This week's roundup:
- In Focus: West Virginia Releases RFP for Foster Children, Youth in Medicaid Managed Care

- Arizona Receives Federal Approval of Waiver to Address Housing Needs

- District of Columbia Council Approves Medicaid Managed Care Contracts Idaho Delays Behavioral Medicaid Awards to November 2022

- Indiana Awards Medicaid FFS Prior Authorization, Utilization Management Contract to Kepro

- Kansas, Gainwell Implement Modular Medicaid Technology Platform

- Nevada Governor Tells SEIU He Will Push for Higher Payment Rates, Wages for Home Care Providers

- New York Fails to Follow Up on Dual Eligible Cost Savings Opportunities, Comptroller Finds

- Pennsylvania Senate Committee Passes Resolution to Study Medicaid Addiction Treatment Reimbursement Rates

- HHS Offers States Certified Community Behavioral Health Clinic Planning Grants

- CMS Agrees to Release Audits of 90 Medicare Advantage Plans

- Acorn Health Acquires 7 Applied Behavior Analysis Centers in FL, VA For Children With Autism

- Brave Health Secures $40 Million in Latest Funding Round to Expand Virtual Medicaid Behavioral Health Services

In Focus
West Virginia Releases RFP for Foster Children, Youth in Medicaid Managed Care
This week, our In Focus section reviews the Mountain Health Promise request for proposals (RFP) released by the West Virginia Department of Health and Human Resources on September 30, 2022, for specialized Medicaid managed care for children and youth in foster care.
Mountain Health Promise RFP
The selected managed care organization (MCO) will provide physical and behavioral health services to children and youth in the foster care system, individuals receiving adoption assistance, youth formerly in foster care up to age 26 who aged out of foster care while on Medicaid in the state of West Virginia, and children eligible under the children with serious emotional disorders (CSED) waiver. Potential expansions could include, but are not limited to, children at risk for foster care placement and the family of youth in crisis. Additionally, the MCO will act as an administrative services organization (ASO) and provide statewide administrative services for all individuals accessing socially necessary services (SNS).
Some of the goals of the program include:
- Enhance coordination and access to services
- Enhance quality of care and minimize barriers for youth and families/improve access to treatment
- Reduce fragmentation and offer seamless continuity of care
- Improve health and social outcomes for youth and impacts on families
- Help reduce the number of children removed from the home and reduce lengths of stay per episode of care through increased family-centered care that provides necessary and coordinated services to all members of the family
- Decrease children involved with the juvenile justice and corrections systems
- Reduce out-of-home and out-of-state placements
- Develop new or enhance existing services, such as children’s mobile crisis response (CMCR), inState Psychiatric Residential Treatment Facilities (PRTF) to reduce the need for out-of-state placements, and intensive home-based treatment
Physical and behavioral health services will be reimbursed through a Medicaid per member per month (PMPM) capitation payment. For SNS administration, the Bureau for Social Services (BSS) will provide a fixed monthly rate. The PMPM capitation rate will not include carved out SNS costs.
It is encouraged, but not required, that the MCO subcontract with regional child welfare organizations, residential mental health treatment facilities (RMHTFs), and organizations that provide home and community-based services for children with serious emotional disorders to assist in the care coordination of services for this population.
Market
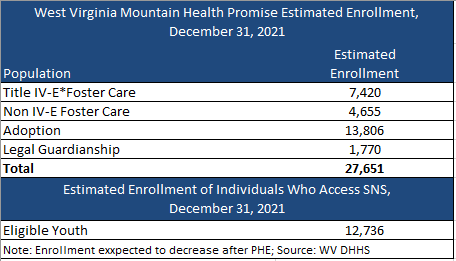
There are nearly 28,000 individuals currently enrolled in Mountain Health Promise, with about 13,000 eligible for SNS. Enrollment, however, is expected to decrease following the end of the Public Health Emergency (PHE). CVS Health/Aetna is the incumbent plan. Aetna had contracted with Kepro to serve as the ASO for SNS.
Timeline
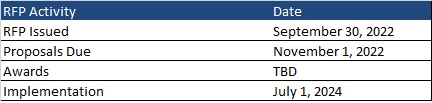
Proposals are due November 1, 2022. The contract is anticipated to run from July 1, 2024, through June 30, 2025, with three one-year options.
Evaluation
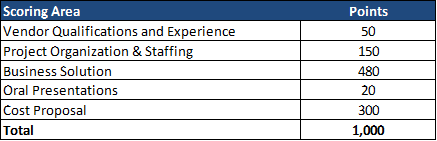
The winning MCO will be chosen based on the highest score of a possible total 1,000 points. The technical evaluation will be a total of 700 of 1,000 points. Cost represents 300 of 1,000 total points.
HMA Roundup
Arizona
