This week's roundup:
- In Focus: The Impact of the 340B Program on Drug Prices Charged by Manufacturers and Covered Entities

- North Carolina Appeals Ruling on Additional Community Services for Individuals with Disabilities

- New Mexico Health Plan Submits Bid for New Medicaid Managed Care Contract

- New York SMI Treatment Programs Face Over 1,000-Person Waiting List

- Oregon Reaches $17 Million Settlement with Former PBM

- Tennessee to Release Dental Benefit Management RFP in Late 2023

- Texas Releases STAR & CHIP Managed Care Services RFP

- Wisconsin Receives Approval to Continue Exchange Plan Reinsurance Program Through 2028

- HHS Releases Medicaid, CHIP FMAP for Fiscal 2024

- Defense Misses Deadline for Announcing Tricare Contract Awards

- Prime Therapeutics Completes Acquisition of Magellan Rx Management from Centene

In Focus
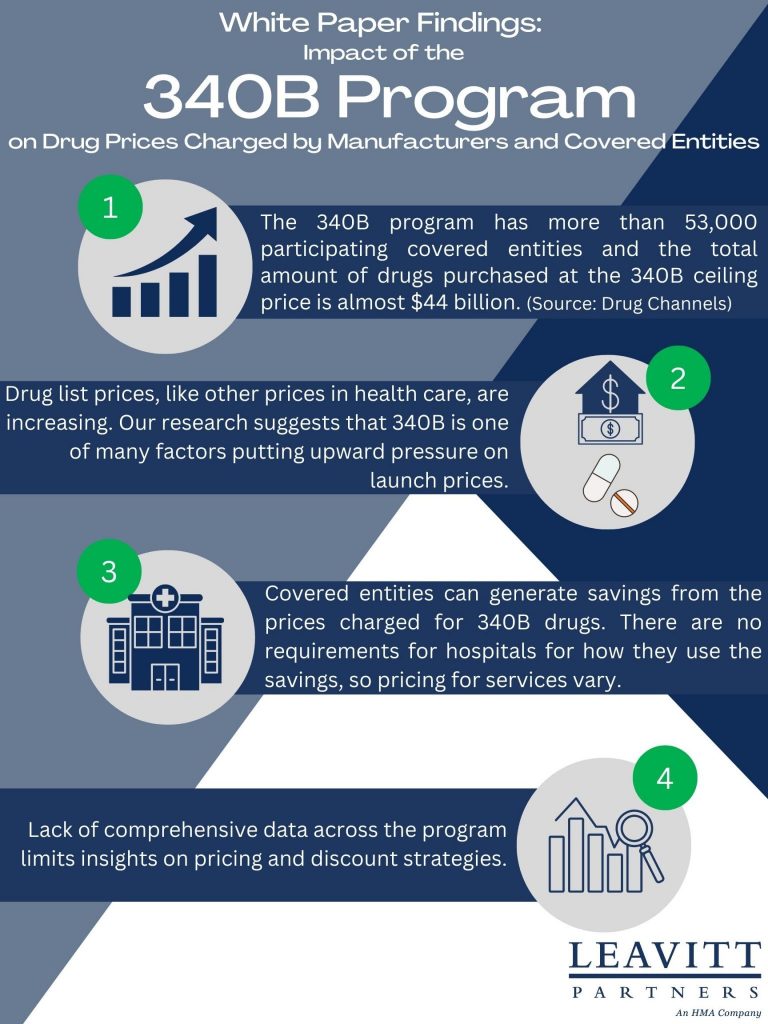
The Impact of the 340B Program on Drug Prices Charged by Manufacturers and Covered Entities
This week, our In Focus highlights a Leavitt Partners white paper, The Impact of the 340B Program on Drug Prices Charged by Manufacturers and Covered Entities, published in November 2022. Leavitt Partners examined publicly available resources to determine the 340B Drug Pricing Program’s (340B) impact on drug prices charged by both covered entities and pharmaceutical manufacturers. To answer these questions, Leavitt Partners undertook a comprehensive literature review of publicly available governmental reports, peer-reviewed journal articles, white papers, news articles, and other publicly available sources to identify the degree to which, and to what extent, the 340B program may impact drug prices. To supplement this literature review, Leavitt Partners also conducted interviews with ten subject matter experts representing the perspectives of covered entities (including Federally Qualified Health Centers, Ryan White Clinics, and Disproportionate Share Hospitals) and drug manufacturers, as well as the analysis of health economists and academic researchers.
Insights/Key Findings:
- The 340B program is a mandatory program for pharmaceutical manufacturers wishing to participate in the Medicaid drug rebate program. Today, the program has more than 53,000 participating covered entities and the total amount of drugs purchased at the 340B ceiling price under the program is almost $44 billion (Drug Channels).
- Drug list prices, like other prices in health care, are increasing. The research for this white paper suggests that 340B is one of many factors putting upward pressure on launch prices.
- Covered entities can generate savings from the prices charged for 340B drugs. There are no requirements for hospitals for how they use the savings, so pricing for services vary.
- Lack of comprehensive data across the program limits insights on pricing and discount strategies.
HMA Roundup
Maryland
Maryland Congressional Delegates Urge State to Seek CCBHC Planning Grant. Members of the Maryland congressional delegation urged the state on December 1, 2022, to apply for a Certified Community Behavioral Health Center (CCBHC) planning grant from the U.S. Substance Abuse and Mental Health Services Administration. The request came in a letter to the Maryland Secretary of Health Dennis Schrader. Grant applications are due by December 19, the last opportunity to participate in the program until 2026. Read More
Maine
Maine Emergency Medical Services Face Crisis, Commission Finds. The Sun Journal reported on December 5, 2022, that Maine’s emergency medical services are struggling from low Medicaid and Medicare reimbursements and high costs for providing services, according to the final report from a state commission. The 17-person commission, established by state law, recommends the state legislature approve an additional $76 million per year for the next five years, largely to shore up transportation services. Read More
Mississippi
