HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Massachusetts Releases RFR for One Care and Senior Care Options

- Wakely, an HMA Company Releases New White Paper Summarizing HHS’ Proposed 2025 Notice of Benefit and Payment Parameters

- Arizona Medicaid Awards Long Term Care Contracts to Centene, United

- Florida Governor’s FY 2005 Budget Proposes More Funding for Florida KidCare, HCBS Waivers

- Florida Legislative Research Office Projects Shortage of 18,000 Physicians by 2035

- Georgia Lawmakers Exploring ‘Private Option’ Model for Medicaid Expansion

- Idaho Medicaid Task Force Fails to Agree on Medicaid Managed Care Restructuring

- Indiana Medicaid Officials Brief Lawmakers on MLTSS Roll-out, Maternal Mortality Initiatives

- Louisiana Medicaid Plan Partners with State Medical Society to Extend Value-based Payment to Independent Practitioners

- New Mexico Medicaid Increases Provider Reimbursements by $409 Million

- North Dakota Seeks Public Comments on Medicaid Quality Strategy Plan

- Pennsylvania Announces Public Comment Period for Section 1115 Waiver Application Addressing Health-related Social Needs

- Medicaid Eligibility Redetermination News: Illinois, Louisiana, Michigan, New York, Ohio, Utah

- Integrated Eligibility System Updates: Florida, West Virginia

- CMS Issues Medicaid Redetermination Reporting Rule With Penalties to Stop Erroneous Disenrollments

