HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: California First in Nation to Receive Federal Approval for Justice-Involved Reentry Demonstration Initiative

- California Awards $119 Million to 98 Organizations to Improve Medicaid Delivery System

- California Insurer to Offer Digital Health App to Medicaid Enrollees

- Iowa House Committee Advances Medicaid Work Requirements Bill

- Indiana Reaches $66.5 Million Settlement with Former PBM

- Michigan Releases Child, Adolescent Health Center Program RFP

- Minnesota Attorney General Asks for Delay of Sanford Health, Fairview Health Services Merger

- Mississippi Senator, Representative File Medicaid Expansion Bills

- North Carolina to Move Children Covered by CHIP to Medicaid

- New Mexico Cancels Medicaid Managed Care RFP

- South Dakota Legislators Propose Medicaid Expansion Fund

- Texas Awards STAR+PLUS Medicaid Managed Care Contracts to 7 Plans

- Utah Senate Passes Legislation to Extend Medicaid Dental Coverage

- CMS Proposes Updates to Medicare Advantage Risk Adjustment Model in 2024 Advance Notice

- CMS Will Not Impose Major Penalties on Medicare Advantage Plans for Overpayments

- CMS Outlines PHE Unwinding Requirements, Phase Out of FMAP Increase

- CVS Health Invests $32.7 Million in Affordable Housing in NC, TX

In Focus
California First in Nation to Receive Federal Approval for Justice-Involved Reentry Demonstration Initiative
This week, our In Focus section reviews the California amendment to the Section 1115 Waiver Demonstration titled, “California Advancing and Innovating Medi-Cal (CalAIM),” approved by the Centers for Medicare & Medicaid Services (CMS) on January 26, 2023. The amendment will provide targeted Medi-Cal services to individuals in state prisons, county jails, and youth correctional facilities for up to 90 days prior to release. This marks the first time in the nation that Medicaid will pay for a limited set of health care services provided to justice-involved individuals before they are released. The approval is effective through the end of the CalAIM demonstration, ending December 31, 2026, unless extended or amended.
The justice-involved initiative is part of the broader CalAIM demonstration, approved December 29, 2021. For more information on CalAIM, please see HMA’s write up from March 2021.
Background
California was one of the first of 11 states – Arizona, California, Kentucky, Massachusetts, Montana, New Jersey, New York, Oregon, Utah, Vermont, and Washington – to propose a demonstration to provide Medicaid-covered healthcare services to justice-involved populations before release. CMS plans to issue guidance on the Reentry Demonstration Opportunity to support community reentry and improvement in care transitions for individuals up to 30 days prior to their scheduled release.
California’s reentry demonstration initiative aims to address the needs of incarcerated beneficiaries as they near the end of their incarceration and reenter the community by improving connections and coordination between the correctional, health care, and social service systems. Currently, Medi-Cal services are only available after release from incarceration.
In California, more than one million adults and youth enter or are released from prisons and jails annually, with at least 80 percent eligible for Medi-Cal. The justice-involved individuals are disproportionately people of color, compared to the state population. Formerly incarcerated individuals are also more likely to experience poor health outcomes and face disproportionately higher rates of physical and behavioral health diagnoses. These individuals are at higher risk for injury and death as a result of violence, overdose, and suicide compared to people who have never been incarcerated.
Demonstration
California will be required to submit for CMS approval a Reentry Initiative Implementation Plan and Reinvestment Plan documenting how the state will operationalize coverage and provision of pre-release services and how existing state funding for carceral health services will continue to support access to necessary care and achievement of positive health outcomes for the justice-involved population.
The goals of the demonstration are to:
- “Increase coverage, continuity of coverage, and appropriate service uptake through assessment of eligibility and availability of coverage for benefits in carceral settings just prior to release;
- Improve access to services prior to release and improve transitions and continuity of care into the community upon release;
- Improve coordination and communication between correctional systems, Medicaid and CHIP systems, managed care plans, and community-based providers;
- Increase additional investments in health care and related services, aimed at improving the quality of care for beneficiaries in carceral settings and in the community to maximize successful reentry post-release;