Arizona Receives Federal Approval of Section 1115 Waiver to Address Housing Needs. The Centers for Medicare & Medicaid Services (CMS) announced on October 14, 2022, approval of the Arizona Health Care Cost Containment System Section 1115 waiver through September 30, 2027. The waiver’s Housing and Health Opportunities program will provide services to support stable housing, housing for individuals transitioning out of institutionalized care, and up to six months of rent and temporary housing for individuals moving from congregate settings, homeless shelters, or the child welfare system. Read More
California
California Faces Two Additional Public Records Act Lawsuits. Health Payer Specialist reported on October 14, 2022, that Centene/Health Net and Community Health Group Partnership Plan have filed separate state lawsuits to require the California Department of Health Care Services (DHCS) to release documents related to the state’s recent Medicaid managed care procurement. Community Health Group also requested that the awards process be paused indefinitely. Blue Shield of California also filed a public records act lawsuit against DHCS. Read More
District of Columbia
District of Columbia Council Approves Medicaid Managed Care Contracts. The Washington Post reported on October 18, 2022, that the District of Columbia City Council voted to approve Medicaid managed care contract awards to MedStar Family Choice, AmeriHealth Caritas, and Elevance Health/Amerigroup. DC Contract Appeals Board judges had already ruled that the procurement process was fair. The contracts are worth more than $8 billion and will run for five years. Read More
Florida
Florida Can Continue to Block Medicaid Coverage of Transgender Care for Now, Judge Rules. Health News Florida/News Service of Florida reported on October 13, 2022, that U.S. District Judge Robert Hinkle denied a preliminary injunction that would have prevented Florida from blocking Medicaid coverage of gender-affirming treatments for transgender individuals. The trial is scheduled for August 2023. Read More
Florida Levies $23 Million in Medicaid Managed Care Compliance Actions, Sanctions in Fiscal 2021. Florida Politics reported on October 13, 2022, that the Florida Agency for Health Care Administration levied more than $23.1 million in Medicaid managed care compliance actions and sanctions in fiscal 2021. Centene’s Sunshine Health Plan and StayWell Health Plan had combined liquidated damages and sanctions of nearly $17 million levied against them. Read More
Idaho
Idaho Delays Behavioral Medicaid Awards to November 2022. Health Payer Specialist reported on October 17, 2022, that Idaho has delayed the award announcement for the Idaho Behavioral Health Plan contract a month until November. Bidders include incumbent United/Optum, as well as Elevance/Beacon Health and Centene/Magellan Healthcare. The contract, which will serve about 51,000 individuals, will run for four years, with four years of renewal options. Read More
Illinois
Illinois Fines Health Plan for Violating Parity, Network Adequacy Laws. Health News Illinois reported on October 19, 2022, that the Illinois Department of Insurance (IDOI) fined Centene/Celtic Insurance Company $1.25 million for failing to comply with federal law requiring equivalent levels of coverage for mental health and substance use disorder compared to medical or surgical care by its Exchange plans from 2018 to 2020. IDOI also found that Celtic violated network adequacy requirements mandated by state law. Read More
Indiana
Indiana Awards Medicaid FFS Prior Authorization, Utilization Management Contract to Kepro. The Indiana Department of Administration announced on October 4, 2022, its intent to award a contract for Medicaid fee-for-service prior authorization and utilization management services to Keystone Peer Review Organization (Kepro). Gainwell Technologies, Maximus, and Telligen also submitted proposals. The contract will run for four years and is valued at nearly $30 million. Read More
Kansas
Kansas, Gainwell Implement Modular Medicaid Technology Platform. Gainwell Technologies announced on October 18, 2022, the implementation of a modular, cloud-based Medicaid technology platform for Kansas. The platform features automated administration of enrollment and managed care information, predictive analytics, and fraud prevention. Read More
Kentucky