- InnovAge Finalizes Acquisition of Two ConcertoCare PACE Programs

In Focus
Massachusetts Releases RFR for One Care and Senior Care Options
This week, our In Focus section reviews the request for responses (RFR) for the Massachusetts One Care and Senior Care Options (SCO) programs, released by the Massachusetts Executive Office of Health and Human Services (EOHHS) on November 30, 2023. The programs provide physical, behavioral, long-term services and supports (LTSS), and other community services to Medicare and Medicaid dual-eligible beneficiaries. Implementation is set to begin January 1, 2026.
One Care
One Care launched in 2013 as a Section 1115 Medicare-Medicaid Plan (MMP) program dual demonstration waiver. It operates under a financial alignment initiative (FAI) capitated model. The program provides integrated care to dual eligible adults ages 21 to 64. Individuals may remain enrolled in One Care when they turn 65 years old as long as they continue to meet all other requirements. Members can also access an independent LTSS coordinator.
As the Centers for Medicare & Medicaid Services (CMS) sunsets the FAI dual demonstrations, One Care will shift to a Fully Integrated Dual Eligible Special Needs Plan (FIDE SNP) beginning in 2026, pending federal approval of the Section 1115 amendment request. Members will have exclusively aligned enrollment with the same plan for both Medicare and Medicaid coverage.
SCO
SCO launched in 2004 and is currently a FIDE SNP with exclusively aligned enrollment. Medicaid enrollees ages 65 and older with or without Medicare are eligible. Enrollment in this managed care program is voluntary. Individuals on the Frail Elder Waiver can only join SCO.
RFR
Massachusetts will award separate contracts for One Care and SCO but may prefer bids from plans seeking to operate both; however, plans may submit bids to operate one type of plan. The state seeks to offer both One Care and SCO coverage for eligible individuals in as many counties as possible, and ideally statewide. Plans must propose to cover people in at least six counties for each type of plan.
To be selected, plans will need to have a contract with CMS to operate a FIDE SNP in Massachusetts in 2026. Applications must be submitted to CMS by February 2025.
Timeline
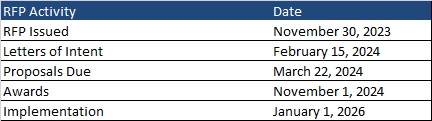
Letters of intent are due February 15, 2024, and the deadline for responses is March 22, 2024. Plans will be selected by November 1, 2024. Implementation is set to begin January 1, 2026. Contracts will run an initial five-year term through December 31, 2030. Contracts may be renewed for up to five years in any increment.
Current Market
Commonwealth Care Alliance, Tufts, and UnitedHealthcare serve 43,000 One Care members.
SCO incumbents WellSense Senior Care Options (formerly BMC Healthnet), Commonwealth Care Alliance, Fallon Health, Molina/Senior Whole Health, Tufts, and UnitedHealthcare serve 77,000 members.
Wakely, an HMA Company Releases New White Paper Summarizing HHS’ Proposed 2025 Notice of Benefit and Payment Parameters
On November 15, 2023, the Department of Health and Human Services (HHS) released the proposed Notice of Benefit and Payment Parameters (Payment Notice) for 2025. The notice includes important proposed rules and parameters for the operation of the individual and small group health insurance markets in 2025 and beyond. More detail on key provisions of the proposed notice, actuarial value calculator, and maximum out of pocket information is included in a white paper available from Michael Cohen and actuary Luke Bremmer of Wakely Consulting Group, an HMA company.
HMA staff and our family of companies have extensive experience in assessing the implications of these policy decisions for state agencies, health plans, and other stakeholders. If your organization is interested in more information, contact Patrick Tigue, Zach Sherman, and Michael Cohen to learn how our expert team can assist with analysis and actuarial support. Read More
HMA Roundup
Arizona
Arizona Medicaid Awards Long Term Care Contracts to Centene, United. The Arizona Health Care Cost Containment System announced on December 1, 2023, that it has awarded contracts to Centene and UnitedHealthcare for the Arizona Long Term Care System Elderly and Physically Disabled program, which covers over 26,000 individuals. Contracts run from October 1, 2024, through September 30, 2027, with options not exceeding a total contract period of seven years. The incumbents are Banner-University Family Care, Mercy Care Plan, and UnitedHealthcare. Other bidders included Banner, Mercy Care, and Blue Cross Blue Shield of Arizona. Read More