Mississippi Senator to Introduce Bill Extending Postpartum Medicaid Coverage from 60 Days to 12 Months. The Daily Journal reported on December 2, 2022, that Mississippi Senate Medicaid Chairman Kevin Blackwell (R-Southaven) intends to file a bill to extend postpartum Medicaid coverage from 60 days to 12 months in the 2023 legislative session. State House Speaker Philip Gunn (R-Clinton) has said he will oppose the bill and would only consider it if the state Division of Medicaid publicly supports it. Read More
North Carolina
North Carolina Appeals Ruling on Additional Community Services for Individuals with Disabilities. The Associated Press reported on December 1, 2022, that North Carolina appealed a federal court order, which directed the state to increase access to community services for individuals with intellectual and development disabilities (IDD) who otherwise live at institutions. The directive calls for stopping new admissions of individuals with IDD at state-run development centers, private intermediate care facilities, and certain adult care homes by January 2028. Read More
New Mexico
New Mexico Health Plan Submits Bid for New Medicaid Managed Care Contract. Health Payer Specialist reported on December 2, 2022, incumbent Blue Cross Blue Shield of New Mexico has submitted a bid in the state’s latest Medicaid managed care procurement. Plans had until December 2 to bid. Other incumbents, Centene/Western Sky Health Plan and Presbyterian Health, did not comment on whether they had submitted bids. The new contracts are set to be implemented January 2024. Read More
New Mexico Launches Center for Health Policy with Focus on Medicaid. The New Mexico Human Services Department announced on December 1, 2022, the launch of the New Mexico Center for Health Policy, in partnership with the University of New Mexico. The center will work to address critical health care issues, with a focus on Medicaid. Projects include updating best practices for prescription drug utilization, analyzing the impact of structural issues that impact health outcomes for Medicaid beneficiaries, and reviewing the efficacy of the state’s Medicaid early childhood visitation programs. Future projects will look at workforce development for Medicaid programs. Read More
New York
New York Home Care Advocates Worry Medicaid Independent Assessor Could Create Delays for Patients. Crain’s New York reported on December 2, 2022, that home care and consumer-directed personal care advocates are expressing concern that New York’s Independent Assessor (NYIA) for home care program eligibility will create delays for patients seeking care. The NYIA contract, held by Maximus Health Services, was implemented on December 1. Read More
New York SMI Treatment Programs Face Over 1,000-Person Waiting List. Crain’s New York reported on December 1, 2022, that more than 1,000 individuals in New York City are on waiting lists for community programs to treat serious mental illness (SMI), including 800 awaiting care from one of the city’s 65 assertive community treatment teams. The community treatment teams provide a range of services to treat SMI, with special teams for justice-involved populations, homeless individuals, and individuals “with a high degree of transience.” Read More
Oregon
Oregon Reaches $17 Million Settlement with Former PBM. The Oregon Department of Justice announced on December 6, 2022, a $17 million agreement to settle claims that Centene overcharged the state Medicaid program while serving as the pharmacy benefit manager (PBM). The state argued that Centene failed to provide pharmacy discounts, leading to higher fees paid to the PBM. Centene also provides Medicaid managed care services to the state through its Trillium Community Health Plan subsidiary. Read More
Tennessee
Tennessee to Release Dental Benefit Management RFP in Late 2023. The Tennessee Division of TennCare announced that a request for proposals (RFP) for the state’s Dental Benefits Management (DBM) Program will be released in the fourth quarter of 2023. TennCare intends to select a contractor to provide management services for the state’s five DBM programs, which cover adult and child TennCare enrollees, children enrolled in the CoverKids program, and adults with intellectual or developmental disabilities. DentaQuest holds the state’s current DBM contract. Read More