- Improve connections between carceral settings and community services upon release to address physical health, behavioral health, and health-related social needs;
- Provide intervention for certain behavioral health conditions and using stabilizing medications like long-acting injectable anti-psychotics and medications for addiction treatment for SUDs, with the goal of reducing decompensation, suicide-related deaths, overdoses, and overdose-related deaths in the near-term post-release; and
- Reduce post-release acute care utilizations such as emergency department (ED) visits and inpatient hospitalizations and all-cause deaths among recently incarcerated Medicaid beneficiaries and individuals otherwise eligible for CHIP if not for their incarceration status through robust pre-release identification, stabilization, and management of certain serious physical and behavioral health conditions that may respond to ambulatory care and treatment (e.g., diabetes, heart failure, hypertension, schizophrenia, SUDs) as well as increased receipt of preventive and routine physical and behavioral health care.”
Eligible individuals under the demonstration will be assigned a care manager while they are incarcerated, as well as a community-based care manager upon their release. Pre-release services will be anchored in comprehensive care management and include physical and behavioral clinical consultation, lab and radiology, Medication Assisted Treatment (MAT), community health worker services, and medications and durable medical equipment. These services will be available for up to 90 days immediately prior to the individual’s expected release date. California expects that it will be able to reduce decompensation, suicide-related death, overdose, and overdose-related deaths in the near-term post-release.
As a condition of approval of this demonstration amendment, CMS is also requiring California to make pre-release outreach, along with eligibility and enrollment support, available to all individuals incarcerated in the facilities in which the demonstration is functioning. Effective January 1, 2023, state statute directs all counties implementing Medi-Cal application processes in county jails and youth correctional facilities to “suspend” their status while an individual is in jail or prison, and easily “turn on” when they enter the community so they can access essential health care services upon release.
The demonstration is expected to begin in April 2024. Correctional facilities can choose their launch date within 24 months of the go-live date and will be subject to a readiness review process before they can launch.
Additional Requirements
Under the amendment, CMS approved the state’s Designated State Health Program (DSHP) financing plan. Under this DSHP, California will receive federal matching funds to support the Providing Access and Transforming Health (PATH) program. As a condition of receiving this funding and as part of the approval, CMS requires California to increase and sustain Medicaid fee-for-service provider payment rates and Medicaid managed care payment rates for obstetrics, primary care, and behavioral health services. According to the U.S. Department of Health and Human Services (HHS), “in obstetrics alone, this represents the potential for $60 million to be invested in the health of pregnant and postpartum women by increasing access to providers and therein improving health outcomes for pregnant women.” The rate increase will close the gap between Medicaid and Medicare rates by at least 2 percentage points, should the state’s average Medicaid to Medicare provider rate ratio be below 80 percent in any of these categories.
Under this amendment, CMS is also updating the budget neutrality methodology for two previously approved community supports, short-term post-hospitalization services and recuperative care, that address health-related social needs.
HMA Roundup
California
California Awards $119 Million to 98 Organizations to Improve Medicaid Delivery System. The California Department of Health Care Services announced on January 31, 2023, awards of $119 million in grants to 98 organizations aimed at improving the state’s Medicaid delivery system. The funding will be used to increase the provider workforce, invest in infrastructure and information technology systems, conduct outreach to underserved communities, and more. Recipients of the Providing Access and Transforming Health Capacity and Infrastructure, Transition, Expansion, and Development grants include cities, counties, local government agencies, tribal entities, not-for-profits, public hospitals, and others. Read More