California
California Medicaid’s CalAIM Initiative Faces Implementation Challenges, Survey Finds. KFF reported on December 5, 2023, that a quarter of the health care insurers, nonprofit organizations, and others responsible for identifying and enrolling patients into California Advancing and Innovating Medi-Cal (CalAIM) are not familiar with the program, according to a California Health Care Foundation survey conducted between July 21, 2023, and September 12, 2023. Implementers surveyed cited workforce shortages, lack of state payments to cover social services costs, inadequate technology assistance, and inconsistencies in rules implemented by managed care plans as barriers to the program. So far, about 141,000 Medi-Cal patients have a personal care manager through CalAIM, and respondents report they are reaching more people and improving access to care. Read More
Florida
Florida Governor’s Fiscal 2025 Budget Proposes More Funding for Florida KidCare, HCBS Waivers. Florida Phoenix reported on December 5, 2023, that Florida Governor Ron DeSantis’s fiscal 2025 state budget proposal included $310 million for the Florida KidCare Program, which subsidizes healthcare for children under age 19 that do not qualify for Medicaid, and a $116.8 million compensation increase for Medicaid providers serving children, pregnant women, and postpartum people. The proposal also requests $127.4 million for Florida’s home and community-based Medicaid waiver program for people with intellectual and developmental disabilities and a pilot program that would deliver care not otherwise covered. Read More
Florida Legislative Research Office Projects Shortage of 18,000 Physicians by 2035. Health News Florida reported on December 6, 2023, that the Florida Legislature’s Office of Program Policy Analysis and Government Accountability (OPPAGA) informed lawmakers that the state is facing a physician shortage of approximately 18,000 by 2035, resulting in the workforce meeting 77 percent of projected demand that year. OPPAGA found that Florida’s Graduate Medical Education program retains 79 percent of its graduates following residency, which is lower than some other states. Senate President Kathleen Passidomo (R-Naples) plans to focus on addressing the physician shortage issue in the 2024 legislative session. OPPAGA recommended strategies to encourage Florida medical schools to prioritize in-state students when matching graduates to healthcare facilities and conduct further research to improve retention rates. Read More
Florida Launches New Integrated Eligibility Portal. Health News Florida reported on December 5, 2023, that Florida has launched a new Medicaid eligibility portal for Medicaid, Supplemental Nutritional Assistance Program (SNAP), and Temporary Assistance for Needy Families recipients. The portal will utilize new technology and retain its original name, MyAccess. The portal will serve more than five million Medicaid beneficiaries and three million SNAP recipients. Read More
Georgia
Georgia Lawmakers Exploring ‘Private Option’ Model for Medicaid Expansion. Governing reported on November 29, 2023, that Georgia legislators are considering a potential Medicaid expansion program structured like Arkansas’s “private option” expansion program, which uses expansion funding to buy private insurance for uninsured residents. This week a key Senate committee approved recommendations to repeal certificate of need laws, which legislators are seeking to couple with the state’s Medicaid expansion plan. Lawmakers expect to revisit these issues in the 2024 legislative session. Read More
Idaho
Idaho Medicaid Task Force Fails to Agree on Medicaid Managed Care Restructuring. The Idaho Capital Sun reported on November 28, 2023, that the Idaho Legislature’s Medicaid Managed Care Task Force issued its final report with a recommendation to keep the existing Medicaid managed care structure rather than move to a comprehensive managed care program. The report recommends that policymakers continue studying ways to improve the existing value-care model and create new quality metrics for the value care and managed care organizations. The group also proposed to convene a new panel to enhance monitoring of the state’s Medicaid contracts. Read More
Illinois