Texas
Texas Releases STAR & CHIP Managed Care Services RFP. The Texas Health and Human Services Commission (HHSC) released on December 7, 2022, a request for proposals (RFP) for the State of Texas Access Reform (STAR) and Children’s Health Insurance Program (CHIP) Managed Care programs, which serve pregnant women and children, as well as SSI adults in rural service areas. HHSC intents to award six-year contracts to at least three managed care organizations, with three, two-year renewal options. Prior STAR & CHIP program contracts were valued at roughly $9.7 billion. There are currently 15 incumbents, with Elevance, Centene/Superior, and Texas Children’s Health Plan providing coverage for more than half of program enrollees. Proposals are due by February 17, 2023. Read More
Virginia
Virginia to Merge Two Managed Care Programs On January 1. The News & Advance reported on November 30, 2022, that Virginia will merge its two Medicaid managed care programs, Medallion 4 and Commonwealth Coordinated Care Plus, into one program called Cardinal Care, on January 1, 2023. Medallion 4 serves children, pregnant women, and adults, while Commonwealth Coordinated Care Plus serves older adults who also are on Medicare, children and adults with disabilities, and individuals in long term care. Read More
Wisconsin
Wisconsin Receives Federal Approval to Continue Exchange Plan Reinsurance Program Through 2028. WisPolitics.com reported on December 5, 2022, that the Centers for Medicare & Medicaid Services approved Wisconsin’s application for an extension of its Section 1332 State Innovation Waiver, which will allow the state to continue operating the Wisconsin Healthcare Stability Plan (WIHSP) for another five years through 2028. WIHSP is a reinsurance program that covers a portion of certain high-cost Exchange enrollee claims. Read More
Wisconsin Submits Section 1115 BadgerCare Reform Waiver Extension. The Centers for Medicare & Medicaid Services announced on December 2, 2022, that Wisconsin submitted a Section 1115 waiver application to extend its BadgerCare Reform demonstration, currently set to expire on December 31, 2023, for four years through 2028. The demonstration provides Medicaid benefits for non-pregnant, non-disabled, non-elderly childless adults up to 100 percent of the federal poverty level (FPL) and provides full coverage of residential substance use disorder treatment for all BadgerCare Plus and Medicaid members. The waiver includes monthly premiums, healthy behavior incentives, copayments, and additional eligibility criteria for childless adults with incomes between 50 and 100 percent of the FPL. The federal public comment period is open until January 1, 2023. Read More
National
18 Million Medicaid Members Could Lose Coverage After PHE, Study Finds. Becker’s Payer Issues reported on December 7, 2022, that 18 million Medicaid members could lose coverage when the federal public health emergency (PHE) expires, according to a study by the Urban Institute and Robert Wood Johnson Foundation (RWJF). That is up two million from an earlier Urban-RWJF projection in March. The study said that most disenrolled members will move to other coverage, including 3.2 million children who will transition to Children’s Health Insurance Program plans. About 3.8 million are expected to become uninsured, including 1.5 million who will be eligible for Exchange subsidies plans but will not enroll. Read More
Medicaid Plans Look to Exchanges to Offset Enrollment Declines After PHE Ends. Bloomberg Law reported on December 7, 2022, that Medicaid plans are looking to Exchange enrollment to help offset membership losses when the public health emergency (PHE) ends. Bloomberg analyst Duane Wright projects, for example, that Elevance Health could offset 10 percent of projected Medicaid enrollment losses by enrolling 25 percent of its former Medicaid members in Exchange plans. Read More