Kentucky Seeks Section 1115 Waiver Extension for Substance Use Disorder Treatment, Foster Child Care. The Centers for Medicare & Medicaid Services announced on October 14, 2022, that Kentucky submitted a five-year extension request for the state’s KY HEALTH Section 1115 waiver demonstration to increase access to substance use disorder treatment and extend Medicaid coverage for former foster care youth under age 26. If approved, the waiver would run from October 1, 2023, to September 30, 2028. Public comments will be accepted through November 13, 2022. Read More
Michigan
Michigan Seeks Federal Approval of Section 1115 Family Planning Waiver. Michigan announced on October 10, 2022, submission for federal approval of a Section 1115 waiver demonstration to offer free contraception, cancer screenings, STI/STD testing, and other family planning services to 25,000 Michiganders. The waiver, called “Plan First,” is projected to save individuals up to $2,000 annually. Read More
Nebraska
Nebraska Announces Medicaid Provider Awards. The Nebraska Department of Health and Human Services announced on October 13, 2022, the winners of the state’s Medicaid Provider Awards for contributions to the Medicaid program and commitment to improving the health of their community. This year’s awards went to Narayana Koduri, MD, of Healthy Blue of Nebraska; Heidi Barker, DO, of Nebraska Total Care; Mark Darby, RN, of UnitedHealthcare Community Plan; and David J. Millea, DDS, of MCNA. Read More
New Hampshire
New Hampshire Requests Extension of IMD Exclusion Waiver. The Centers for Medicare & Medicaid Services announced on October 17, 2022, the New Hampshire Department of Health and Human Services submitted for federal approval a Section 1115 waiver extension request to continue providing covered substance use disorder, serious mental illness, and other behavioral health services to individuals who are short-term residents in institutions of mental disease. The request would also implement a community reentry program. Public comments will be accepted through November 16, 2022. Read More
Nevada
Nevada Governor Tells SEIU He Will Push for Higher Payment Rates, Wages for Home Care Providers. The Nevada Appeal reported on October 16, 2022, that Nevada Governor Steve Sisolak intends to recommend raising the Medicaid reimbursement rate for home care services to $25 and implementing a $15 per hour minimum wage for home care providers. The comments were made to members of the Service Employees International Union (SEIU). Read More
New York
New York Fails to Follow Up on Dual Eligible Cost Savings Opportunities, Comptroller Finds. New York State Comptroller Thomas DiNapoli announced on October 14, 2022, that the state failed to follow up on cost savings recommendations for dual eligibles and on improper payments for individuals with more than one Medicaid identification number. The dual eligible cost savings recommendations, released in a prior audit from the Comptroller’s office, found that “New York’s current Medicaid payment rules for recipients also covered by Medicare Part C cost-sharing liabilities have significantly higher costs compared to the allowable alternatives.” Read More
Pennsylvania
Pennsylvania Senate Committee Passes Resolution to Study Medicaid Addiction Treatment Reimbursement Rates. The Sharon Herald reported on October 18, 2022, that the Pennsylvania Senate Health and Human Services Committee passed a resolution to order a study of Medicaid reimbursement rates for addiction treatment services. The study, which would aim to determine if rates are keeping up with increased demand, would be conducted by the Joint State Government Commission in 2023. Read More
National
HHS Offers States Certified Community Behavioral Health Clinic Planning Grants. The Associated Press reported on October 18, 2022, that the U.S. Department of Health and Human Services (HHS) announced an opportunity for 15 states to receive $1 million planning grants in 2023 to develop certified community behavioral health clinics (CCBHCs). Of the states awarded planning grants, 10 will be included in the CCBHC demonstration program in 2024. HHS already awarded $300 million in grants directly to CCBHCs in September 2022. Read More
U.S. Supreme Court Declines to Hear Appeal from Molina Healthcare in False Claims Lawsuit. Modern Healthcare reported on October 18, 2022, that the U.S. Supreme Court has declined to hear an appeal from Molina Healthcare in a whistleblower lawsuit alleging that the Medicaid insurer charged Illinois and the federal government for nursing home services it did not provide. A provider group filed the False Claims Act lawsuit in 2017 in the U.S. District Court for the Northern District of Illinois, and the court dismissed the case in June 2020. In August 2021, the U.S. Court of Appeals for the 7th Circuit reversed the lower court’s decision and ordered the case be sent back to the district court. Read More
