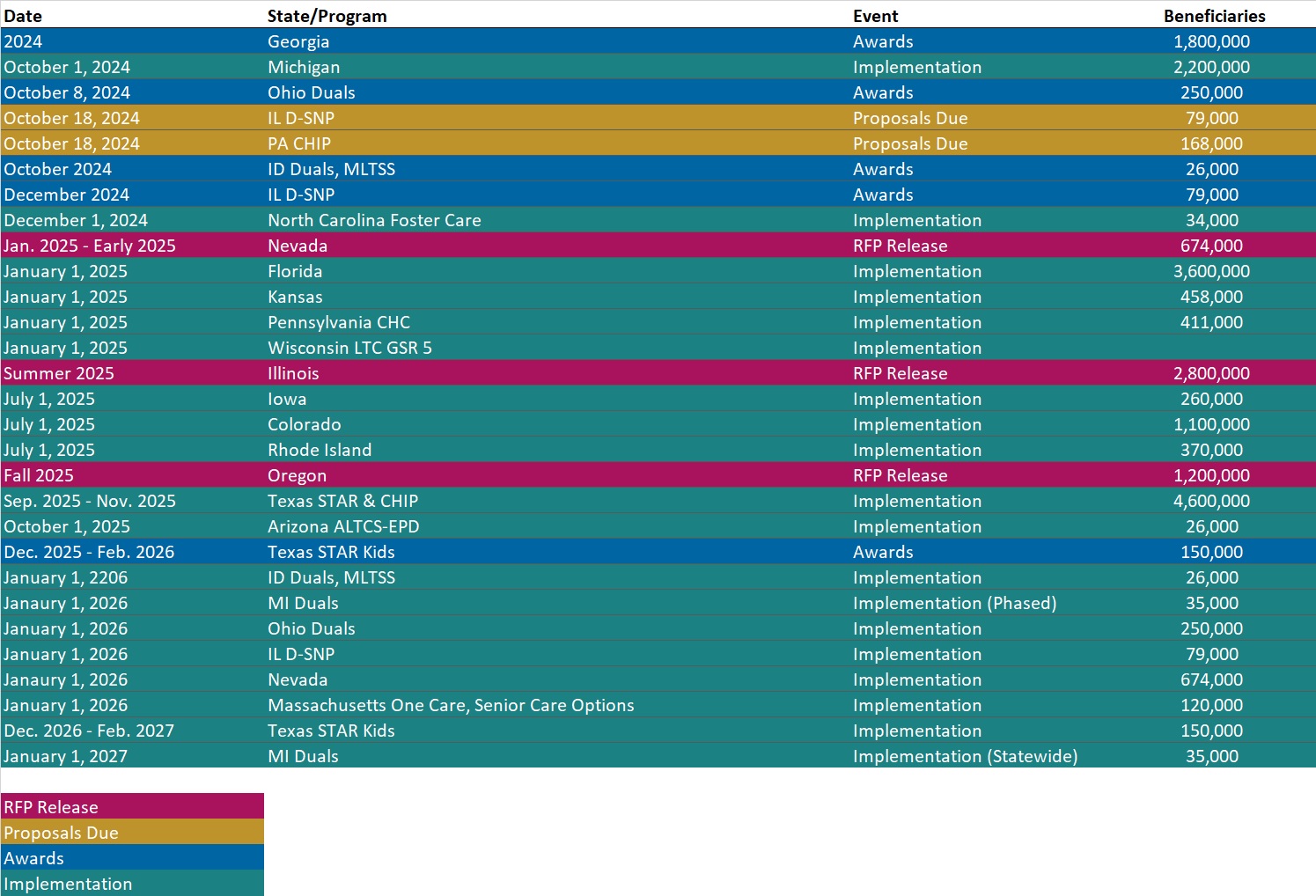
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Reports
- Updated Federal Regulatory Tracker
- Updated Indiana State Overview
- Updated Iowa State Overview
Medicaid Data
Medicaid Enrollment:
- Kentucky Medicaid Managed Care Enrollment is Down 8.1%, Sep-24 Data
- Minnesota Medicaid Managed Care Enrollment is Down 14.1%, Aug-24 Data
- Mississippi Medicaid Managed Care Enrollment is Up 16.1%, Jul-24 Data
- Nevada Medicaid Managed Care Enrollment is Down 7.1%, Mar-24 Data
- New Mexico Medicaid Managed Care Enrollment is Flat, Mar-24 Data
- Pennsylvania Medicaid LTSS Enrollment is Down 5.3%, Jul-24 Data
- Pennsylvania SNP Membership at 247,323, Mar-24 Data
- Pennsylvania Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Tennessee Medicaid Managed Care Enrollment is Down 12.2%, Jul-24 Data
- Tennessee SNP Membership at 154,106, Mar-24 Data
- Tennessee Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
- Vermont Medicaid Fee for Service vs. Managed Care Penetration, 2014-23
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- California Medicare Advantage D-SNP Model Contracts, 2021-25
- Indiana Medicare Advantage D-SNP Model Contract, 2024
- Indiana Self-Direction Financial Management Services RFP and Attachments, Jul-24
- New Hampshire Medicaid to Schools Financing RFI, Sep-24
Medicaid Program Reports, Data, and Updates:
- Arkansas DHS Annual Statistical Reports, 2018-23
- Florida Managed Medical Assistance (MMA) 1115 Demonstration Waiver Approval and Amendments, 2016-24
- Maine 1915(c) Home and Community-Based Services Waiver and Amendments, 2024
- Nevada Draft Medicaid, CHIP Quality Strategy, 2025-27
- Nevada Dual Special Needs Plan Report, Jun-24
- Oklahoma OHCA Review of Funding Sources Report, Sep-24
- Rhode Island MMP to D-SNP Transition Plan, 2022-23
- Vermont Medicaid Program Enrollment and Expenditures Reports, SFY 2018-24
- West Virginia Medicaid Mountain Health Trust EQR Reports, 2009-23
- HHS OIG Revised Medicaid Fraud Control Unit Standards, Sep-24
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at amaresca@healthmanagement.com.