CMS Proposes Electronic Prior Authorization by 2026 for Publicly Sponsored Plans. Fierce Healthcare reported on December 6, 2022, that the Centers for Medicare & Medicaid Services (CMS) proposed a rule that would require Medicaid, Children’s Health Insurance Program, Medicare Advantage, and Exchange plans to implement electronic prior authorization systems by January 2026. The rule would also require that plans respond to urgent prior authorization requests within 72 hours and include justifications for denied requests. Read More
HHS Releases Medicaid, CHIP FMAP for Fiscal 2024. The U.S. Department of Health and Human Services published on December 5, 2022, the fiscal 2024 Medicaid and Children’s Health Insurance Program (CHIP) federal medical assistance percentages (FMAP) to the Federal Register. The FMAPs will be effective October 1, 2023, to September 30, 2024. Read More
MACPAC Meeting Scheduled for December 8, 9. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on December 5, 2022, that its next meeting will be held on December 8-9. Among the topics for discussion will be policy options for improving race and ethnicity data collection and reporting in Medicaid, recent developments in Medicaid Section 1115 demonstration waivers and implications for future policy, MACPAC’s required annual analysis of Disproportionate Share Hospital allotments, and potential nursing facility payment principles and recommendations. Read More
Medicaid DSH Payments Went to Hospitals That Did Not Meet Criteria in 2015, Study Finds. Modern Healthcare reported on December 5, 2022, that almost 32 percent of the $14.5 billion in Medicaid disproportionate share hospital (DSH) payments in 2015 went to hospitals that did not meet certain statutory criteria, according to a study from Health Affairs. More than three percent went to hospitals that did not meet any of the DSH criteria. Read More
Pharmacy Chains Appeal $650 Million Federal Court Ruling for Fueling Opioid Epidemic. Becker’s Hospital Review reported on December 5, 2022, that CVS, Walgreens, and Walmart have appealed a 2021 U.S. Circuit Court ruling ordering the pharmacies to pay $650 million for spurring the opioid epidemic in Turnbull and Lake counties in Ohio. The appeal claims there is a lack of evidence demonstrating violations of the federal Controlled Substance Act and that other pharmacy chains should contribute to the fines. Read More
Defense Misses Deadline for Announcing Tricare Contract Awards. Health Payer Specialist reported on December 2, 2022, that the U.S. Department of Defense missed a November deadline to announce new Tricare contract winners. Current incumbents are Humana and Centene. The new contract is set to go into effect in January 2024 and run for nine years. Read More
Senate Committee Considers Policy to Increase Physical, Behavioral Health Parity. Becker’s Payer Issues reported on December 2, 2022, that the U.S. Senate Finance Committee is discussing policies to improve physical and mental health coverage parity in Medicare and Medicaid, including updated provider directory requirements for Medicare Advantage and Medicaid managed care plans. The committee is also considering requiring the Government Accountability Office to compare behavioral health cost sharing and utilization differences in Medicare Advantage and traditional Medicare. Read More
Hospitals Oppose National Directory of Healthcare Providers. The American Hospital Association (AHA) announced on December 1, 2022, its opposition to a national directory of health care providers (NDH), citing administrative burdens and questioning the directory’s usefulness in response to a Centers for Medicare & Medicaid Service (CMS) request for information. AHA believes CMS should wait to establish NDH until it is clear how it would fit within existing provider databases. Read More