California Insurer to Offer Digital Health App to Medicaid Enrollees. Fierce Healthcare reported on January 26, 2023, that Blue Shield of California will offer its Wellvolution digital health program to Medicaid managed care enrollees. The app-based program, which was developed in collaboration with Solera Health, includes disease prevention, chronic condition reversal, mental health support, and tobacco cessation supports. Read More
California Medi-Cal Agreement to Reduce Number of Beneficiaries Who Have to Switch Plans. Kaiser Health News reported on January 27, 2023, that California’s decision to negotiate Medi-Cal managed care contracts outside its normal competitive bidding process will reduce the number of beneficiaries who have to switch plans from 2.3 million to 1.2 million, according to state officials. However, the process has raised concerns about the state’s resolve in standing up to insurers and driving through program improvements. Read More
Georgia
Georgia Governor Proposes $3 Million for Additional Staff to Help With Medicaid Redeterminations in Fiscal 2024 Budget. Now Habersham reported on January 29, 2023, that Georgia Governor Brian Kemp is proposing $3 million for additional caseworkers and administrative support for Medicaid redeterminations in his fiscal 2024 budget on top of the $8.4 million approved for fiscal 2023. Another $52 million would cover implementation of the Pathways to Coverage program in July, $14 million to keep individuals with intellectual and developmental disabilities from being institutionalized, and $13 million for three behavioral health crisis centers. Read More
Iowa
Iowa House Committee Advances Medicaid Work Requirements Bill. Iowa Public Radio reported on January 26, 2023, that the Iowa House Health and Human Services Committee advanced a bill that would implement Medicaid work requirements, including at least 20 hours of work or volunteering per week. Read More
Indiana
Indiana Reaches $66.5 Million Settlement with Former PBM. WTHR reported on January 31, 2023, that Indiana reached a $66.5 million settlement in a lawsuit alleging that Centene overcharged the state’s Medicaid program while serving as its pharmacy benefit manager (PBM). Centene will pay the sum in two installments over 12 months. Read More
Michigan
Michigan Releases Child, Adolescent Health Center Program RFP. The Michigan Department of Health and Human Services released on January 26, 2023, a request for proposals (RFP) to expand the state’s Child and Adolescent Health Center program through schools. The RFP is open to public and not-for-profit entities, including local health departments, community health centers, community mental health agencies, federally qualified health centers, and other health care or social services organizations. The five-month award runs from May 1 to September 30, and there is $12.1 million available, with maximum awards of $330,000. Responses are due on March 1. Read More
Minnesota
Minnesota Governor Proposes $17 Million for MinnesotaCare Public Option in Fiscal 2024-25 Budget. The Minnesota Department of Human Services reported on January 31, 2023, that Governor Tim Walz is proposing $17 million over two years to create a MinnesotaCare public option. The funds, which are included in Walz’ fiscal 2024-25 budget proposal, would be aimed at expanding comprehensive health insurance options for people who struggle to afford private coverage, including the state’s nearly 300,000 uninsured. Walz is also proposing continuous Medicaid eligibility for children under age six, a 50 percent increase in the rate for adult day treatment for group therapeutic services, and expanding mobile crisis services. Read More
Minnesota Attorney General Asks for Delay of Sanford Health, Fairview Health Services Merger. Modern Healthcare reported on January 26, 2023, that Minnesota Attorney General Keith Ellison has asked Sanford Health and Fairview Health Services to delay their $14 billion merger pending an investigation into its consequences. Originally, the deal was expected to close by March 31. Read More
Mississippi
Mississippi Representative Files Bills to Extend Postpartum Medicaid Coverage from 60 Days to 12 Months. Super Talk Mississippi Media reported on January 30, 2023, that Mississippi Representative Missy McGee (R-Hattiesburg) filed two bills to extend postpartum Medicaid coverage from 60 days to 12 months and to allow pregnant women to be deemed presumptively eligible for ambulatory prenatal care under Medicaid for up to 60 days. Approximately 65 percent of births in Mississippi are covered by Medicaid annually. Read More
Mississippi Senator, Representative File Medicaid Expansion Bills. Mississippi Today reported on January 26, 2023, that Mississippi Senator Angela Turner Ford (D-West Point) and Representative Bryant Clark (D-Pickens) have separately filed Medicaid expansion bills (Senate Bill 2070, House Bill 108) for the current session. Multiple bills have also been filed to extend postpartum Medicaid coverage from 60 days to 12 months. Read More
