This week our In Focus section reviews the Delaware request for proposals (RFP) for Diamond State Health Plan (DSHP) and Diamond State Health Plan Plus (DSHP Plus), the state’s Medicaid managed care programs. The RFP was released by the Delaware Department of Health and Social Services (DHSS), Division of Medicaid and Medical Assistance (DMMA) on December 15, 2021.
DSHP/DSHP Plus provides integrated physical, behavioral health, and longterm services and supports (LTSS) to approximately 280,000 members. Delaware intends to contract with two or three Medicaid managed care organizations (MCOs). Current incumbents are AmeriHealth Caritas and Highmark Health Options.
Background
DSHP provides coverage to individuals with incomes up to the 100 percent of the federal poverty level (FPL). In 2012, the state created DSHP Plus to include dual eligible, LTSS/nursing facility (NF), and Medicaid buy-in populations. Since then, the state has also added the former foster youth population to DSHP. In 2014, the state implemented the Promoting Optimal Mental Health for Individuals through Supports and Empowerment (PROMISE) program, which provides behavioral health benefits to Medicaid beneficiaries who have a severe and persistent mental illness (SPMI) and/or a substance use disorder (SUD) and require home and community-based services (HCBS).
DSHP/DSHP Plus operate under a Section 1115 waiver demonstration, with a current renewal effective until December 31, 2023. DSHP also includes the Delaware Healthy Children Program (DHCP), which covers uninsured children from birth to the age of 19 with a family income at or below 212 percent of the FPL. Families are required to pay a monthly premium.
RFP
Newly awarded MCOs will work with DMMA to achieve the following goals:
1. Member focus, including a. Providing whole person, person-centered care b. Engaging with communities c. Identifying, addressing health-related social needs d. Advancing health equity
2. Accountability
3. Innovation
4. Alignment with other state initiatives
MCOs are expected to be able to implement new Medicaid benefits (including doula services and respite services for children), implement value-based purchasing models, adopt practices to improve health equity, and implement projects addressing social determinants of health
Timeline
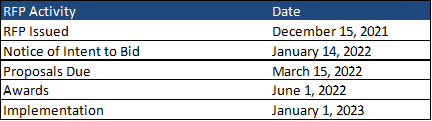
Contracts will be effective January 1, 2023 and run for five years with three optional one-year extensions. MCOs were encouraged to submit a notice of intent to bid by January 14; however, it was not a requirement nor an obligation to submit proposals. Proposals are due March 15, 2022, and awards are expected to be announced on June 1.
Evaluation
Proposals will be scored on seven topic areas, weighted as follows:
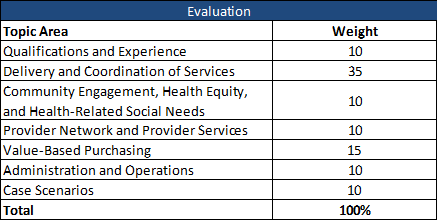
Following the initial scoring, bidders may be invited to make oral presentations, which will have a weight of 10.