Illinois Shifts to Individual Ex Parte Medicaid Eligibility Redeterminations to Prevent Incorrect Procedural Disenrollments. State of Reform reported on December 1, 2023, that the Illinois Department of Health and Family Services has resumed Medicaid eligibility redeterminations and is conducting ex parte redeterminations on the individual level to prevent unnecessary procedural disenrollments, as required by the Centers for Medicare & Medicaid Services. The state is currently working to reinstate Medicaid beneficiaries who were inappropriately disenrolled on July 31. Thus far, Illinois has completed two-thirds of its Medicaid redeterminations and has disenrolled approximately 57,700 individuals. Well over three-quarters of disenrolled individuals were found to be ineligible for renewal. Read More
Indiana
Indiana Medicaid Officials Brief Lawmakers on MLTSS Roll-out, Maternal Mortality Initiatives. The Indiana Capital Chronicle reported on November 30, 2023, that Indiana Medicaid is slated to begin coverage under its new PathWays for Aging Program by July 1, 2024. Approximately 130,000 individuals over age 60 will be eligible to receive managed long-term services and supports (MLTSS) through the PathWays program, and they can begin selecting a plan starting in February 2024. State officials also report that $4.5 million has been distributed to organizations working to address Indiana’s maternal mortality level, including through the state’s pilot Pregnancy Promise program designed to treat pregnant mothers with substance use disorder and opioid use disorder. Read More
Louisiana
Louisiana Disenrolls 197,000 Medicaid Beneficiaries During Redeterminations. The Louisiana Illuminator reported on December 4, 2023, that Louisiana has disenrolled a total of 197,000 Medicaid beneficiaries, with a quarter of those disenrolled being children, following eligibility redeterminations from June through October 2023. Of those disenrolled, about two-thirds were due to procedural reasons. Initially, the state disenrolled 258,000 individuals, including 45,266 during October, but has since restored eligibility for approximately 61,000 of these individuals. Read More
Medicaid Plan Partners with State Medical Society to Extend Value-based Payment to Independent Practitioners. Biz New Orleans reported on December 3, 2023, that Louisiana Healthcare Connections, a subsidiary of Centene Corporation, will partner with the Louisiana State Medical Society to extend value-based payments and quality incentives to independent practitioners to improve healthcare delivery and access for Medicaid beneficiaries. Louisiana Healthcare Connections will also invest $1 million to allow participating practitioners to implement electronic medical records and support enhanced interoperability for independent primary care practices. Read More
Michigan
Michigan Medicaid Disenrolls 16,424 Beneficiaries in October. The Michigan Department of Health and Human Services announced on November 29, 2023, that it has disenrolled 16,424 Medicaid beneficiaries during October redeterminations, including 2,806 for procedural reasons. The state renewed coverage for 168,088 beneficiaries and has more than 85,000 pending eligibility cases for individuals whose renewal was due in October. Read More
New Mexico
New Mexico Maternal Mortality Committee Issues Recommendations to Reduce Maternal Deaths. Source New Mexico reported on December 4, 2023, that 86 percent of pregnancy-related maternal deaths in New Mexico were preventable, with Medicaid beneficiaries accounting for the majority of deaths, according to the New Mexico Maternal Mortality Review Committee’s annual report using data from 2015 through 2020. The Pregnancy-related Mortality Ratio nationwide is 17 deaths per 100,000 live births through 2019, but in New Mexico that figure is 31 deaths per 100,000 live births through 2020. The state received a five-year federal grant that will support a new maternal health task force starting in 2025 to address and improve maternal health outcomes. Read More
Medicaid Increases Provider Reimbursements by $409 Million. The New Mexico Human Services Department announced on December 1, 2023, a $409 million increase in reimbursement rates for the majority of Medicaid health care providers, retroactive to July 1, 2023. The rate increase is part of a three-phase approach aimed at boosting payments to ensure Medicaid beneficiaries have access to essential health care services. The proposal for phase three rate increases has been included in the agency’s budget request for state fiscal year 2025. Read More
New York
New York Disenrolls 784,798 Medicaid Beneficiaries Following Redeterminations from July Through October. The Times Union reported on December 1, 2023, that New York has disenrolled 784,798 Medicaid beneficiaries, including 384,964 that were disenrolled due to procedural reasons, during redeterminations from July through October. The state has renewed coverage for approximately 1.7 million beneficiaries and has about 70,800 pending eligibility cases for individuals whose renewal was due between July through October. Read More
