This week, our In Focus section reviews the Nebraska Heritage Health request for proposals (RFP), released by the Nebraska Department of Health and Human Services (DHHS) on April 15, 2022. DHHS will award statewide contracts to two or three Medicaid managed care organizations (MCOs) to serve approximately 342,000 individuals. Implementation is set to begin July 1, 2023. Contracts are currently worth $1.8 billion annually.
RFP
MCOs will provide integrated physical health, behavioral health, pharmacy, and dental services. Dental services are currently not covered under the MCO contracts and are instead provided under a separate dental benefit management contract. With the integration of dental services in the upcoming contracts, Nebraska Medicaid will be increasing dental rates to providers and removing the annual dental benefit limits for adults.
MCOs will be required to have a Fully Integrated Dual Eligible (FIDE) Dual Special Needs Plan (DSNP) in place no later than January 1, 2024.
Winning bidders will also be required to establish a common provider credentialing service. MCOs will work with all other contracted MCOs to jointly procure a Central Credentialing Verification Subcontractor (CCVS). The CCVS must begin its work at full capacity no later than one year from the start of the MCO’s contract start date. The CCVS will help reduce administrative burdens on providers and streamline the process to improve member access. A provider seeking to be credentialed with any of the MCOs will need to only submit a single application to the CCVS.
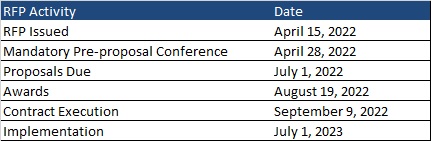
Timeline
A mandatory pre-proposal conference will be held on April 28, 2022. Proposals are due by July 1, 2022, with awards expected August 19. Contracts will be executed September 9, 2022, and implementation will begin July 1, 2023. Contracts will run for five years with two one-year renewal options.
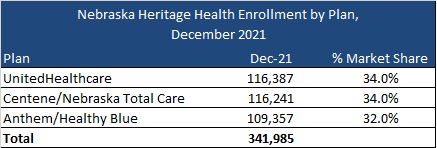
Current Market
Current incumbents are Anthem/Healthy Blue, Centene/Nebraska Total Care, and UnitedHealthcare, serving 342,000 Medicaid members as of December 2021.
Evaluation
Proposals that meet the mandatory requirements will be scored out of a total possible 6,600 points. Part 1, consisting of the corporate overview, will be worth 1,000 possible points. The corporate overview should include:
- the ability, capacity, and skill of the bidder to deliver and implement the system or project that meets the requirements of the solicitation
- the character, integrity, reputation, judgment, experience, and efficiency of the bidder
- whether the bidder can perform the contract within the specified time frame
- the quality of vendor performance on prior contracts
Part 2, consisting of the approach, will be worth 5,100 points. Bidders will provide a detailed response on how managed care services will be provided. Topics include:
- eligibility and enrollment
- business requirements
- staffing requirements
- covered services and benefits
- member services and education
- grievances and appeals
- provider network requirements
- provider services
- subcontracting requirements
- care management and case management
- quality management
- utilization management
- program integrity
- provider reimbursement
- systems and technical requirements
- claims management
- reporting and deliverables
- transition and implementation
- electronic visit verification for home health care services
Oral interviews, if required, will be worth 500 points.