This week, our In Focus reviews the Kaiser Health Foundation (KFF) analysis, Fiscal and Enrollment Implications of Medicaid Continuous Coverage Requirement During and After the PHE Ends, published on May 10, 2022.
Background
The end of the public health emergency (PHE), slated for mid-July 2022, will come with significant implications for state Medicaid programs. If the PHE is not extended further, states that meet maintenance of eligibility (MOE) requirements under the Families First Coronavirus Response Act (FFCRA) will lose the enhanced 6.2 percentage point increase in the federal Medicaid match rate (FMAP) on September 30, 2022. The continuous Medicaid enrollment requirement under the MOE will also end August 1, 2022.
KFF examined two potential scenarios on how states may manage the resumption of eligibility redeterminations and disenrollments, based on two scenarios predicted by past KFF surveys. In a February 2022 survey of Medicaid directors, state officials predicted Medicaid enrollment would decline by five percent after the PHE ends. Meanwhile, in a January 2022 survey, states signaled they expect on average about 13 percent of Medicaid enrollees to be disenrolled at the end of the continuous enrollment requirement.
Enrollment
From 2019 through the end of fiscal 2022 (September 30, 2022), KFF estimates that Medicaid enrollment will grow 22.2 million, or approximately 25 percent, to 110.3 million. Baseline Medicaid growth would account for 3.5 million of the gain, while the MOE continuous enrollment requirement would account for 18.7 million. Of this predicted growth, children represent 42 percent, Affordable Care Act (ACA) expansion adults 33 percent, other adults 20 percent, persons with disabilities three percent, and seniors three percent. Over this same period, KFF estimates baseline growth would have been four percent, prior to the pandemic and MOE.
Based on the two scenarios, KFF predicts that Medicaid enrollment will decline from 5.3 million (assuming a five percent decline) to 14.2 million (assuming a 13 percent decline) from fiscal 2022 to fiscal 2023, with the largest losses expected among ACA expansion adults, other adults, and children.
Spending
KFF estimates that between fiscal 2020 and fiscal 2022, states will have received $100.4 billion in fiscal relief due to the enhanced FMAP. KFF estimates state costs due to the additional MOE enrollees is $47.2 billion. On average, the total expected fiscal relief is 2.3 times the costs of the additional enrollment. See table below.
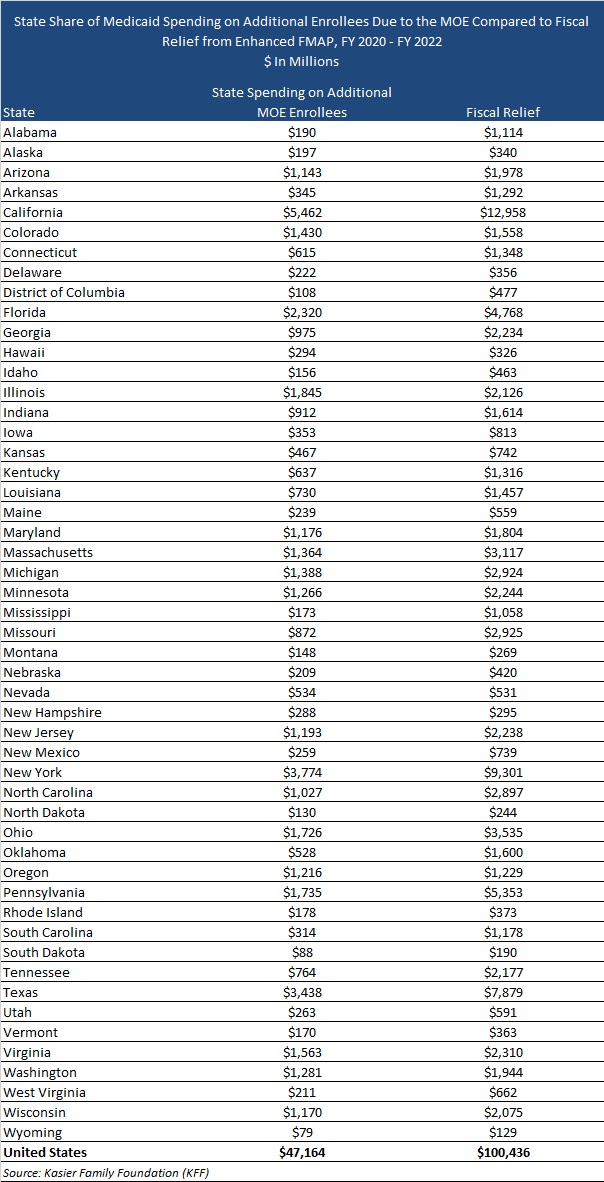
States that did not expand Medicaid tended to draw more federal fiscal relief than expansion states. However, during the pandemic, Idaho, Missouri, Nebraska, Oklahoma, and Utah expanded their Medicaid programs.
KFF estimates state Medicaid spending over the entire pandemic period will be six percent lower compared to baseline state Medicaid spending without the enhanced FMAP or enrollment growth due to the MOE, while federal spending will be 19 percent higher than baseline federal spending. After the end of the PHE, state Medicaid directors expect total Medicaid spending to increase by two percent due to changes in per enrollee expenses following the end of the PHE.