North Dakota
North Dakota Seeks Public Comments on Medicaid Quality Strategy Plan. The North Dakota Health and Human Services department announced on December 1, 2023, that it is seeking public comments on the draft 2024 North Dakota Medicaid Quality Strategy Plan, which aims to ensure compliance with federal quality requirements. The strategy sets a direction for priority interventions and identifies the standards for optimizing desired outcomes for Medicaid fee-for-service enrollees as well as the Medicaid expansion members enrolled in a managed care organization. Comments will be accepted through January 2, 2024. Read More
Ohio
Ohio Disenrolls 71,367 Medicaid Beneficiaries During October Redeterminations. News 5 Cleveland reported on December 2, 2023, that Ohio disenrolled 71,367 Medicaid beneficiaries in October, including 52,782 for procedural reasons and 18,585 due to ineligibility. The state has disenrolled a total of more than 342,000 enrollees since redeterminations began in April. Read More
Pennsylvania
Pennsylvania Announces Public Comment Period for Section 1115 Waiver Application Addressing Health-related Social Needs. Pennsylvania Department of Human Services (DHS) Secretary Dr. Val Arkoosh announced on December 4, 2023, that the public comment period for Pennsylvania’s new Section 1115 waiver application, titled “Bridges to Success: Keystones of Health For Pennsylvania,” will be open through January 2, 2024. The waiver is intended to address health-related social needs and continuous eligibility among vulnerable populations utilizing an integrated, whole-person approach. The waiver specifically aims to reduce healthcare costs and expand services to individuals in the focus areas: individuals reentering society from correctional facilities; recipients in need of stable housing, food and nutrition services; and continuous Medicaid coverage for children under age six. If approved, the state would administer the waiver from January 1, 2025, to January 1, 2030. Read More
Utah
Utah Disenrolls 132,306 Medicaid Beneficiaries During Redeterminations. State of Reform reported on December 6, 2023, that Utah has disenrolled 132,306 Medicaid beneficiaries during redeterminations from April through October. Of those disenrolled, 94 percent or 124,544 were due to procedural reasons. The state has renewed coverage for 95,618 beneficiaries and is expected to complete redeterminations for the remaining 7 percent of beneficiaries by April 2024. Read More
West Virginia
West Virginia Launches Pilot Transfer for Family Assistance Programs to Integrated Eligibility System. The West Virginia Department of Health and Human Resources announced on December 1, 2023, that it will launch a pilot transfer of its integrated eligibility system for family assistance programs from the Recipient Automated Payment and Information Data System to West Virginia People’s Access to Help this month for Clay, Hardy, Kanawha, Mercer, Mingo, and Randolph counties. The statewide transition will occur in Spring 2024 and is intended to improve eligibility determination and delivery of services for Medicaid, Supplemental Nutrition Assistance Program, Temporary Assistance for Needy Families, child welfare, child care, and child support. Read More
National
CMS Issues Medicaid Redetermination Reporting Rule With Penalties to Stop Erroneous Disenrollments. Modern Healthcare reported on December 4, 2023, that states not in compliance with federal rules governing Medicaid redeterminations are at risk of reduced federal funding under an interim final rule released by the Centers for Medicare & Medicaid Services (CMS). States failing to provide CMS with monthly redetermination reports will have to submit corrective action plans, and failure to do so will result in a pause of procedural disenrollments and penalties of up to $100,000 per day, effective December 6. Public comments will be accepted through February 2. CMS reiterated that it will work with states to fix the issues before deciding to take enforcement actions. Read More
HHS OIG to Recoup More Than $3.4 Billion in Healthcare Fraud, Misspent Funds in Fiscal 2023. Healthcare Dive reported on December 4, 2023, that more than $3.44 billion is expected to be recovered by the Department of Health and Human Services (HHS) Office of the Inspector General (OIG) in fiscal 2023 following an investigation into fraud and misspent funds in Medicare, Medicaid, and other government health programs. HHS OIG found 707 criminal enforcement actions and 746 civil actions including false claims, unjust-enrichment lawsuits, and civil monetary penalty settlements from October 1, 2022, through September 30, 2023. Read More
