This week, our In Focus section reviews Medicaid spending data collected in the annual CMS-64 Medicaid expenditure report. After submitting a freedom of information act request to CMS, we have received a draft version of the CMS-64 report that is based on preliminary estimates of Medicaid spending by state for federal fiscal year (FFY) 2017. The final version of the report will be completed by the end of 2018 and posted to the CMS website at that time. Based on the preliminary estimates, Medicaid expenditures on medical services across all 50 states and 6 territories in FFY 2017 exceeded $571 billion, with over half of all spending now flowing through Medicaid managed care programs. In addition, total Medicaid spending on administrative services was $27.8 billion, bringing total program expenditures to just under $600 billion.
Total Medicaid Managed Care Spending
Total Medicaid managed care spending (including the federal and state share) in FFY 2017 across all 50 states and 6 territories was $297 billion, up from $271 billion in FFY 2016. This figure includes spending on comprehensive risk-based managed care programs as well as prepaid inpatient health plans (PIHPs) and prepaid ambulatory health plans (PAHPs). PIHPs and PAHPs refer to non-comprehensive prepaid health plans that provide only certain services, such as dental services or behavioral health care. Fee-based programs such as primary care case management (PCCM) models are also counted in this total. However, comprehensive risk-based managed care organizations (MCOs) account for 95 percent of the total. Below we highlight some key observations:
- Total Medicaid managed care spending grew 9.5 percent in FFY 2017, the lowest year-over-year growth rate since at least FFY 2007.
- This slowing of spending growth, down from a peak of 31.4 percent in FFY 2015, is due in large part to fewer states expanding Medicaid under the Affordable Care Act (ACA).
- In dollar terms, the increase from FFY 2016 to FFY 2017 was $25.8 billion compared to $32.7 billion from FFY 2015 to FFY 2016.
- Medicaid managed care spending has increased at a 16.9 percent compounded annual growth rate (CAGR) since FFY 2007, compared to 6.1 percent growth in total Medicaid spending.
- Medicaid managed care spending represented 51.9 percent of total Medicaid spending in FFY 2017, exceeding half of total Medicaid medical services expenditures for the first time. Compared to FFY 2016, the penetration rate increased by 2.8 percentage points, the smallest annual increase since FFY 2011.
Medicaid MCO Expenditures as a Percentage of Total Medicaid Expenditures FFY 2007-2017 ($M)

Source: CMS-64
The data breaks down the state and federal share of Medicaid expenditures, which illustrates the impact that the Medicaid expansion, which was initially 100 percent federally funded in the states where it was implemented, has had on the sources of funding.
As the table below indicates, 61.6 percent of FFY 2017 spending was contributed by federal sources, which is 4.2 percentage points higher than the pre-Medicaid expansion share in FFY 2013, but 1.6 percentage points lower than FFY 2016 due to the matching rate reduction for Medicaid expansion enrollees from 100 percent to 95 percent.
Federal vs. States Share of Medicaid Expenditures, FFY 2012-2017
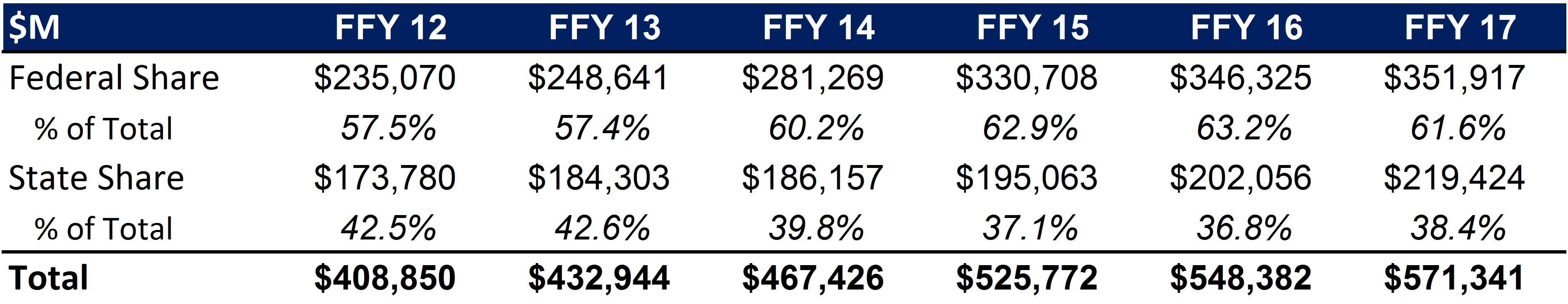
Source: CMS-64
State-specific Growth Trends
Forty-five states and territories report MCO spending on the CMS-64 report of which five states (Alabama, Idaho, North Carolina, Oklahoma and North Dakota) utilize a PCCM and/or PIHP/PAHP model exclusively. Of the remaining 40 states and territories that contract with risk-based MCOs, average spending in FFY 2017 increased 10.3 percent. On a percentage basis, Iowa experienced the highest year-over-year growth in Medicaid managed care spending for the second consecutive year at 88 percent, which was attributable to the continuing roll-out of its managed care program that began in April 2016. Louisiana, Nebraska and New York all saw Medicaid managed care spending growth of more than 40 percent.
