This week, our In Focus section reviews the Hawaii QUEST Integration (QI) Medicaid Managed Care request for proposals (RFP), issued by the Hawaii Department of Human Services (DHS) on August 26, 2019. DHS intends to contract with four health plans. All four will serve Medicaid and Children’s Health Insurance Program (CHIP) members in Oahu, while two will also operate statewide. The two plans with the highest scoring technical proposals will serve beneficiaries statewide. The Quest Integration program is worth $2.2 billion annually.
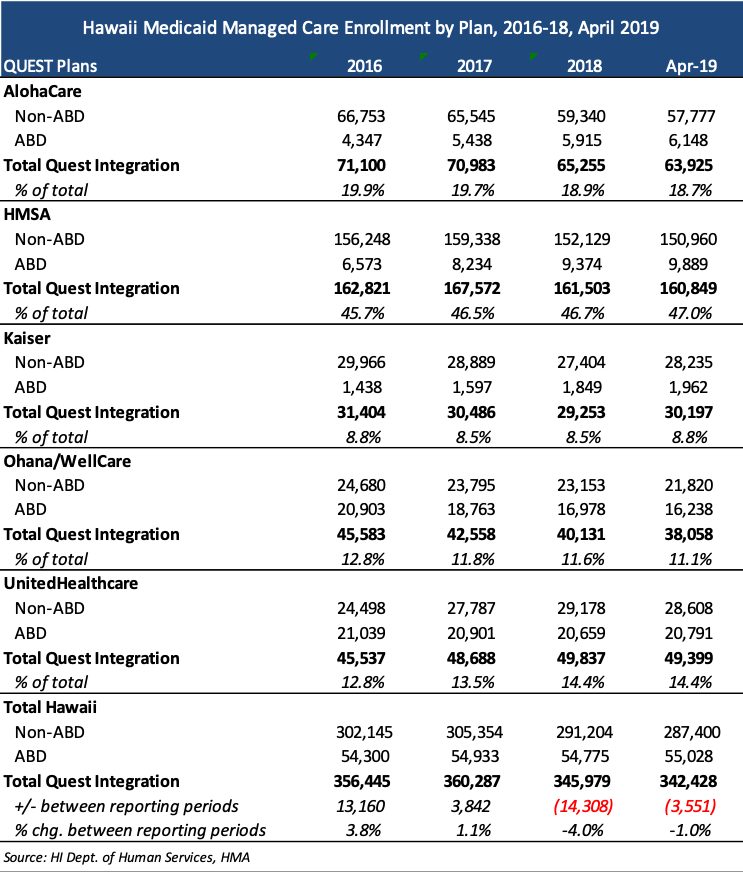
The QUEST program, which stands for Quality care, Universal access, Efficient utilization, Stabilizing costs, and Transforming the way health care is provided to QUEST members, first began in 1994. In 2009, the aged, blind, or disabled (ABD) population was transitioned to a managed care program called QUEST Expanded Access (QExA) and in January 2015, integrated into the program now known as Quest Integration, serving more than 342,000 individuals. Health plans will provide medical, behavioral health, and long-term services and supports (LTSS) services to covered populations, including CHIP, Foster Care, QUEST Family, Expansion, Childless Adults, Aged, and Blind/Disabled, and Medicaid-Medicare dual eligible members.
Hawaii `Ohana Nui Project Expansion (HOPE) Program
Under the RFP, Hawaii intends to implement the HOPE program, focusing on health and wellness. The program will invest in primary care, prevention, and health promotion; improve outcomes for individuals with special health care needs through care management; reform and align payment to providers; and support community-driven initiatives to improve population health. The five goals of the HOPE program are:
- Advancing primary care
- Supporting team-based care using a range of clinical providers and nonclinical providers, such as medical assistants, peer support specialists, and community health workers
- Implementing prevention and health promotion
- Implementing the stepped care approach to behavioral health. In a stepped care approach, individuals can move up or down a continuum of services as needed, with treatment level and intervention based on the level of the individual.
- Addressing Social Determinants of Health (SDOH)
Dual-Eligible Special Needs Plan (D-SNP)
Selected health plans will need to have an operational D-SNP by January 1, 2021. Medicare Improvements for Patients and Providers Act of 2008 (MIPPA) terms will be included in the QUEST Integration contract. Plans can also request to be a Fully Integrated Dual Eligible (FIDE) SNP beginning January 1, 2021.