CMS Releases First Annual Guidance on Medicaid Core Set Reporting. The Centers for Medicare & Medicaid Services (CMS) released on December 1, 2023, a State Health Official (SHO) letter which details the requirements for compliance with mandatory annual state reporting of the Core Set of Children’s Health Care Quality Measures for Medicaid and CHIP (Child Core Set) and the behavioral health measures on the Core Set of Adult Health Care Quality Measures for Medicaid (Adult Core Set). The letter includes guidance on mandatory reporting regulations; core set measures; populations and the population exemption process; stratification categories; measures subject to stratification; attribution rules; and the Child and Adult Core Set State Plan Amendment. Read More
14 States Paid Managed Care Organizations $249M for Deceased Medicaid Enrollees, OIG Finds. Becker’s Payer Issues reported on November 30, 2023, that 14 audits conducted between 2009 and 2019 found that California, Ohio, Michigan, Florida, New York, Kansas, Illinois, Minnesota, North Carolina, Tennessee, Georgia, Texas, Indiana, and Wisconsin paid an estimated $249 million in improper capitation payments for deceased enrollees, according to a report from the U.S. Department of Health and Human Services Office of the Inspector General (OIG). Several of these states did not utilize federal data to identify individuals’ date of death, and 11 of the 14 states failed to identify and process enrollees’ death information. The OIG recommended that the Centers for Medicare & Medicaid Services (CMS) collect payments from the three states that still owe the government. CMS disagreed with a separate recommendation that the agency examine options to connect federal and state data to identify deaths. Read More
Medicaid, CHIP Enrollment Drops 1.5 Million in August 2023, CMS Reports. The Centers for Medicare & Medicaid Services (CMS) reported on November 30, 2023, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) was approximately 90 million in August 2023, a decrease of 1.5 million from July 2023. Medicare enrollment was 66.3 million, up 129,947 from July 2023, including 32.3 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. Read More
Industry News
InnovAge Finalizes Acquisition of Two ConcertoCare PACE Programs. InnovAge announced on December 1, 2023, that it has completed its acquisition of two California-based PACE programs operated by ConcertoCare. With the acquisition, InnovAge now operates 18 PACE centers in five states and has four PACE centers under development. Read More
H.I.G. Growth Completes Sale of Just Home Healthcare Services to Honor Health Network, RHA Health Services. H.I.G. Growth Partners announced on December 6, 2023, the sale of its portfolio company, Just Home Healthcare Services, in two parts. H.I.G. sold the Personal Home Care and Adult Day Health business segments to Honor Health Network in April 2023, and the Independent Living Program business segments to RHA Health Services in October 2023. Read More
Banner Health Transfers Arizona Hospice Operations to Hospice of the Valley. Modern Healthcare reported on December 5, 2023, that Phoenix-based health system Banner Health has ended hospice operations in Arizona effective December 1. Banner Health transitioned operations to the Phoenix-based nonprofit Hospice of the Valley, which served approximately 22,000 patients last year. Banner Health will continue to operate its hospice locations in Colorado. Read More
Tygon Peak Invests in Two TX Primary Care Businesses to Develop New Healthcare Platform. Tygon Peak Capital, a New York-based private equity firm, announced on December 5, 2023, that it has invested in two Texas-based primary care businesses, Doctors of Internal Medicine (DIM) and Internal Medicine Associates of Plano (IMAP), to create a new healthcare platform, known as the Platform. The chief executives of the two businesses will continue to act as co-chief executives of the Platform, which will provide primary care, geriatrics, endocrinology, radiology and cardiology testing, allergy, chronic care management, lab testing, and cosmetic services. Read More
