This week, our In Focus section reviews the Ohio Medicaid Managed Care request for applications (RFA) released by the Ohio Department of Medicaid (ODM) on September 30, 2020. The RFA follows the release of two requests for information (RFIs) in June 2019 and February 2020, soliciting feedback from individuals, providers, and interested bidders to help design a new Medicaid managed care program. Ohio will award contracts, worth over $11 billion annually, to no more than five managed care organizations (MCOs) in each of the state’s three regions (Central/Southeast Region, Northeast Region, and West Region), with implementation beginning January 5, 2022. The procurement will not include the MyCare Ohio dual demonstration.
Ohio Medicaid Managed Care Program
The selected MCOs will be part of a re-imagined Medicaid managed care program that unbundles the current program and will include a new single, statewide prepaid inpatient health plan, the OhioRISE Plan, that will provide behavioral health services to children with serious/complex behavioral health needs that are at risk or in foster care; and a single pharmacy benefit manager (SPBM) responsible for providing and managing pharmacy benefits for all Medicaid eligibles. Together, the MCOs, the OhioRISE Plan, and the SPBM will coordinate and collaborate to achieve a seamless service delivery system for members, providers, and system partners. ODM will also centralize claims submission, prior authorization submission, through a single fiscal intermediary (FI) for non-pharmacy claims and authorization requests, which the FI will triage to the MCOs for adjudication. Additionally, ODM is centralizing provider credentialing and re-credentialing to minimize the provider burden of credentialing with multiple MCOs.
MCOs will provide physical health services to all enrollees and will provide behavioral health services to all enrollees except for behavioral health to children in the OhioRISE Plan. MCOs will be required to use population health management principles to address health inequities and disparities, including removing barriers to care through the use of alternative sites and providers of care, such as telehealth and community-based providers; providing preventive, health promotion, and wellness services; connecting with communities; ensuring health equity in all policies, practices, and operations; and recognizing the significance of behavioral health needs to overall health and wellbeing.
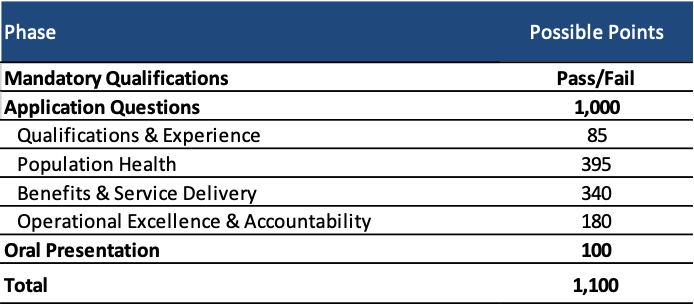
Evaluation
The evaluation process consists of four phases:
- Phase I: Review of Mandatory Qualifications
- Phase II: Review of Responses to Application Questions
- Phase III: Oral Presentation
- Phase IV: Selection
MCOs can achieve a total of 1,100 points. Those with the highest total scores will be recommended for selection.
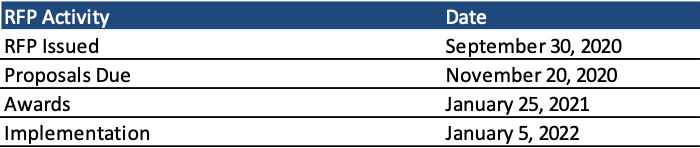
Timeline
Proposals are due November 20 with awards expected January 25, 2021. The contracts will run from January 5, 2022, through June 30, 2024, with optional renewals each fiscal year afterwards.
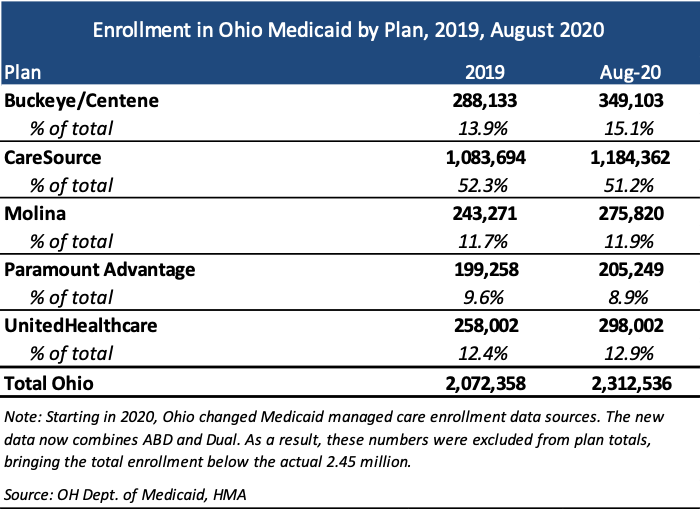
Current Market
Current incumbents are Centene/Buckeye Health Plan, CareSource, Molina, Paramount Advantage, and UnitedHealthcare. The market is largely dominated by CareSource, with over half the market share based on covered lives.