This week, our In Focus reviews North Carolina’s much-anticipated Prepaid Health Plan Services request for proposals (RFP), released by the Department of Health and Human Services, Division of Health Benefits on August 9, 2018, and District of Columbia’s Medicaid Managed Care RFP released on August 14, 2018. North Carolina is transitioning its Medicaid fee-for-service program to Medicaid managed care through its procurement. DC is reprocuring its managed care program, covering the District of Columbia Healthy Families Program (DCHFP), Alliance program, and the Immigrant Children’s Program (ICP).
North Carolina
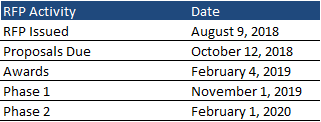
North Carolina has been working on a plan to transition 1.5 million individuals to Medicaid managed care since 2015. Following feedback from beneficiaries, clinicians, hospitals, counties, health plans, and elected officials, the state released an RFP for Prepaid Health Plans (PHPs) to provide coverage beginning in 2019, worth an estimated $6.4 billion in annual spending. PHPs, which include Commercial Plans (CPs) and Provider-Led Entities (PLEs), will integrate physical health, behavioral health, and pharmacy services for Medicaid and North Carolina Health Choice (health insurance for low-income children) beneficiaries. Proposals are due October 12, 2018, and contracts will be awarded on February 4, 2019.
Eligible Populations
Most North Carolina Medicaid and North Carolina Health Choice populations will be mandatorily enrolled in PHPs.
Exempt Populations:
- Medicare-Medicaid dual eligibles for whom North Carolina’s coverage is limited to Medicare premiums and cost sharing
- Medically needy
- Program of All-Inclusive Care for the Elderly (PACE) beneficiaries
- NC Health Insurance Premium Payment (HIPP) program beneficiaries
- Medicaid Family Planning program beneficiaries
- Prison inmates
- Community Alternatives Program for Children (CAP/C) beneficiaries
- Community Alternatives Program for Disabled Adults (CAP/DA) beneficiaries
- Qualified aliens subject to the five-year bar
Temporarily Excluded Populations:
- Nursing facility residents
- Medicare-Medicaid dual eligibles whom North Carolina Medicaid coverage is not limited to the coverage of Medicare premiums and cost sharing, excluding individuals served through CAP/DA
Individuals with a serious mental illness, a serious emotional disturbance, a severe substance use disorder, an intellectual/developmental disability, or a traumatic brain injury will be exempt until the state establishes Behavioral Health Intellectual/Developmental Disability Tailored Plans (BH I/DD Tailored Plans). These plans are expected to be operational at the start of the first State fiscal year one year after the implementation of the first contracts for Standard Benefit Plans.
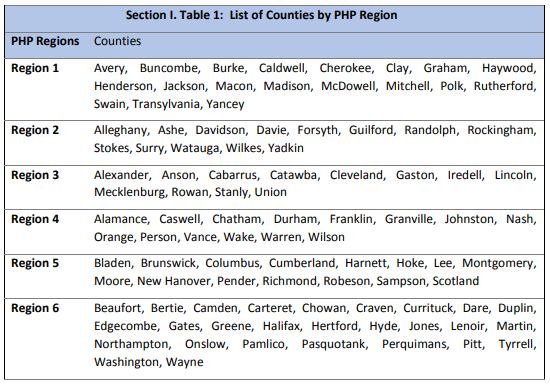
Services Areas
The RFP was released as a statewide procurement. The state has established six Medicaid Managed Care Regions, called PHP Regions. The Department will cap the number of regional contracts awarded at one (1) for each of Regions 1 and 6, and two (2) for each of Regions 2, 3, 4 and 5. Each PHP must serve a minimum of 45,000 to 50,000 lives across all regions it is awarded. To meet this requirement, the state strongly encourages PHPs to submit a bid for more than one region.
Timeline
Medicaid and North Carolina Health Choice beneficiaries who are not members of designated special populations will be transitioned from fee-for-service to managed care on a regional basis. The state is planning a two-phase approach with two distinct open enrollment periods to help ensure each region has an appropriate balance of enrollees, PHPs, and other considerations. Phase 1 is scheduled to begin on November 1, 2019, and Phase 2 is scheduled to begin on February 1, 2020. Following the awards, the state will announce which Regions will be selected for Phase 1 and Phase 2, depending on factors such as the number of members in the region, a goal of including urban and rural regions in Phase 1, and including a mix of commercial plans and PLEs, in Phase 1. North Carolina expects Tailored Plans to be operational at the start of the first fiscal year, one year after the implementation of the first contracts.
