This week, our In Focus section reviews the KanCare Medicaid capitated managed care request for proposals (RFP), released October 2, 2023, by the Kansas Department of Health and Environment and Department for Aging and Disability Services. The program covers approximately 520,000 beneficiaries and is worth $4.1 billion. New contracts would begin January 2025.
KanCare Background
KanCare is the state’s Medicaid managed care program, covering both traditional Medicaid and Children’s Health Insurance Program (CHIP) members. In all, KanCare covers approximately 320,000 children, 79,000 parents and pregnant women, 59,000 individuals with disabilities, and 54,000 individuals ages 65 and older.
Managed care organizations (MCOs) provide statewide integrated physical health, behavioral health, and long-term services and supports. Covered services include nursing facility care and home and community-based services, as well as Medicaid-funded inpatient and outpatient mental health and substance use disorder services and seven Section 1915(c) HCBS waiver programs.
Kansas is not currently an expansion state. While the governor’s 2024 budget plan called for Medicaid expansion, lawmakers rejected the proposal during the last legislative session.
In 2022, the state legislature delayed the procurement until 2023 to ensure that it occurred after the gubernatorial election and extended current MCO contracts through 2024.
RFP
Kansas expects to select three MCOs. The RFP includes a renewed focus on integrated, whole-person care, workforce retention, and accountability measures for the MCOs. The state lists the main goals for the KanCare procurement as:
- Improve member experience and satisfaction
- Improve health outcomes by providing integrated, holistic care with a focus on the impacts of social determinants of health
- Reduce healthcare disparities
- Expand provider network and direct care workforce capacity and skill sets
- Improve provider experience and encourage provider participation in Medicaid
- Increase the use of cost-effective strategies to improve health outcomes and the service delivery system
- Leverage data to promote continuous quality improvement
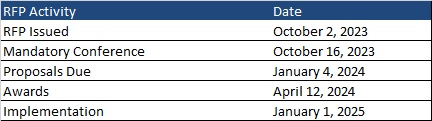
Timeline
A mandatory pre-bid conference will take place on October 16, 2023. Proposals are due January 4, 2024, with awards expected April 12, 2024. Contracts will be effective January 1, 2025, through December 31, 2027, with up to two one-year renewal options. Following is the timeline leading up to implementation.
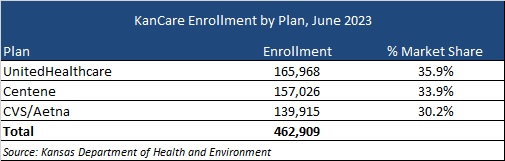
Current Market
Incumbents are Centene, CVS/Aetna, and UnitedHealthcare. A breakdown of market share by enrollment as of June 2023 can be seen in the table below. Other insurers have already cited their interest in bidding for the new contracts.