HealthEdge Partners Invests in P3 Oral Surgery to Develop Oral Surgery Platform. HealthEdge Investment Partners announced on December 4, 2023, that it has invested in Pluri Potent Partnership (P3), an oral surgery organization, to build an Oral Surgery Services Organization in the Mid-Atlantic region. P3 currently supports thirteen locations in the region, and its surgeons will retain an ownership stake. Read More
Health Care Service Corporation Considers Buying Cigna’s Medicare Advantage Business. Health Payer Specialist reported on November 30, 2023, that Health Care Service Corporation is considering purchase of Cigna Group’s Medicare Advantage business, comprised of less than 600,000 enrollees. The report coincides with Cigna’s discussion of a potential merger with Humana and potential efforts to appease antitrust regulators. Read More
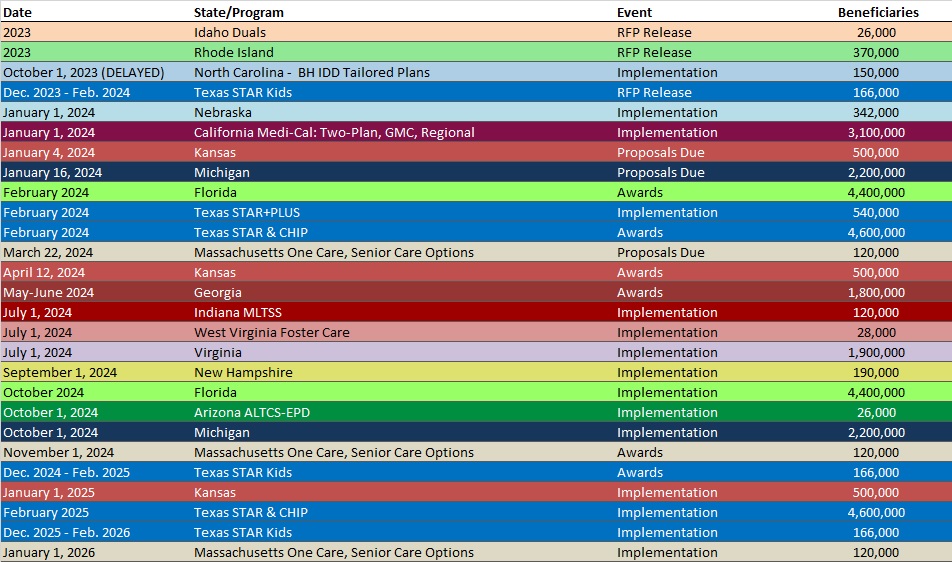
RFP Calendar
HMA News & Events
Upcoming HMA Webinar:
Collaborating to Improve Children’s Behavioral Health- A Comprehensive Playbook to Fostering Wellbeing in Children. Tuesday, December 12, 2023, 12 p.m. ET. Beyond the statistics lie the stories of countless children and families needing immediate and critical access to behavioral health services and community-based supports. Addressing these issues requires comprehensive cross-system reforms, including policies that promote integrated financing, enhanced care coordination, increased provider collaboration, and bolster upstream prevention efforts. HMA is working with several national partner organizations to prioritize and focus on cross system integrated and interoperable solutions to address the needs of children, youth, and families with complex behavioral health needs.
Health Management Associates (HMA) in partnership with the National Association of State Mental Health Program Directors (NASMHPD), National Association of Medicaid Directors (NAMD), and Child Welfare League of America (CWLA), American Public Human Services Association (APHSA), and with support from the Annie E. Casey Foundation, Casey Family Programs and other funders, developed a multi-state policy lab to be held in February 2024. Applications for state agency participation will be open the week of November 6th. This webinar will share more about the overall effort and for states to hear from this partnership on the importance of collaborating to strengthen the children’s behavioral health system. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Colorado RAE Enrollment is Down 0.7%, Jun-23 Data
- Colorado RAE Enrollment is Up 1.3%, May-23 Data
- Colorado RAE Enrollment is Up 0.9%, Apr-23 Data
- Colorado RAE Enrollment is Up 1.9%, Mar-23 Data
- MLRs at Iowa Medicaid MCOs Average 90.9%, 2022 Data
- Louisiana Medicaid Managed Care Enrollment is Down 8%, Oct-23 Data
- Maryland Medicaid Managed Care Enrollment Is Flat, Jul-23 Data
- MLRs Average 83.4% at Michigan Medicaid MCOs, 2022 Data
- Mississippi Medicaid Managed Care Enrollment is Down 1%, Oct-23 Data
- MLRs Average 90.3% at Nebraska Medicaid MCOs, 2022 Data
- MLRs Average 84% at New Jersey Medicaid MCOs, 2022 Data
- MLRs Average 81.2% at Ohio Medicaid MCOs, 2022 Data
- MLRs at Pennsylvania Medicaid MCOs Average 89%, 2022 Data
- MLRs Average 89.6% at Puerto Rico Medicaid MCOs, 2022 Data
- Rhode Island SNP Membership at 14,556, Mar-23 Data
- MLRs Average 89.8% at Rhode Island Medicaid MCOs, 2022 Data
- MLRs Average 81.5% at Tennessee Medicaid MCOs, 2022 Data
- MLRs at Washington Medicaid MCOs Average 87.2%, 2022 Data
- West Virginia SNP Membership at 32,269, Mar-23 Data
- Wyoming SNP Membership at 1,694, Mar-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Arizona Long Term Care System RFP, Proposals, Scoring, and Related Documents, 2023
- Arizona Pharmacy Benefits Management (PBM) Services RFP and Q&A, 2023
- Massachusetts One Care, Senior Care Options RFR, Nov-23
Medicaid Program Reports, Data, and Updates:
- Idaho Medicaid Managed Care Task Force Final Report, Nov-23
- Louisiana PHE Medicaid Redeterminations Monthly Report to CMS, Oct-23
- Michigan PHE Medicaid Redeterminations Monthly Reports to CMS, Oct-23
- North Dakota Medicaid Quality Strategy Plan Draft, 2024
- North Dakota PHE Medicaid Redeterminations Monthly Report to CMS, Oct-23
- Pennsylvania Section 1115 Health-Related Social Needs Waiver Draft Application, Nov-23
- Rhode Island Medicaid Managed Care Rate Certification, SFY 2024
- Texas Utilization Review in STAR+PLUS Managed Care Reports, 2018-23
- Texas Behavioral Health Strategic Plan Progress Reports, 2018-23
- Texas All Access Reports on Mental Health, 2022-23
- Texas Medicaid Behavioral Health In Lieu of Services Annual Reports, 2020-23
- Texas Medicaid CHIP Data Analytics Unit Quarterly Reports, 2018-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected]