Medicare Advantage Plan Faces Federal False Claims Lawsuit. Modern Healthcare reported on October 17, 2022, that the Justice Department filed a federal false claims lawsuit against Cigna for allegedly submitting invalid diagnoses for its Medicare Advantage members between 2012 and 2019. A similar whistleblower lawsuit was filed against Cigna in 2017. Read More
Exchange Enrollment Hits 16.9 Million in Early 2022. Kaiser Family Foundation reported on October 17, 2022, that Exchange enrollment was 16.9 million in early 2022, up 20 percent since 2020, driven by enhanced subsidies, increased outreach, and an extended enrollment period. Enhanced subsidies will continue through 2025. Read More
CMS Releases RFI on National Directory of Healthcare Providers, Services. The Centers for Medicare & Medicaid Services (CMS) released on October 17, 2022, a request for information (RFI) on the creation of a National Directory of Healthcare Providers and Services (NDH). The NDH would act as a centralized data hub aimed at improving interoperability, patient choice, care coordination, and administrative efficiency. The public comment period will be open through December 6. Read More
CMS Releases FAQ on Eligibility Redeterminations, Addresses Optional COVID-19 Eligibility. The Centers for Medicare & Medicaid Services released on October 17, 2022, a set of frequently asked questions (FAQ) concerning eligibility redeterminations following the end of the public health emergency. CMS also provided information related to coverage and redetermination for individuals in the optional COVID-19 eligibility group, which expanded access to Medicaid coverage for COVID-related services to uninsured individuals. Read More
CMS Announces Grants Available for American Indian/Alaska Native Outreach, Enrollment. The Centers for Medicare & Medicaid Services (CMS) announced on October 17, 2022, grants available to help with outreach and enrollment for American Indian/Alaska Native individuals on Medicaid and the Children’s Health Insurance Program (CHIP). Funding is limited to Indian Health Service providers, tribes, or tribal entities. Applications are due by December 20, 2022. Read More
CMS Agrees to Release Audits of 90 Medicare Advantage Plans. Kaiser Health News (KHN) reported on October 14, 2022, that the Centers for Medicare & Medicaid Services (CMS) has agreed to release the audits of 90 Medicare Advantage (MA) plans in response to a lawsuit filed by the Kaiser Health Network. The Risk Adjustment Data Validation audits, conducted from 2011 to 2013, are expected to reveal more than $600 million in overpayments to Medicare plans. Read More
Biden Calls for Payment, Delivery Models That Reduce Drug Costs. Fierce Healthcare reported on October 14, 2022, that President Biden issued an executive order directing federal regulators to report on payment and delivery models that could improve access to innovative therapies and lower drug costs for Medicare and Medicaid beneficiaries. The models will be tested by the Center for Medicare and Medicaid Innovation. Read More
USDA Awards $110 Million in Rural Healthcare Grants. Fierce Healthcare reported on October 14, 2022, that the U.S. Department of Agriculture (USDA) awarded $110 million in grants to 208 organizations for infrastructure improvements at rural hospitals and clinics. Funding will go toward telehealth and nutrition assistance programs, staffing for COVID-19 vaccination and testing, construction and renovation of facilities, and medical supplies. The grant recipients serve five million individuals across 43 states and Guam. Read More
HHS Extends Public Health Emergency Another 90 Days. Reuters reported on October 13, 2022, that the U.S. Department of Health and Human Services (HHS) has extended the COVID-19 public health emergency by another 90 days to January 2023. President Biden also requested $22.4 billion from Congress to prepare for a potential winter surge in COVID cases. Read More
Industry News
Acorn Health Acquires 7 Applied Behavior Analysis Centers in FL, VA For Children With Autism. Acorn Health announced on October 18, 2022, the acquisition of six applied behavior analysis centers in Florida and one in Virginia for children diagnosed with autism spectrum disorder. The acquisition brings Acorn Health to 14 locations in Florida and 13 in Virginia. Read More