North Carolina
North Carolina to Move Children Covered by CHIP to Medicaid. The Winston-Salem Journal reported on January 30, 2023, that North Carolina is joining 17 other states in moving children covered by NC Health Choice, the state’s Children’s Health Insurance Program (CHIP) to Medicaid. The change, which will be effective April 1, will impact 55,000 children statewide. The fiscal 2023 budget included a provision for the shift. Read More
Nebraska
Nebraska Hospital Groups Urge Lawmakers to Pass Medicaid Payment Increase Legislation. The Omaha World Herald reported on January 31, 2023, that representatives from the Nebraska Hospital Association and Nebraska Rural Health Association urged the state legislature to pass a bill that would increase Medicaid payments for hospitals by 9.6 percent in fiscal 2024 and 7.7 percent in fiscal 2025. Nebraska lawmakers are also considering bills to increase interim payment rates for rural hospitals and to raise payment rates for inpatient psychiatric care and rehabilitation services. Read More
New Mexico
New Mexico Cancels Medicaid Managed Care RFP. The New Mexico Human Services Department announced on January 30, 2023, the cancellation of its Turquoise Care Medicaid managed care procurement, which serves 800,465 members. The request for proposals (RFP), which was issued in September 2022, was cancelled so the agency’s new leadership can assess the design of the procurement given the planned departures of both Secretary David Scrase and the Medicaid Director Nicole Comeaux. Current contracts, which are set to expire at the end of 2023, will continue until a new, expedited RFP is issued. A notice of intent to award was scheduled for January 16 and the final awards for March 22. Read More
New York
New York Health Plan Announces Grants to Increases Access to Community Health Workers at FQHCs. UnitedHealthcare Community Plan of New York announced on January 30, 2023, $750,000 in grants aimed at increasing access to community health workers at federally qualified health centers (FQHCs). The program is in collaboration with the Community Health Care Association of New York State. Read More
Ohio
Ohio Medicaid Managed Care Contracts Take Effect. The Ohio Department of Medicaid announced on February 1, 2023, that Next Generation Medicaid managed care contracts took effect, including enhanced features like individualized care management, 12 months of postpartum coverage, behavioral health services for children, a statewide crisis line, and telehealth
South Dakota
South Dakota Legislative Committee Advances Medicaid Work Requirements Constitutional Amendment. Fox News reported on January 30, 2023, that the South Dakota House of Representatives State Affairs Committee advanced a constitutional amendment to institute Medicaid work requirements. The amendment, which would appear on the 2024 general election ballot, now moves to the full House. Read More
South Dakota Legislators Propose Medicaid Expansion Fund. The Argus Leader reported on January 27, 2023, that South Dakota legislators introduced a bill to create a $54 million Medicaid expansion fund, which would cover almost 81 percent of the estimated cost of the state’s share of expansion in fiscal 2024. Read More
Texas
Texas Awards STAR+PLUS Medicaid Managed Care Contracts to 7 Plans. The Texas Health and Human Services Commission (HHSC) announced on January 27, 2023, its intent to award contracts for its STAR+PLUS Medicaid managed care program, which serves aged, blind, and disabled populations, to incumbents United Healthcare Community Plan of Texas, Molina Healthcare of Texas, Centene/Superior HealthPlan, and Elevance/Amerigroup Insurance Company, as well as Community First Health Plans, El Paso Health, and Community Health Choice Texas. Plans with existing dual-eligible special needs plan (D-SNP) contracts must apply to the Centers for Medicare & Medicaid Services for a 2024 service area expansion by February. STAR+PLUS contracts require that plans have a companion D-SNP covering the entirety of their STAR+PLUS service area. Contracts are anticipated to begin in February 2024. Please see data package below for awards by regions. Read More
Texas MCO Overstated $1.5 Million in Expenses in 2020, Audit Finds. The Texas Health and Human Services Office of the Inspector General announced on January 24, 2023, that Molina Healthcare of Texas overstated more than $1.5 million of expenses on its 2020 combined financial statistical report (FSR). The managed care organization (MCO) inaccurately reported 43 percent of its expenses and included costs that should not have been in the FSR. Read More
Utah
