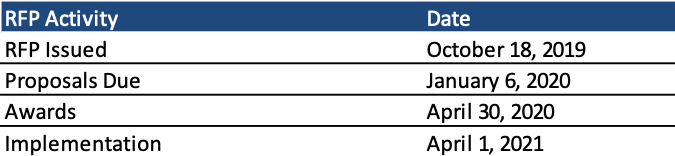
This week, our In Focus section reviews the Indiana Hoosier Care Connect request for proposals (RFP), issued by the Indiana Family and Social Services Administration (FSSA), Office of Medicaid Policy and Planning (OMPP) on October 18, 2019. Hoosier Care Connect is the state’s Medicaid managed care program for approximately 90,000 aged, blind, and disabled (ABD) Medicaid beneficiaries. Implementation is expected April 1, 2021, with contracts worth $1.4 billion annually.
Background
The Hoosier Care Connect program provides coordinated care to individuals who are aged 65 years and older, blind, or disabled and who are also not Medicare eligible and do not receive institutional care. Through the program, the state seeks to improve clinical and functional status, enhance quality of life, improve member safety, and enhance member autonomy and adherence to treatment plans for beneficiaries. Members complete a health screening to determine a level of need for care coordination. Medicaid managed care organizations (MCOs) are required to maintain a minimum Medical Loss Ratio (MLR) of 90 percent.
The program includes voluntary enrollment for foster care children, former foster care children, children receiving adoption assistance, and wards of the state. The state released a separate request for information (RFI) regarding a potential healthcare program or other options for eligible children and youth to receive Medicaid services.
Dual Eligible Special Needs Plans (D-SNPs)
MCOs will be required to operate a D-SNP statewide by April 1, 2022. The State Medicaid Agency Contract (SMAC) for calendar year 2022 must be submitted to the Centers for Medicare & Medicaid Services (CMS) by July 2021. CMS will issue SNP approval/denial notices in September 2021.
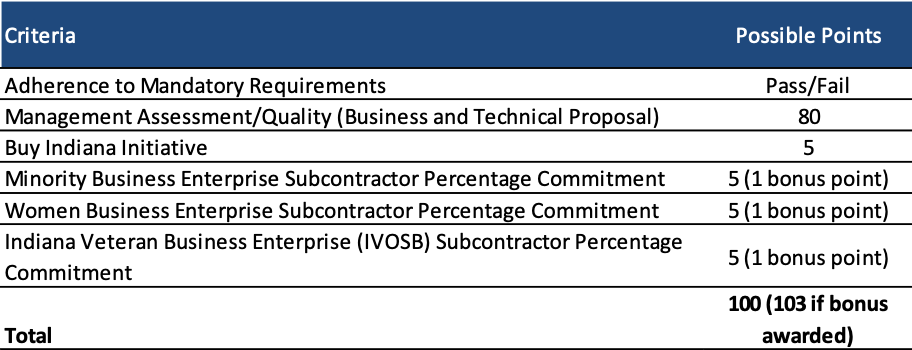
Evaluation
Proposals will be scored out of a total of 103 points, with the business and technical proposal worth 80 points. Indiana-based organizations will be awarded 5 points through the Buy Indiana Initiative.
Timeline
Proposals are due January 6, 2020, with award announcements expected on April 30, 2020. New contracts will run for four years beginning April 1, 2021, with two optional one-year renewals.
Current Market
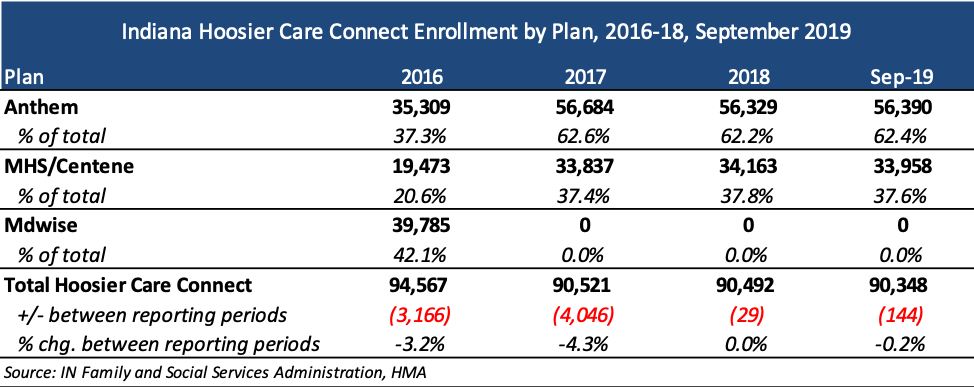
Incumbent health plans are Anthem and Managed Health Services (MHS)/Centene with approximately 56,000 and 34,000 members respectively.