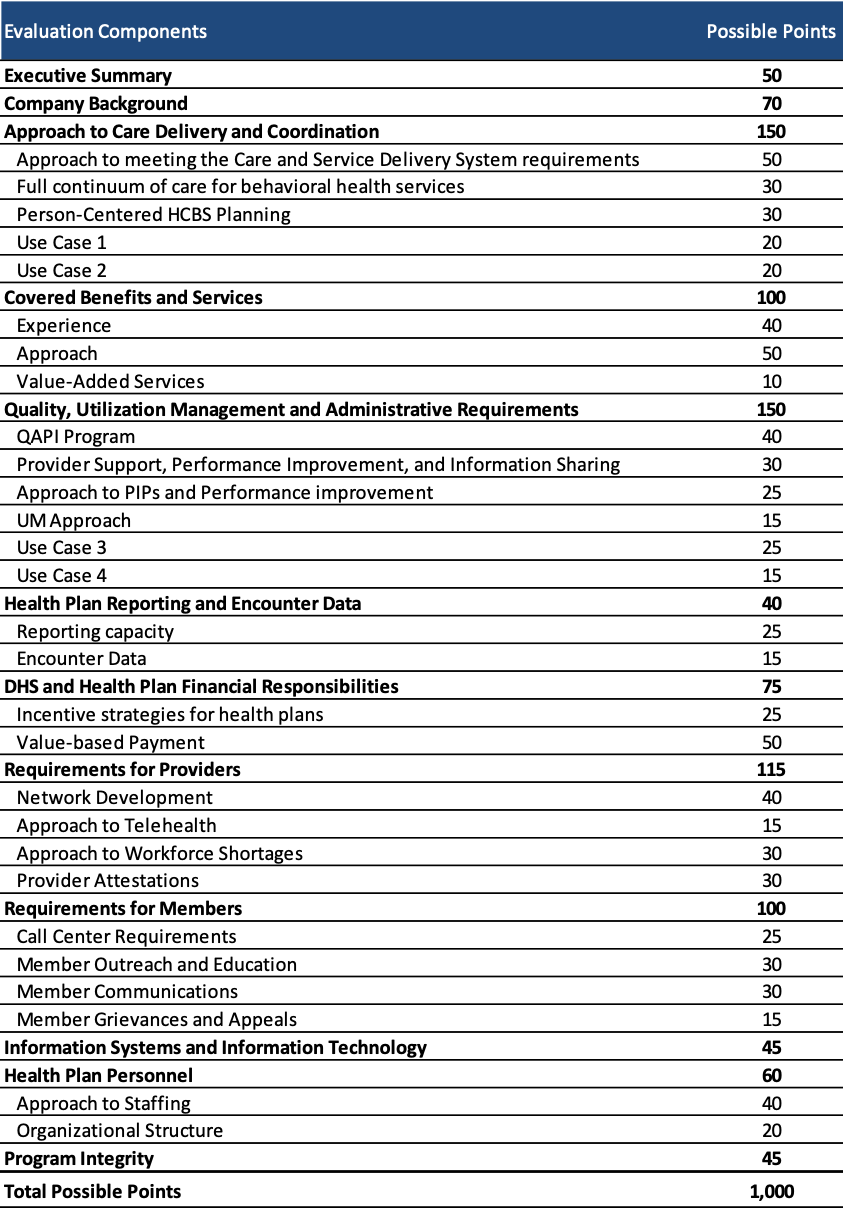
Evaluation
Technical proposals will be scored on a total of 1,000 possible points. To be considered responsive to the RFP, plans must score at least 750 points. Points are allocated to sections of the technical proposal as follows:
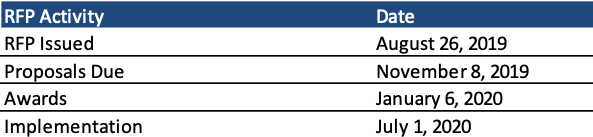
Timeline
Proposals are due November 8, 2019, and awards will be made on January 6, 2020. Implementation begins July 1, 2020, with contracts running through December 31, 2025, with four additional optional years.
Current Market
Current Medicaid incumbents are AlohaCare, HMSA, Kaiser, WellCare, and UnitedHealthcare, serving more than 342,000 individuals. HMSA (an independent licensee of the Blue Cross Blue Shield Association) has the largest market share, with 47 percent of current enrollment.