Centene to Offer Exchange Plans in AL in 2023. Becker’s Payer Issues reported on October 17, 2022, that Centene/Ambetter Health will offer Exchange plans in Alabama in 2023 as well as in 60 additional counties in the 12 states where it already offers Exchange plans. Centene/Ambetter will also expand its Virtual Access individual plan option into nine new states. Read More
Elevance/Anthem BCBS to Expand WI Exchange Offerings. Elevance’s Anthem Blue Cross Blue Shield plan in Wisconsin announced on October 17, 2022, that it is expanding Exchange options from nine to 68 counties in 2023. Anthem has also created a dedicated Wisconsin support center for health navigators assisting individuals with choosing health plans. Enrollment begins on November 1 and runs through January 15, 2023. Read More
Humana to Provide Dual Eligible Plan Members With Allowances for Social Needs, Dental Benefits in 2023. Humana announced on October 17, 2022, dual eligible enrollees in Florida will receive a monthly allowance of $150 to $275 for social needs, including groceries, gas, utilities, and rent. Members will also receive a yearly dental allowance up to $6,000. Additionally, Humana expanded dental benefits and provider networks for its 2023 Medicare Advantage plans in Florida. Read More
Brave Health Secures $40 Million in Latest Funding Round to Expand Virtual Medicaid Behavioral Health Services. Fierce Healthcare reported on October 12, 2022, that Brave Health, a virtual behavioral health provider serving Medicaid beneficiaries, has secured $40 million in its latest round of funding led by Town Hall Ventures. Existing investors Union Square Ventures and City Light Capital also participated in the round. Brave Health offers its service in 18 states. Read More
Essentia Health, Marshfield Clinic Health System Consider Merger. Essentia Health and Marshfield Clinic Health System announced on October 12, 2022, that they are evaluating a potential merger. The combined organization would have a network of 3,800 providers serving more than two million individuals in rural and mid-urban communities through more than 150 sites, including 25 hospitals. Read More
RFP Calendar
HMA News & Events
HMA WELCOMES
Holly Michaels Fisher, Principal – New York, NY
Holly Michaels Fisher is an accomplished healthcare executive, consultant, and thought leader specializing in Medicare, Medicaid, Special Needs Plans (SNPs), Medicare integration for dual eligibles, and Medicaid long-term services and supports and home and community-based services. She has deep industry experience in many areas including but not limited to Medicare/Medicaid managed care product innovation and development, Medicare bid and product strategy, and clinical program/product planning and operational design
Holly has a successful track record of building and leading SNPs, pioneering innovative specialized home and community-based services and managed care products; building, leading, and/or consulting to Medicare and Medicaid health plans; developing strategies to improve care management of Medicare and Medicaid members, impact Medicare Advantage Star and Medicaid quality performance; and developing and executing network design and contracting strategies to impact financial and clinical outcomes.
Most recently, Holly was the architect of Aetna’s significant DSNP expansion, expanding from two states to 30 states and from 20,000 members to more than 180,000 in less than four years. Prior to this, she was a managing director with PricewaterhouseCoopers where she provided management consulting services to national and regional Medicare and Medicaid health plans, specializing in operations and performance improvement related to medical management, clinical program design, network strategy, and Stars/quality.
Holly held a number of positions with UnitedHealth Group including executive director for Evercare in New York and New Jersey and as vice president and managing director for OptumInsight. At Evercare, a Medicare Advantage Institutional Special Needs Plan, she led a product turn around and managed the skilled nursing home network for all UnitedHealth Care lines of business. While at OptumInsight, Holly helped build and co-manage a consulting practice focused on Medicare, Medicaid, Special Needs Plans, Stars, and care management and utilization management programs for complex populations.