Utah Senate Passes Legislation to Extend Medicaid Dental Coverage. State of Reform reported on January 26, 2023, that the Utah Senate passed legislation to pursue waivers to extend Medicaid coverage of dental services to adults age 21 and up. The bill, which now heads to the House, would extend coverage to approximately 130,000 individuals. Read More
West Virginia
West Virginia Committees Advance Opioid Use Disorder, SUD Treatment Legislation. The Weirton Daily Times reported on February 1, 2023, that the West Virginia House Health and Human Resources Committee advanced a bill that would remove certificate of need requirements from opioid treatment programs like methadone clinics. Separately, the Senate Health and Human Resources Committee advanced a bill that would make residential substance use disorder (SUD) service programs subject to existing behavioral health licensing rules. Read More
Wyoming
Wyoming Legislature Considers 20 Mental Health, Related Bills. WyoFile reported on January 27, 2023, that at least 20 bills impacting mental health care have been submitted to the Wyoming legislature in 2023. Proposed legislation includes suicide call center support, Medicaid expansion, mental health provider licensing requirements, school-based mental health services, and extensions of postpartum Medicaid coverage. Read More
National
CMS Proposes Updates to Medicare Advantage Risk Adjustment Model in 2024 Advance Notice. The Centers for Medicare & Medicaid Services (CMS) released on February 1, 2023, its 2024 Advance Notice for the Medicare Advantage (MA) and Part D Prescription Drug Programs, proposing technical updates to the MA risk adjustment model. The notice also outlines updates to the Part D program that go into effect on January 1, 2024, including the continuation of reduced cost-sharing for insulin; eliminated cost-sharing for recommended, preventive vaccines; the elimination of cost-sharing for Part D prescription drugs in the catastrophic phase; and expansion of eligibility for full cost-sharing and premium subsidies under the Low-Income Subsidy program. The public comment period is open until March 3. Read More
73 Percent of Dual Eligibles Qualified for Full Medicaid Benefits in 2020, KFF Analysis Finds. Kaiser Family Foundation (KFF) reported on January 31, 2023, that 73 percent of dual eligibles were eligible for full Medicaid benefits in 2020, including long-term services and supports, according to a KFF analysis. KFF also found that 87 percent had an income less than $20,000, almost 40 percent were under age 65 and eligible for Medicare due to a disability, and Medicare spending per dual eligible in traditional Medicare was substantially higher than per capita spending for other Medicare beneficiaries. Read More
Medicaid, CHIP Enrollment Exceeds 91 Million in October 2022. The Centers for Medicare & Medicaid Services (CMS) announced on January 31, 2023, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) topped 91.3 million in October 2022, an increase of more than 462,000 from September 2022. Medicare enrollment topped 65 million, up nearly 133,000 from September 2022, including 30.2 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. CMS also reported that more than 16.3 million individuals enrolled in Exchange plans during open enrollment. Read More
CMS Issues Rule to Claw Back Medicare Advantage Overpayments. CQ News reported on January 30, 2023, that the Centers for Medicare & Medicaid Services (CMS) released a final rule to claw back overpayments to Medicare Advantage (MA) plans. The rule will bring the same level of oversight and accountability to MA that is used in traditional fee-for-service Medicare, according to CMS. The agency is expecting to recoup more than $4 billion over the next 10 years. Read More
CMS Will Not Impose Major Penalties on Medicare Advantage Plans for Overpayments from 2011-17. Kaiser Health News reported on January 30, 2023, that the Centers for Medicare & Medicaid Services (CMS) announced it will not impose major financial penalties on Medicare Advantage (MA) plans that overcharged the federal government between 2011 through 2017. CMS will begin imposing extrapolated penalties after conducting audits for 2018 and beyond. Read More
CMS Outlines PHE Unwinding Requirements, Phase Out of FMAP Increase. The Centers for Medicare & Medicaid Services (CMS) announced on January 27, 2023, that states must initiate eligibility redeterminations for all Medicaid, Children’s Health Insurance Program, and Basic Health Program enrollees within 12 months of the state’s public health emergency (PHE) unwinding period, between April 1, 2023 and June 30, 2024, in order to continue receiving the temporary increase in the Federal Medical Assistance Percentage (FMAP). During the unwinding period, states must redetermine eligibility for all enrollees and submit monthly data about eligibility determination and redetermination activities to CMS. The FMAP increase will phased out by the end of 2023. Additionally, CMS announced a temporary Exceptional Circumstances Special Enrollment Period for individuals who lose coverage during the PHE unwinding period. Read More