Republican Lawmakers Call for Speedy Medicaid Redeterminations. Health Payer Specialist reported on December 2, 2022, that Republican lawmakers are reportedly supporting a proposal calling for speedy Medicaid redeterminations after the public health emergency (PHE) ends, which is currently scheduled for January 11. A projected 15 million to 25 million Medicaid beneficiaries could be disenrolled when the PHE ends. Read More
One Third of Dual Eligibles Lose Medicaid Coverage in First Year of Enrollment, Study Finds. The Kaiser Family Foundation (KFF) reported on November 30, 2022, that 38 percent of newly-enrolled dual eligibles in 2018 lost Medicaid coverage for at least one month during the first year of enrollment, according to a KFF study. The Centers for Medicare & Medicaid Services proposed a rule this year that could reduce coverage losses in the dual eligible population. Read More
Industry News
UnitedHealth Acquisition of LHC Group Is Delayed Until Early 2023. Health Payer Specialist reported on December 7, 2022, that UnitedHealth Group’s acquisition of home healthcare company LHC Group has been delayed until the first quarter of 2023, the company confirmed. UnitedHealth announced its agreement to acquire LHC for $5.4 billion in March 2022. Read More
BayMark Health Services Acquires Nashville Recovery. BayMark Health Services announced on December 6, 2022, the acquisition of Nashville Recovery, a provider of office-based opioid treatment programs. Baymark operates more than 70 opioid treatment programs in 19 states. Read More
Advocate Aurora Health, Atrium Health Merge After Approval from IL Regulatory Agency. Modern Healthcare reported on December 2, 2022, that Advocate Aurora Health and Atrium Health completed their merger following approval from Illinois regulators. The board of the combined company, called Advocate Health, will be comprised evenly of members from both organizations. Atrium Health chief executive Eugene Woods and Advocate Aurora chief executive Jim Skogsbergh will jointly lead the organization until Skogsbergh retires in 18 months. The combined company has 67 hospitals and $27 billion in annual revenues. Read More
Prime Therapeutics Completes Acquisition of Magellan Rx Management from Centene. Managed Healthcare Executive reported on December 5, 2022, that Prime Therapeutics, the Minnesota-based pharmacy benefit manager, completed its acquisition of Magellan Rx Management from Centene for $1.35 billion. Centene acquired Megallan Rx in January 2022 through the acquisition of Magellan Health. Magellan Rx serves about 1.7 million members. Read More
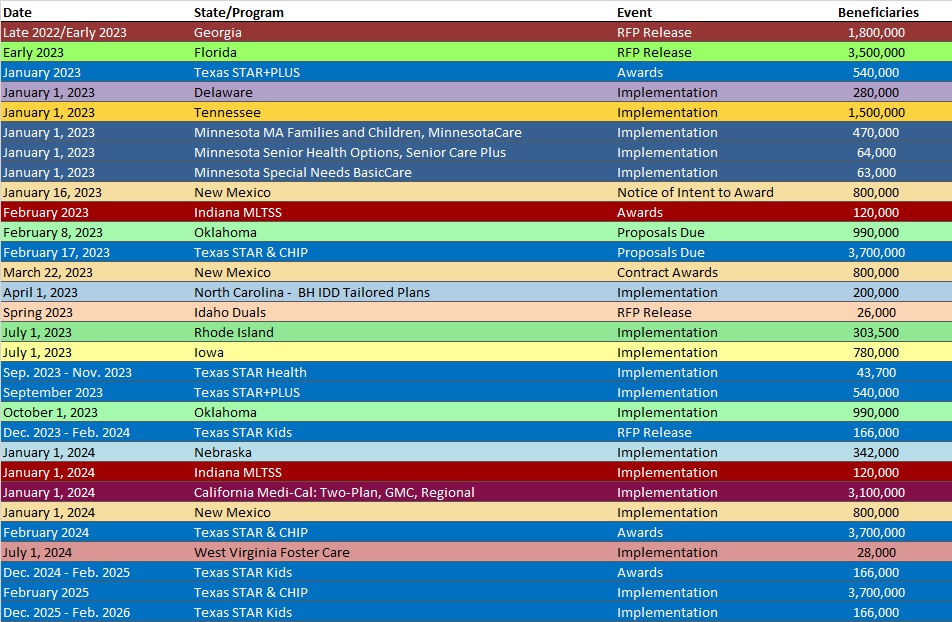
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Indiana Medicaid Managed Care Enrollment Is Up 7.6%, Sep-22 Data
- Louisiana Medicaid Managed Care Enrollment is Up 4.3%, Sep-22 Data
- Michigan Medicaid Managed Care Enrollment is Up 3.2%, Sep-22 Data
- Michigan Dual Demo Enrollment is Up 4.5%, Sep-22 Data
- Missouri Medicaid Managed Care Enrollment is Up 22.6%, Sep-22 Data
- Nevada Medicaid Managed Care Enrollment is Up 4.9%, Jul-22 Data
- New Mexico Medicaid Managed Care Enrollment is Up 2%, Sep-22 Data
- Oregon Medicaid Managed Care Enrollment is Up 5%, Aug-22 Data
- South Carolina Medicaid Managed Care Enrollment is Up 4.3%, Jul-22 Data
- South Carolina Dual Demo Enrollment is Down 8.6%, Jul-22 Data
- Washington Medicaid Managed Care Enrollment is Up 3.9%, Aug-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Connecticut Dental Administrative Services Organization Contract, 2019-20
- Texas STAR, CHIP Managed Care RFP, 2022
Medicaid Program Reports, Data, and Updates:
- Indiana Medicaid Advisory Committee Meeting Materials, Nov-22
- Tennessee Managed Care Organization Financial Reports, 2022
- Texas All Access Report on Mental Health, Dec-22
- Texas Behavioral Health Strategic Plan Progress Reports, 2018-22
- Texas HHS Quality Measures and Value-Based Payments Annual Reports, 2018-22
- Texas Medicaid Benefits and Services Not Provided Under the Managed Care Model Report, Dec-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.