This week, our In Focus section reviews updated information issued by the Department of Health & Human Services (HHS) Centers for Medicare & Medicaid Services (CMS) on Medicaid expansion enrollment from the “September 2018 Medicaid and CHIP Application, Eligibility Determination, and Enrollment Report,” published on November 30, 2018. Additionally, we review 2018 Exchange enrollment data from the “Health Insurance Marketplaces 2018 Open Enrollment Period: Final State-Level Public Use File,” published by CMS on April 3, 2018. Combined, these reports present a picture of Medicaid and Exchange enrollment in 2018, representing 73 million Medicaid and CHIP enrollees and nearly 12 million Exchange enrollees.
Key Takeaways from Medicaid Enrollment Report
- Across all 50 states and DC, Medicaid and CHIP enrolled nearly 73 million individuals as of September 2018.
- Medicaid and CHIP enrollment is down more than 1 million members since September 2017, a 1.6 percent decrease in enrollment.
- Since September 2017, 20 states saw positive percentage growth in Medicaid and CHIP. No states saw double digit growth. The highest growth was seen in Alaska (7.4 percent); Montana (5.1 percent); Connecticut (4.2 percent); Iowa (4.1 percent); and Alabama (2.4 percent). Virginia expansion has been signed into law and will be effective January 1, 2019. Maine, Nebraska, and Utah are also likely to expand in 2019.
- Over that same period, 31 states saw a net decline in Medicaid and CHIP enrollment.
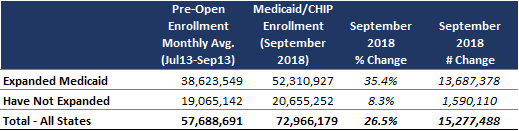
- As of September 2018, national Medicaid and CHIP enrollment is up nearly 15.3 million (26.5 percent) from the “Pre-Open Enrollment” period, defined as July 2013 through September 2013.
- The top five states in percentage growth of Medicaid and CHIP enrollment since the Pre-Open Enrollment period are Kentucky (102.3 percent), Nevada (93.9 percent), Montana (86.7 percent), Alaska (72 percent), and Colorado (70.9 percent). All five are Medicaid expansion states.