The chart below provides additional detail on Medicaid managed care spending growth in states with risk-based managed care programs in FFY 2017. Interestingly, six states reported year over year declines in spending compared to two in FFY 2016.
Medicaid Managed Care Spending Growth on a Percentage Basis by State FFY 2016-17
Click to view graph in April 11, 2018 Weekly Roundup
Source: CMS-64
*Note: Not all states are included in the table due to incomplete data sets
Looking at year-over-year spending growth in dollar terms, New York experienced the largest increase in Medicaid managed care spending by far at over $13 billion. Other states with significant year-over-year spending increases in dollar terms included Lousiana ($2.6 billion), California ($2.2 billion) and Texas ($2.0 billion). All other states saw year-over-year spending growth of less than $2 billion. The chart below illustrates the year over year change in spending across the twenty states with the greatest increases.
Medicaid Managed Care Spending Growth on a Dollar Basis by State (Top Twenty States) FFY 2016-17 ($M)
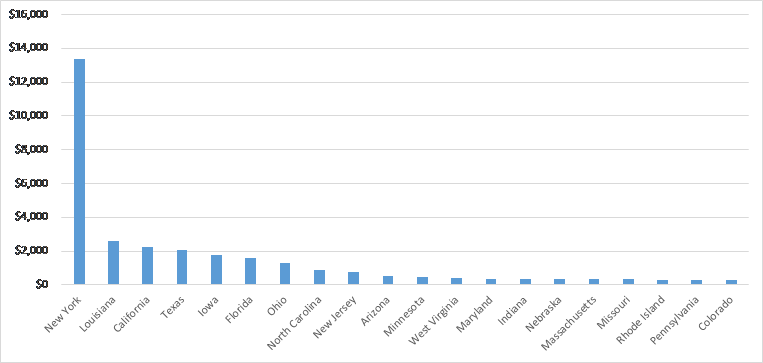
Source: CMS-64
The percentage of Medicaid expenditures directed through risk-based Medicaid MCOs increased by more than 5 percentage points in eight states from FFY 2016 to FFY 2017. The managed care spending penetration rate rose 16.3 percentage points in Nebraska, and 12.5 percentage points in Louisiana.
Medicaid MCO Expenditures as a Percentage of Total Medicaid Expenditures in States with a 5 percent or Greater Increase From FFY 2016 to FFY 2017 ($M)
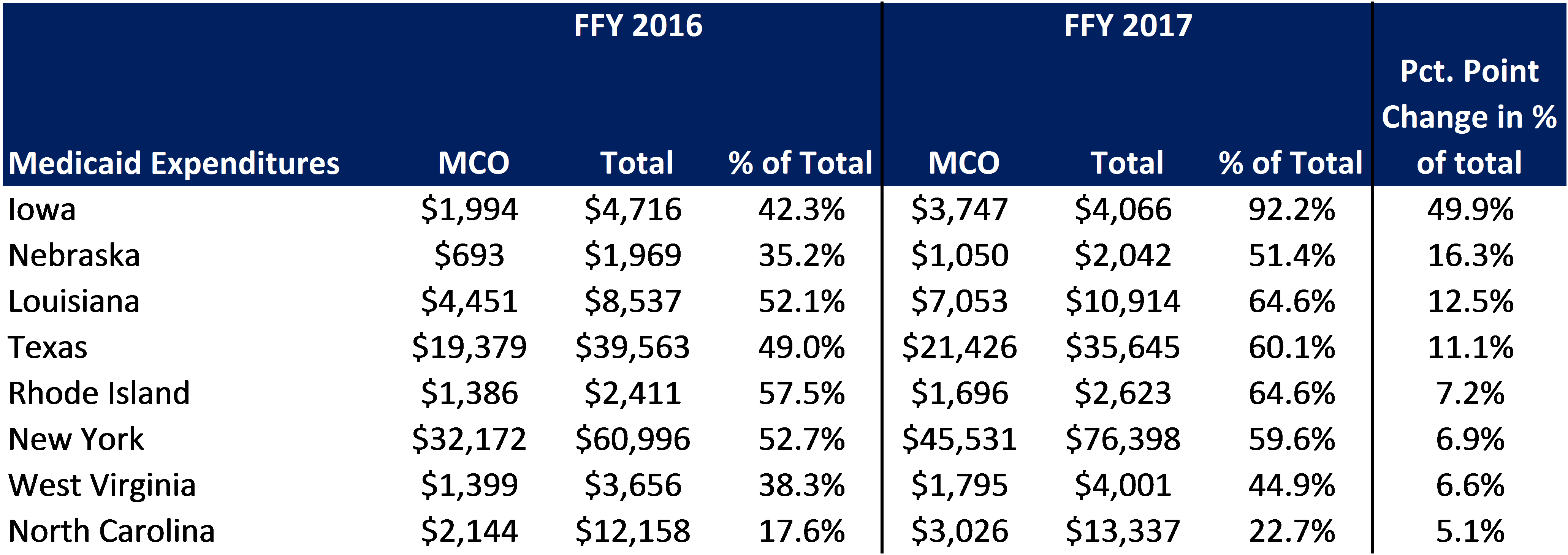
Source: CMS-64
The table below ranks the 40 states with risk-based comprehensive Medicaid managed care programs by the percentage of total Medicaid spending that is through Medicaid MCOs. Puerto Rico reported the highest such percentage at 98.6 percent, followed by Hawaii at 94.7 percent and Kansas at 93.5 percent. Iowa is fourth on the list having increased its Medicaid managed care spending penetration rate from 13.4% to 92.2% over the last two years.