Evaluation
| Proposal Evaluation Criteria | Sub Weight | Weight |
| Qualifications/Experience | 20% | |
| Scope of Services | 70% | |
| a) Develop, implement and sustain the organizational, operational, technical and administrative functions and capabilities to reliably serve as an effective partner in delivering Medicaid Managed Care to North Carolinians. | 7.5% | |
| b) Improve the likelihood of better health outcomes by enhancing the Member experience through promoting Member rights, engaging Members through health education, providing optimal customer service and support, and delivering services in a culturally competent manner. | 15% | |
| c) Develop coordinated programs and services that deliver health through whole-person care, comprehensive care management, improve population health, and provide programs and services addressing healthy opportunities. | 25% | |
| d) Develop and maintain a robust provider network that maintains strong provider and community participation and demonstrates an understanding of the health needs of the North Carolina population to ensure available, accessible, high quality care and services are delivered to all Members. | 15% | |
| e) Develop a comprehensive quality improvement and value-based purchasing approach to drive the Department’s overall vision for advancing and measuring high-value care. | 15% | |
| f) Engage and integrate key Department partners and stakeholders including tribal populations, county agencies, community-based organizations, other managed care program entities, and Department partners to support North Carolina’s Medicaid Managed Care goals. | 7.5% | |
| g) Promote and monitor North Carolina’s Medicaid Managed Care sustainability by developing the processes, standards, and data protocols needed to demonstrate good financial stewardship of limited resources and adherence to financial management objectives. | 10% | |
| h) Promote a culture of compliance through comprehensive oversight and program integrity strategies aligned with industry best practices and compliant with federal and state law and regulation. | 5% | |
| Use Cases | 5% | |
| Client References | 5% | |
| Bonus Points: Marketplace Participation | 2.5% |
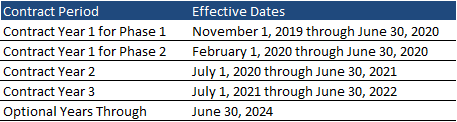
Contracts
The contracts will be effective for three years, with two additional optional years. Phase 1 contracts will begin November 1, 2019 and Phase 2 contracts will begin February 1, 2020. Contract Year 1 for both phases will run through June 30, 2020, followed by an additional two years ending June 30, 2022. The program will be worth $6.4 billion in annualized spending.
District of Columbia
The District of Columbia is reprocuring its Medicaid Managed Care Program (MMCP), worth approximately $1 billion. Managed care organizations (MCOs) will serve the Medicaid program, District of Columbia Healthy Families Program (DCHFP); Alliance program, covering low-income residents not eligible for Medicaid; and the Immigrant Children’s Program (ICP), covering low-income immigrant children not eligible for Medicaid.
The RFP comes after an administrative law judge ruled in December 2017 that the District failed to treat all bidder’s equally and “undermined the integrity of the procurement process,” ordering DC to reevaluate the bids of the previous procurement. The District announced contract awards to AmeriHealth Caritas, Trusted Health Plan, and Anthem/Amerigroup in May 2017. Incumbent MedStar was not awarded a contract and filed a protest.
Contracts
DC expects to award up to three new contracts. Proposals are due September 13, 2018. Contracts will run from the date of award to September 30, 2019. DC may extend the contracts for four one-year option periods. The total duration of the contracts cannot exceed five years.
Evaluation
Proposals will be scored out of a total of 112 points, consisting of technical criteria, price, and preference points. The price evaluation is objective, with the lowest price receiving the maximum score.
| Evaluation Criteria | Points |
| Technical Criteria | 90 |
| Technical Approach and Methodology | 45 |
| Offeror’s comprehensive explanation about the processes, resources, and activities it will employ to successfully implement the Medicaid managed care contract (operations and scope of work) in the District of Columbia, including the organizational description listing Offeror’s proposed key personnel. | 20 |
| Offeror’s detailed explanation and description of its processes for improving access and utilization of perinatal visits and birth outcomes within the eligible populations, as defined in Section B.1, including how the Offeror proposes to enhance Enrollee engagement to increase prenatal visits and Provider engagement to achieve timely access to perinatal services and improved birth outcomes. | 15 |
| Offeror’s detailed explanation of its approach and methodology to ensure all of its Network Providers are enrolled as Medicaid providers with the District as of the Start Date and prior to the Offeror rendering services to Enrollees. | 10 |
| Technical Expertise | 25 |
| The extent to which the Offeror’s Utilization Management (UM) program and processes: uses nationally recognized clinical practice guidelines/criteria and adverse action notification procedures; uses the UM committee; encompasses a prior authorization process; demonstrates integration between UM and Case Management departments; and includes UM program evaluation methodologies with the expected outcomes. | 10 |
| Offeror’s detailed description of its proposed complex case management program and methodology for identifying Enrollees who are appropriate for case management; efforts to engage Enrollees in case management, once Enrollees are enrolled in case management; and care coordination amongst various health care providers, the Enrollee’s family, social support agencies, and other relevant entities who will be involved in the Enrollee’s care. | 15 |
| Past Performance | 20 |
| Price Criterion | 10 |
| Preference Points | 12 |
| Total | 112 |