- The top five states in percentage growth of Medicaid and CHIP among states that did not expand Medicaid are North Carolina (27.4 percent), Idaho (16.3 percent), Georgia (14.9 percent), Florida (14.3 percent), and Alabama (13.9 percent).
- The top five states in total enrollment growth of Medicaid and CHIP are California (4.2 million), New York (829,752), Kentucky (620,467), Washington (616,424), and Colorado (555,696).
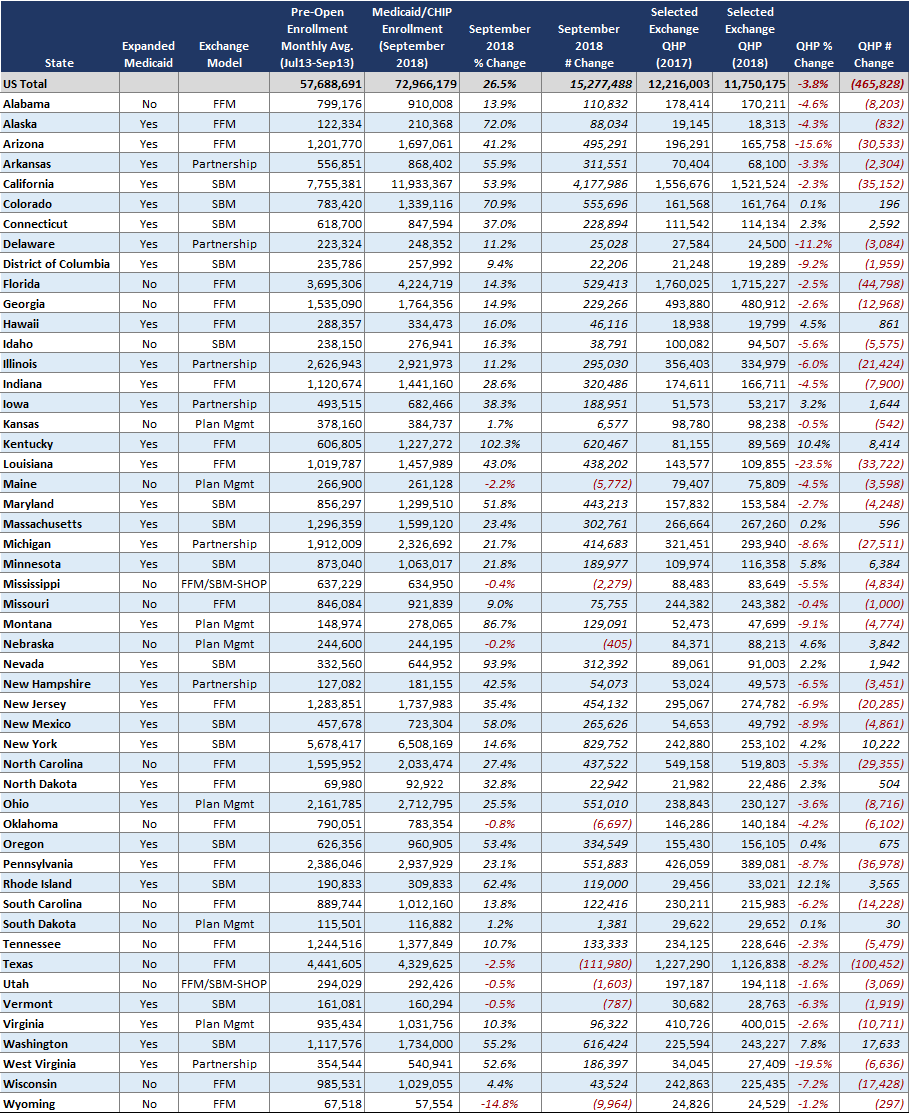
Table 1 – Overall U.S. Medicaid/CHIP Enrollment Growth – Pre-Open Enrollment Monthly Average through September 2018
Key Takeaways from 2018 Exchange Enrollment Report
- Final Exchange enrollments for the 2018 plan year, published in April 2018, showed that Qualified Health Plan (QHP) plans have been selected by nearly 11.8 million individuals across all 50 states and DC.
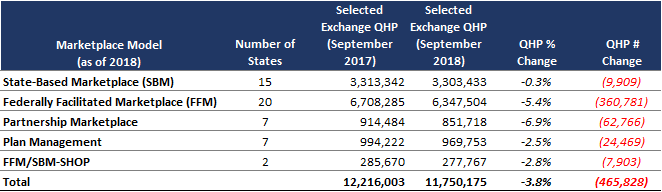
- 2018 QHP selections are down nearly 466,000 from 2017 QHP selections, a decline of 3.8 percent across all 50 states and DC.
- Only two states saw double-digit percentage growth in QHP selections – Rhode Island (12.1 percent), a State-Based Marketplace, and Kentucky (10.4 percent), a Federally Facilitated Marketplace.
- A total of 17 states saw declines in QHP selections between 0 percent and 5 percent. Another 15 states saw declines of 5 percent to 10 percent. A total of four states saw double-digit percentage declines in QHP selections from 2017 to 2018.
- Overall, all Exchange/Marketplace administration models saw declines in enrollment.
Table 2 – Overall U.S. Exchange QHP Selection Growth – 2017 through 2018
The table below (Table 3) provides state-level data on Medicaid and Exchange enrollment.
Medicaid and Exchange Enrollment Data Sources
Link to CMS Medicaid Expansion Enrollment Report:
Link to CMS Marketplace Open Enrollment Period Public Use Files:
“2018 Marketplace Open Enrollment Period Public Use Files” (April 2018)