We note that in many states, there are certain payment mechanisms which may never be directed through managed care such as supplemental funding sources for institutional providers and spending on retroactively eligible beneficiaries. Thus, the maximum achievable penetration rate in each state will vary and may be below that achieved in other states. Nevertheless, we note that there are a few large states where the penetration rates are currently below two-thirds of total spending but where they have expanded their Medicaid managed care programs recently including Pennsylvania and Virginia. Accordingly, we expect that in FFY 2017 we will see continued growth in Medicaid MCO penetration, though likely at a more moderate pace.
Medicaid MCO Expenditures as a Percent of Total Medicaid Expenditures, FFY 2015-2017
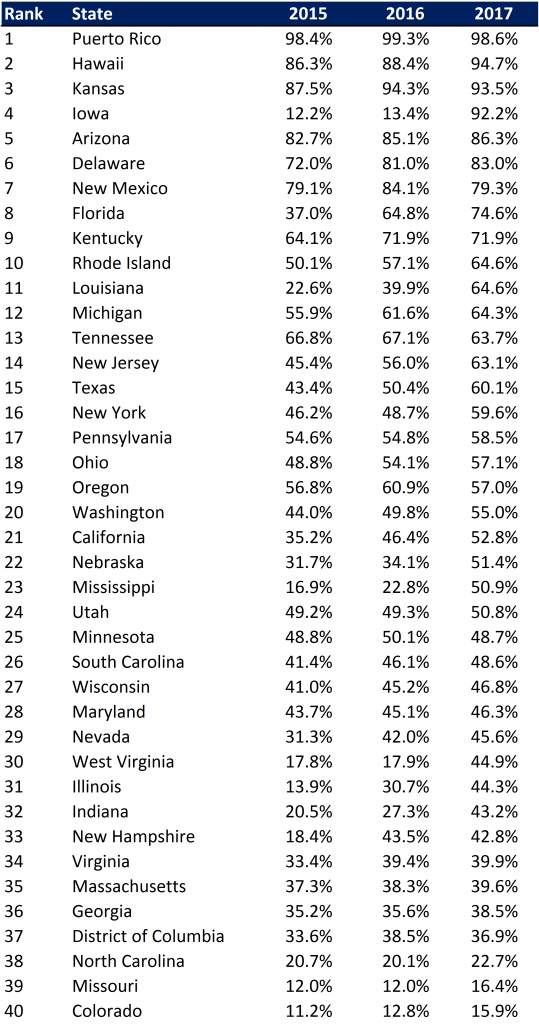
Source: CMS-64
Non-MCO Expenditures
Despite the rapid growth in Medicaid managed care over the last ten years, program spending still represented just over half of total Medicaid expenditures in FFY 2017. So where is the remaining FFS spending (approximately $275 billion) going? First, as noted above, there are many states/territories with Medicaid managed care programs where certain beneficiaries or services are carved-out of the program, and these are typically associated with high-cost populations. The total amount of non-MCO spending in these 40 states in FFY 2017 was around $235 billion. If we were to assume for the sake of argument that “full penetration” was 85 percent of total Medicaid spending, then we estimate that an additional $200 billion in current FFS spending could shift to a managed care model just in the states that already employ managed care for a subset of services and/or beneficiaries.