US Legislators Introduce Bill to Enhance Medicaid HCBS Payments. McKnight’s Senior Living reported on January 27, 2023, that U.S. Senator Bob Casey (D-PA) and Representative Debbie Dingell (D-MI) introduced legislation that would increase Medicaid payments for home and community-based services (HCBS) providers. The bill seeks to address waiting lists totaling 650,000 for HCBS. Read More
US Legislators Introduce Bills to Regulate PBMs. Fierce Healthcare reported on January 27, 2023, that U.S. Senators Maria Cantwell (D-WA) and Chuck Grassley (R-IA) introduced legislation to regulate pharmacy benefit managers (PBMs) in part by preventing clawbacks on payments made to pharmacies and limiting fees used to offset the cost of reimbursed medicines. The legislation would also require that PBMs submit annual reports detailing pricing for health plans and payments to pharmacies. Read More
Most Individuals Disenrolled from Medicaid, CHIP Go Uninsured For All or Part of Next 12 Months, KFF Study Finds. Kaiser Family Foundation (KFF) reported on January 25, 2023, that 65 percent of individuals who are disenrolled from Medicaid or the Children’s Health Insurance Program (CHIP) go uninsured for all or part of next 12 months. Additionally, 41 percent of the disenrolled population re-enroll in Medicaid or CHIP coverage within a year. Read More
Industry News
CareSource Joins Walmart, J&J to Improve Black Maternal Health in GA. Health Payer Specialist reported on January 25, 2023, that CareSource formed a partnership with Walmart and Johnson & Johnson (J&J) to develop programs aimed at improving Black maternal health in Georgia. The programs will focus on digital solutions, health care provider education, and self-care support. Read More
CVS Health Invests $32.7 Million in Affordable Housing in NC, TX. Health Payer Specialist reported on January 25, 2023, that CVS Health is investing $32.7 million in affordable housing in Charlotte, NC; and Houston, TX. In 2022, the company invested $257 million in affordable housing across the United States. Read More
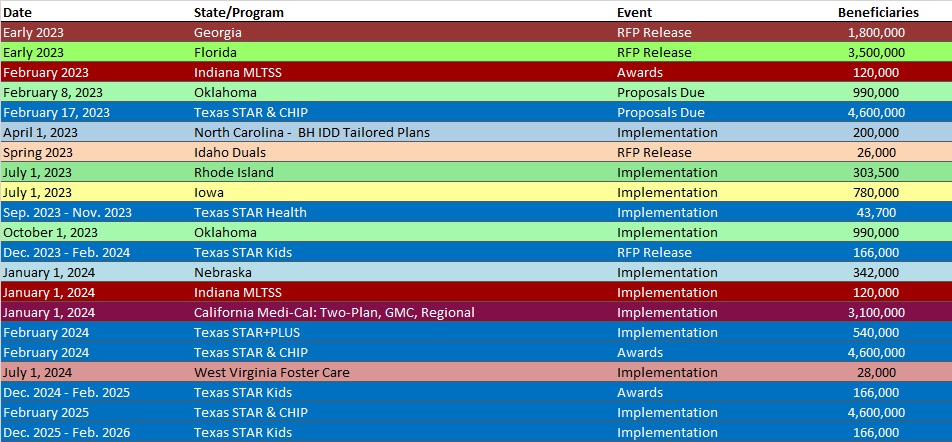
RFP Calendar
HMA News & Events
Health Management Associates acquires Lovell Communications and establishes Nashville office. Jay Rosen, founder, president, and co-chairman of Health Management Associates (HMA), today announced the firm’s acquisition of Lovell Communications, a leading strategic communications and change management firm that exclusively serves the healthcare industry. Read More
HMA LinkedIn Live
Growth and Opportunity in the ACA Marketplaces. The anticipated resumption of Medicaid redeterminations, the slowdown of new ACA entrants in 2023, and high-profile low-cost carrier exits has resulted in a significant marketplace enrollment opportunity for new entrants and incumbents. This conversation with Wakely Consulting Group‘s Karan Rustagi and Michelle Anderson will reflect on past ACA cycles to anticipate opportunities for payers in 2023 and beyond. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Indiana Medicaid Managed Care Enrollment Is Up 9.3%, Nov-22 Data
- Iowa Medicaid Managed Care Enrollment is Up 5.9%, Nov-22 Data
- Kansas Medicaid Managed Care Enrollment is Up 5.5%, Oct-22 Data
- Kansas SNP Membership at 19,158, Nov-22 Data
- Kentucky Medicaid Managed Care Enrollment is Up 5.7%, Nov-22 Data
- Kentucky SNP Membership at 76,297, Nov-22 Data
- Maine SNP Membership at 33,616, Nov-22 Data
- Massachusetts SNP Membership at 66,322, Nov-22 Data
- Michigan SNP Membership at 102,516, Nov-22 Data
- Minnesota SNP Membership at 54,204, Nov-22 Data
- Mississippi SNP Membership at 70,444, Nov-22 Data
- Montana SNP Membership at 4,061, Nov-22 Data
- North Dakota Medicaid Expansion Enrollment is Up 9.1%, Nov-22 Data
- North Dakota SNP Membership at 215, Nov-22 Data
- Puerto Rico SNP Membership at 312,128, Nov-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Florida Medicare Advantage D-SNP Contracts, 2023
- Idaho Medicare Advantage D-SNP Contracts, 2023
- Oregon Medicare D-SNP Contracts, 2023
- Pennsylvania Community HealthChoices Model Contract, 2018-23
- South Carolina Medicare Advantage D-SNP Model Contract, 2023
- Texas STAR, CHIP Managed Care RFP, Q&A, and Related Documents, 2022-23
Medicaid Program Reports, Data, and Updates:
- Louisiana Medicaid Financial Forecast Reports, SFY 2018-22
- Pennsylvania Medical Assistance Advisory Committee (MAAC) Meeting Materials, Jan-23
- Texas OIG Medicaid Health Plan Administrative and Medical Expense Audits, Aug-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