Holly has held leadership positions in several Medicare and Medicaid managed care plans in New York State including EmblemHealth, Universal American, Centerlight, and the Visiting Nurse Service of New York (VNS). At EmblemHealth she led the carrier’s Medicare and Medicaid lines of business. At Universal American, she led a subsidiary organization that worked for states providing care management services for complex Medicaid beneficiaries, was president of a newly acquired Medicaid plan, and managed Medicare for the northeast region. At Centerlight, Holly was CEO for what was then the largest PACE organization in the country with 14 locations and more than 2,300 members. With VNS, among other accomplishments as the vice president for Long Term Care and vice president for Program Development, she founded the first managed long-term care program in New York State (VNS CHOICE) for which she served as the first executive director from its founding in 1998 until 2005.
Holly earned her undergraduate degree in nursing and master’s degrees in public health administration and urban planning, all from Columbia University.
Helena Lefkow, Senior Consultant – Chicago, IL
Helena Lefkow is seasoned at identifying the practical implications of Medicaid law, regulation, and policy on hospital and health systems revenue cycle operations. She has extensive experience working with state agencies, health plans, associations, and other stakeholders to resolve Medicaid managed care and commercial payer billing and payment issues.
Prior to joining HMA, Helena served as senior director of Managed Care Policy at the Illinois Health and Hospital Association (IHA), where she was responsible for developing legislation, policy positions, and advocacy strategies to address a wide range of government and commercial managed care payer issues. In this role, she helped craft meaningful legislation to reform the Medicaid managed care program and secure telehealth coverage for commercially insured Illinoisans. She worked closely with state agencies and health plans on the implementation of new laws and regulations affecting hospitals and health systems, including the development of administrative rules on Illinois’ Medicaid managed care provider dispute resolution process and hospital readmission policies.
Helena also oversaw IHA’s Patient Financial Services program, which provides hospitals and health systems with current information on regulatory and administrative changes affecting revenue cycle operations; a forum for sharing best practices and addressing collective revenue cycle concerns; and technical assistance on a variety of Medicare, Medicaid, and private payer billing and payment issues. In this role, she led IHA’s efforts to resolve hospital billing and Medicaid managed claims processing errors, which led to creation of a comprehensive billing manual for hospital services and helped reduce the claim denial rate from 10 percent in 2018 to 5 percent in 2020.
Helena received a Master of Public Affairs, with a concentration in health policy, from the University of Wisconsin-Madison, and a bachelor’s degree in history from Northwestern University. She has served as a member of the Illinois Workers’ Compensation Medical Fee Advisory Board and the Illinois Child Welfare Advisory Committee convened by the Illinois Department of Healthcare and Family Services.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Colorado RAE Enrollment is Up 4%, Jun-22 Data
- Mississippi Medicaid Managed Care Enrollment is Down 11.8%, Sep-22 Data
- Nebraska Medicaid Managed Care Enrollment Is Up 6.2%, Jul-22 Data
- South Carolina Medicaid Managed Care Enrollment is Up 3.1%, May-22 Data
- South Carolina Dual Demo Enrollment is Down 6.7%, May-22 Data
- Tennessee Medicaid Managed Care Enrollment is Up 3.3%, Jul-22 Data
- Virginia Medicaid Managed Care Enrollment is Up 5.9%, Jun-22 Data
- Virginia Medicaid MLTSS Enrollment is Up 2.7%, Jun-22 Data
- West Virginia Medicaid Managed Care Enrollment is Up 3.1%, Jul-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- California Fiscal Intermediary for Dental Business Operations RFP and Proposals, 2021-22
- California Medi-Cal Managed Care Two-Plan, GMC, and Regional Models RFP, Proposals, Evaluation, Awards, Appeals and Responses, Oct-22
- Vermont HCBS Mental Health Urgent Care Services RFP, Oct-22
- West Virginia Medicaid Specialized Managed Care for Children, Youth RFP, Sep-22
Medicaid Program Reports, Data, and Updates:
- Alabama Medicaid Agency Annual Reports 2012-20
- Idaho CHIP Annual Reports to CMS, 2017-21
- Indiana CHIP Annual Reports to CMS, 2017-21
- Louisiana CHIP Annual Reports to CMS, 2017-21
- Maryland CHIP Annual Reports to CMS, 2017-21
- Texas Consolidated Reporting of Opioid-Use Disorder Related Expenditures, FY 2019-21
- Vermont Medicaid Program Enrollment and Expenditures Reports, SFY 2018-22
- Wyoming Medicaid PMPM Expenditures and Utilization Reports, SFY 2015-21
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
About HMA