Next, there are 16 states/territories that did not utilize a comprehensive risk-based managed care model in FFY 2017. One of these states, North Carolina, is planning to implement such a model in the next several years. In general, the 16 states/territories that do not utilize managed care today are smaller states, North Carolina being the largest at $13 billion of Medicaid spending in FFY 2017. Total Medicaid spending across all 16 non-managed care states was $34.7 billion. The 16 states/territories that did not employ a risk-based comprehensive Medicaid managed care model in FFY 2017 were Alabama, Alaska, American Samoa, Arkansas, Connecticut, Guam, Idaho, Maine, Montana, Northern Mariana Islands, North Dakota, North Carolina, Oklahoma, South Dakota, Vermont and Virgin Islands.
In terms of spending by service line, the largest remaining fee-for-service (FFS) category is inpatient services, at $61 billion or 22.4 percent of FFS spending. This amount is split fairly evenly between regular FFS payments (53 percent of total) and supplemental/Disproporate Share Hospital (DSH) payments (47 percent). Measured as a whole, however, we estimate long term care services and supports (including nursing facility, waiver and other home and community based services) represent the largest FFS funding category.
Fee for Service Medicaid Expenditures by Service Line, FFY 2017
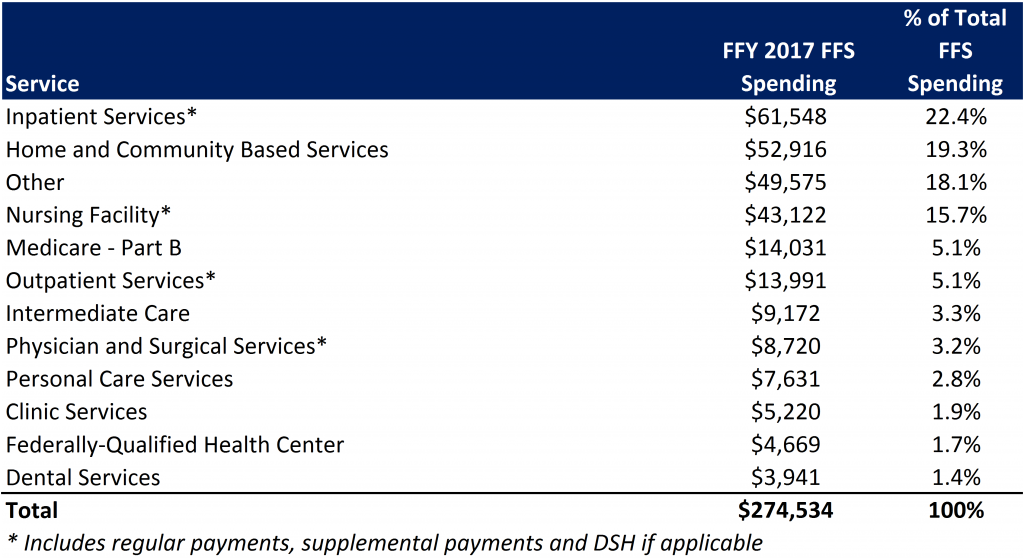
Source: CMS-64
Finally, we note that while the CMS-64 report provides valuable detail by service line for all FFS expenditures, it does not capture how spending directed to Medicaid MCOs is allocated by category of service. As such, it is not possible to calculate total spending by service line, a challenge that will only intensify as more spending runs through MCOs.