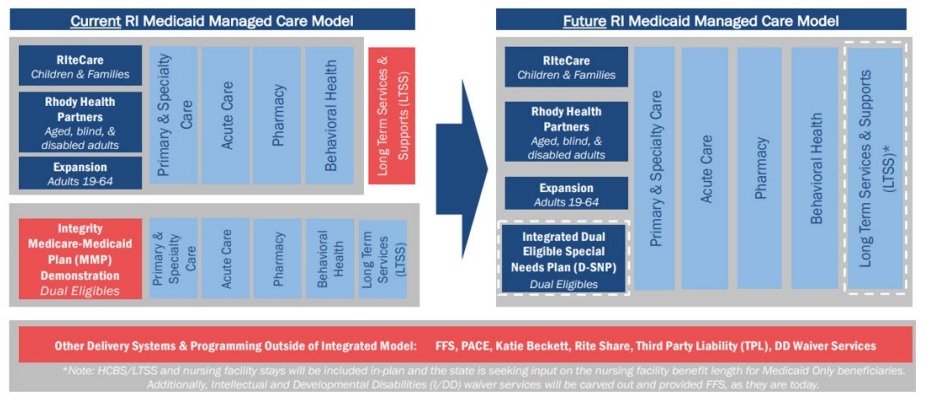
This week our In Focus section reviews the Rhode Island statewide, capitated risk-bearing Medicaid managed care program request for proposals (RFP), which the Rhode Island Executive Office of Health and Human Services (EOHHS) released December 15, 2023. New program changes will include carving in long-term services and supports (LTSS) as an in-plan benefit for all populations and expanding managed care to include people who are dually eligible for Medicare and Medicaid. Contracts are expected to be worth $2.3 billion.
Background
Rhode Island’s Medicaid managed care program, which operates under the authority of a Section 1115 waiver and Section 1932(a) state plan amendment, consists of the following programs:
- RIteCare, which serves children and families, including children with special healthcare needs
- Rhody Health Partners, which serves aged, blind, or disabled (ABD) adults
- Medicaid expansion, which serves childless adults ages 19 to 64
At present, full-benefit dual eligible (FBDE) members are not covered through the Medicaid managed care organization (MCO) contracts.
RFP
New contracts will be implemented in three phases, starting with enrollment of core populations and the addition of LTSS in-plan benefits to Medicaid managed care for Medicaid-only enrollees beginning July 1, 2025. In the second phase, current fully dual eligible members will transition to Medicaid managed care plans on January 1, 2026. All bidders will be required to offer an integrated Dual Eligible Special Needs Plan (D-SNP) and managed LTSS (MLTSS) plan to dually eligible members, as Rhode Island transitions from the Financial Alignment Initiative (FAI) Medicare-Medicaid Plan (MMP) Demonstration, which sunsets December 31, 2025. In addition, beginning January 1, 2027, default enrollment will begin for Medicaid members who become newly eligible for Medicare.
EOHHS will award contracts to two or three MCOs.
Other changes in the RFP include increasing oversight and accountability for the use of pharmacy benefit managers (PBMs); requiring that EOHHS approve contracts for MCO major subcontractors; reducing unnecessary prior authorizations, particularly for behavioral health services; increasing financial sanctions for noncompliant MCOs; and increasing investments in population health and health equity with a focus on the identification of health disparities; and other changes.
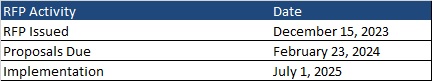
Timeline
Proposals are due February 23, 2024. The new contracts will take effect July 1, 2025, and will run through June 30, 2030, with an option to extend the agreement for up to five additional years.
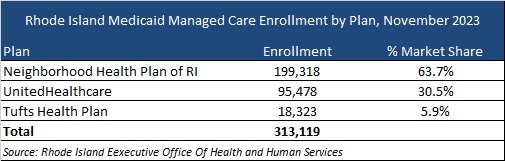
Current Market
Neighborhood Health Plan, Tufts Health, and UnitedHealthcare served approximately 313,000 members as of November 2023. These MCOs have signed contract extensions through June 30, 2025.
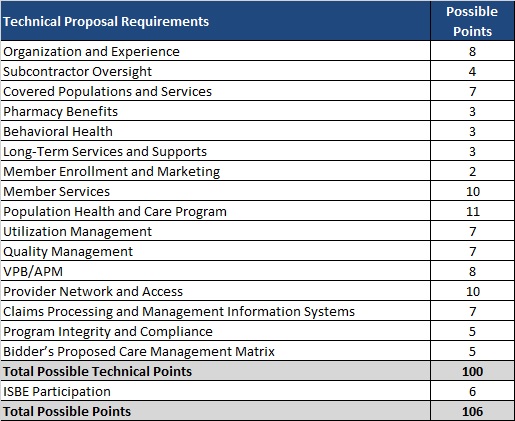
Evaluation
Rhode Island will not require cost proposals under this procurement, with capitation rates set by EOHHS actuaries. MCOs must meet the passing technical score of 85 points. Technical proposal requirements are shown below: