This week's roundup:
- North Carolina Releases Foster Care Specialty Plan Program RFP

- Florida Delays Awards for Medicaid Managed Care ITN

- Georgia Proposes Bill to Establish Study Committee to Examine Private Option Medicaid Expansion Waiver

- Iowa Senate Advances Bills Altering Postpartum Medicaid Coverage, MOMS Program

- Kentucky Senate Advances Bill to Cover Midwife Services Under Medicaid

- Maryland Awards Behavioral Health ASO Contract to Elevance

- Missouri Supreme Court Rules Against Blocking Medicaid Payments to Planned Parenthood

- Nebraska Legislature Considers Bill to Expand Medicaid Coverage of Anti-obesity Medications

- Pennsylvania Submits Section 1115 Waiver Application Addressing Health-related Social Needs

- CMS Issue Brief Finds Doulas, Community Health Workers Improve Postpartum Outcomes

- CMS Releases Preliminary CMS-64 2023 Medicaid, CHIP Expenditure Report

- CMS Issues Final Rule Imposing Restrictions on DSH Payments

- Point32Health to Acquire Health New England

- Bon Secours Mercy Health Enters Joint Venture with Compassus

- Brightside Announces New Medicaid, Medicare Partnerships to Expand Telehealth for Mental Health Services

In Focus
North Carolina Releases Foster Care Specialty Plan Program RFP
This week, our In Focus section reviews the statewide North Carolina request for proposals (RFP) for the new Children and Families Specialty Plan (CFSP), which the North Carolina Department of Health and Human Services (DHHS) released on February 7, 2024. The plan will provide physical health, behavioral health, intellectual and developmental disability, long-term care, and pharmacy services to children, youth, and families that the child welfare system serves. Implementation is scheduled for December 1.
Background
North Carolina implemented Medicaid managed care on July 1, 2021, after working on a plan to transition individuals from fee-for-service to managed care since 2015. CFSP is one of the four types of integrated Medicaid managed care plans the state will contract with to serve Medicaid beneficiaries. The other three are Standard Plans, the Behavioral Health and Intellectual/Developmental Disability (BH IDD) Tailored Plans, and the Eastern Band of Cherokee Indians Tribal Option.
Standard Plans are operated by one of two types of Medicaid managed care organizations (MCOs): statewide commercial plans (CPs) or regional provider-led entities (PLEs). The state awarded contracts to four CPs, the maximum allowed under the procurement, and one PLE. AmeriHealth Caritas North Carolina, Blue Cross and Blue Shield of North Carolina, UnitedHealthcare of North Carolina, and WellCare of North Carolina serve beneficiaries across six Medicaid managed care regions. A regional contract with provider-led Carolina Complete Health, a partnership between the North Carolina Medical Society and Centene, covers Regions 3, 4, and 5. The total value of the contracts is approximately $6.4 billion. The plans serve more than 2 million members as of year-end 2023.
The state plans to implement BH IDD Tailored Plans July 1. Tailored plans will be provided through the awarded local management entity-managed care organizations (LME-MCOs): Alliance Health, Partners Health Management, Trillium Health Resources, and Vaya Health. Implementation has been delayed multiple times since 2022. As a result, the state issued a directive last year to dissolve the Sandhills Center and consolidate Eastpointe and Trillium Health Resources to hasten the delayed rollout. The tailored plans are expected to cover approximately 160,000 beneficiaries.
Details about the CFSP
The following populations will be enrolled automatically in CFSP:
- Beneficiaries who are in foster care
- Beneficiaries who are receiving adoption assistance
- Beneficiaries enrolled in the former foster youth eligibility group
- The minor children of enrolled parents
The following populations will be eligible for enrollment in CFSP during contract year two:
- Parents, caretaker relatives, guardians and custodians with children in foster care
- Minor siblings of beneficiaries in foster care
- Adults identified on an open Child Protective Services (CPS) In-Home Family Services Agreement case and any minor children living in the same household
- Adults identified in an open Eastern Band of Cherokee Indians Department of Public Health and Human Services Family Safety program case and any children living in the same household
- Any other beneficiary that has been involved with the child welfare system who could benefit from enrollment
RFP
The state will award the contract to a single statewide managed care plan. Applicant MCOs will need to develop strategies for engaging with historically marginalized populations, addressing health disparities, and incorporating health equity. Technical proposals will be evaluated based on the following criteria:
- Medicaid Managed Care Qualifications and Experience
- Medicaid Managed Care Program Administration
- Administration and management
- Program operations
- Claims and encounter management
- Financial requirements
- Compliance
- Technical specifications
- Historically underutilized businesses
- Diversity, equity, and inclusion
- Integrated and Coordinated Delivery of Services
- Members and recipients
- Benefits and services
- Providers
- Stakeholder engagement
- Comprehensive Care Management
- Care management
- Quality and value
Timeline
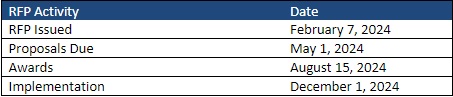
The CFSP data book and capitation rate methodology will be released March 1, with an overview for presentation at a pre-proposal conference on March 7. Proposals are due May 1 and awards are expected to be announced August 15. Contracts are scheduled to run December 1, 2024, through June 30, 2028, with one additional option year. The RFP indicates that the Department will work with awardee to establish an appropriate launch date.
HMA Roundup
Arizona
Arizona Receives Federal Approval to Increase CHIP Income Limit. The Arizona Health Care Cost Containment System announced on February 20, 2024, that it has received federal approval to increase the upper income limit of KidsCare, the state’s Children’s Health Insurance Program (CHIP), to 225 percent of the federal poverty level, beginning April 1. The state has also received approval to pay parents as caregivers of their minor children with disabilities enrolled in Arizona’s Long Term Care System, which will now be a permanent feature of the program. Read More
Colorado
Colorado Disenrolls 67,967 Medicaid Beneficiaries During January Redeterminations. The Colorado Department of Health Care Policy & Financing disenrolled approximately 67,967 Medicaid beneficiaries during January eligibility redeterminations, including 45,566 due to procedural reasons and 22,401 due to ineligibility. Read More
Connecticut
Connecticut Medicaid Reimbursement Rates Generally Lower Compared to Peer States, Medicare. CT Mirror reported on February 19, 2024, that Connecticut’s Medicaid reimbursement rates were generally lower when benchmarked against five peer state averages and Medicare, according to a phase-one rate study report released by the Connecticut Department of Social Services. The peer states included Maine, Massachusetts, New Jersey, New York, and Oregon. Overall, Connecticut paid less than a peer state benchmark for 85 percent of services analyzed and less than a Medicare-based benchmark for 94 percent of services analyzed. The rate study phase two report is due January 1, 2025. Read More
Florida
Florida Delays Awards for Medicaid Managed Care ITN. The Florida Agency for Health Care Administration released on February 15, 2024, an addendum extending the anticipated award date for the Statewide Medicaid Managed Care procurement from February 23 to March 25. The bidders are AmeriHealth Caritas, CareSource/ImagineCare, Centene/Sunshine State Health Plan, CVS/Aetna, Elevance/Simply Healthcare Plans, Florida Community Care, Humana, Molina, Sentara Care Alliance, South Florida Community Care Network/Community Care Plan, and UnitedHealthcare. Contracts are expected to take effect October 1. Read More
Florida House Committee Advances Bill to Boost Physician Workforce. Health News Florida reported on February 16, 2024, that the Florida House Health & Human Services Committee advanced a bill, sponsored by House Majority Leader Michael Grant (R-Port Charlotte), that would offer $717 million to expand medical residency programs, increase the number of doctors in the state, and provide increased access to student loan programs. A similar bill, sponsored by Senate Health Policy Chairwoman Colleen Burton (R-Lakeland), passed in the Senate. The bill will next head to the House floor for review. These bills comprise Senate President Kathleen Passidomo’s “Live Healthy” legislation package aimed at improving healthcare access. Read More
Georgia
Georgia Bill Would Establish Study Committee to Examine Private Option Medicaid Expansion Waiver. The Atlanta Journal Constitution reported on February 20, 2024, that Georgia House Speaker Jon Burns (R-Newington) introduced a bill that would establish a study committee to examine a waiver to enroll additional Medicaid beneficiaries through a private option. The Comprehensive Health Coverage Commission would include nine members who would examine a similar waiver program implemented in Arkansas that allowed the state to utilize expansion dollars to purchase private insurance for uninsured individuals. The push for a study committee indicates that state lawmakers are unlikely to advance Medicaid expansion legislation this year. Read More
Iowa
Iowa Senate Advances Bills Altering Postpartum Medicaid Coverage, MOMS Program. The Iowa Capital Dispatch reported on February 19, 2024, that the Iowa Senate has advanced two bills, one of which would extend postpartum Medicaid coverage to 12 months for families. The bill would limit eligibility for Medicaid coverage of birth and postpartum care from 380 percent of the federal poverty level under current law to 215 percent. It is estimated that 1,300 women and 400 infants would lose Medicaid coverage per month under the new income restrictions. The second bill would allow the Iowa Department of Health and Human Services to directly oversee the More Options for Maternal Support (MOMS) program and contract with providers, removing the previous requirement to hire a third-party administrator. Read More
Kentucky
Kentucky Senate Advances Bill to Cover Midwife Services Under Medicaid. News From The States reported on February 16, 2024, that the Kentucky Senate passed a bill that would allow Medicaid to cover licensed certified professional midwife services for women with low-risk pregnancy. Licensed midwives may offer prenatal, postpartum, and labor and delivery services. The bill now moves to the House. Read More
Maryland
Maryland Awards Behavioral Health ASO Contract to Elevance. The Maryland Department of General Services announced on February 14, 2024, that Maryland has awarded Carelon, an Elevance subsidiary, the state’s administrative services organization (ASO) contract for the Public Behavioral Health System (PBHS). The PBHS provides mental health and substance use disorder services to Medicaid members. The five-year contract is valued at a total of $339.6 million. The incumbent is United/Optum. Read More
Missouri
Missouri Supreme Court Rules Against Blocking Medicaid Payments to Planned Parenthood. The Missouri Independent reported on February 14, 2024, that the Missouri Supreme Court has ruled that a 2022 budget bill, which prohibits Medicaid from paying for any health care services from a provider that also performs abortion, was unconstitutional. In 2020, the Missouri Supreme Court ruled in favor of Planned Parenthood in a similar dispute. Read More
Nebraska
Nebraska Legislature Advances Bill to Increase Medicaid Hospital Payment Rates. Nebraska Public Media reported on February 15, 2024, that the Nebraska Legislature advanced a provider tax bill, sponsored by Senator Mike Jacobson (R-North Platte) and 19 co-sponsors, that could garner $1 billion in additional funding, raise Medicaid payment rates for hospitals, and reduce cuts in services. The bill would require hospitals to pay an assessment of up to 6 percent of net patient revenue, which would serve as the match for federal funding. The bill will next receive the second of three reviews from the legislature. Read More
Legislature Considers Bill to Expand Medicaid Coverage of Anti-obesity Medications. The Nebraska Examiner reported on February 15, 2024, that the Nebraska legislature is considering a bill, sponsored by Senator Mark Riepe (R-Ralston), that would expand Medicaid coverage of anti-obesity medications. The bill is expected to cost $3.6 million annually and is aimed at improving health outcomes for the more than 30 percent of residents affected by obesity. The bill is currently in the Health and Human Services Committee. Read More
Legislature Advances Bill to Expand Medicaid Prenatal Care Reimbursement. The Omaha World-Herald reported on February 14, 2024, that the Nebraska legislature advanced a bill to establish the Nebraska Prenatal Plus Program. The program, aimed at at-risk mothers who are Medicaid recipients, would expand Medicaid reimbursements for prenatal care to include nutrition counseling and targeted case management beginning six months prior to birth. Legislators adopted an amendment to end the program in June 2028. The bill will next undergo the second of three reviews by the Legislature. Read More
New York
New York Proposed Budget Amendment to Increase Consumer Directed Personal Assistance Program Oversight. The New York Post reported on February 16, 2024, that New York Governor Kathy Hochul submitted a fiscal 2025 proposed budget amendment which makes changes to the Consumer Directed Personal Assistance Program (CDPAP), aimed at minimizing fraud. The amendment includes limiting the number of financial intermediaries that can operate in the state, limiting the number of hours those employed can work, and allowing the state Department of Health expanded oversight and regulatory powers. The administration estimates the proposed changes to the CDPAP will save the state around $100 million per year. Read More
Pennsylvania
Pennsylvania Submits Section 1115 Waiver Application Addressing Health-related Social Needs. The Centers for Medicare & Medicaid Services announced on February 15, 2024, that Pennsylvania submitted a new Section 1115 waiver application, titled “Bridges to Success: Keystones of Health For Pennsylvania.” The waiver is intended to address health-related social needs and specifically aims to reduce healthcare costs and expand services to individuals in the following focus areas: individuals reentering the community from correctional facilities; recipients in need of stable housing, food and nutrition services; and continuous Medicaid coverage for children under age six. If approved, the state would administer the waiver from January 1, 2025, through January 1, 2030. The federal comment period will be open through March 16. Read More
Utah
Utah Senate Considers Bill Allowing Medicaid Coverage for Native Healing Services. The Salt Lake Tribune reported on February 19, 2024, that the Utah Senate is considering a bill that would allow Medicaid to cover traditional Native healing services. Utah would be the fourth state to request federal approval to reimburse for Native healing practices, following New Mexico which is currently approved, and California and Arizona, which have pending requests. It is estimated that about 1,100 Medicaid eligible Native Americans will use the traditional healing services. Read More
Virginia
Virginia Senate Passes Medicaid Initiative Bill for Undocumented Children. The Post Millennial reported on February 14, 2024, that the Virginia Senate passed the “Cover All Kids” Medicaid initiative which would expand a Medicaid style program to about 88,000 children who are undocumented in the state. The plan will now move to the House of Delegates for consideration. Read More
National
CMS Issues Final Rule Imposing Restrictions on DSH Payments. Modern Healthcare reported on February 20, 2024, that the Centers for Medicare & Medicaid Services (CMS) has issued a final rule setting new restrictions on how Medicaid disproportionate share hospital (DSH) payments are calculated and distributed. Under the rule, hospitals will only be able to account for patients with Medicaid as their primary payer, although safety-net hospitals with the highest concentrations of low-income patients are exempt. Read More
Surprise Billing Negotiations Surpass Federal Estimates, CMS Finds. Fierce Healthcare reported on February 16, 2024, that the number of surprise billing negotiations that reached the independent dispute resolution phase of the No Surprises Act protocols surpassed federal estimates in the first six months of 2023, according to a report from the Centers for Medicare & Medicaid Services (CMS). The number of cases totaled 288,810 during this period, which was 13 times higher than projections for the entire year. CMS also reported that a small number of entities drove the majority of the cases, with the top 10 parties representing 78 percent of all cases that went to dispute resolution, including large practice management companies, revenue cycle management firms, and medical practices. In the first half of 2023, three entities were responsible for starting 58 percent of the disputes, SCP Health, Team Health, and Radiology Partners. Providers won in 77 percent of cases, while health insurers won in 23 percent of cases. Read More
CMS Issue Brief Finds Doulas, Community Health Workers Improve Postpartum Outcomes. The Centers for Medicare & Medicaid Services (CMS) released on February 16, 2024, a brief highlighting findings from the Improving Postpartum Care Affinity Group from 2021 through 2023. Several states found that doulas, community health workers, and home visits reduced postpartum complications and improved maternal and infant outcomes. Maternity case management services also ensured beneficiaries received the services and supports they needed. States that participated include Kentucky, Georgia, Oklahoma, South Carolina, Texas, Kansas, Missouri, Montana, and Wyoming. Read More
HHS, FTC Release RFI to Investigate Generic Drug Shortages. CQ reported on February 14, 2024, that the U.S. Department of Health and Human Services (HHS) and the Federal Trade Commission (FTC) have released a joint request for information (RFI) to seek feedback on how group purchasing organizations and drug wholesalers affect generic drug shortages. The RFI mainly focuses on how market concentration and contracting terms affect drug supply and whether violations of antitrust and price discrimination laws are present. Read More
CMS Releases Preliminary CMS-64 2023 Medicaid, CHIP Expenditure Report. The Centers for Medicare & Medicaid Services (CMS) released the Medicaid Budget and Expenditure System/State Children’s Health Insurance Budget and Expenditure System expenditure report for 2023. The report contains preliminary data from state Form CMS-64 filings, with breakdowns of expenditures for Medicaid, Medicaid administration, and CHIP. If you’re interested in becoming an HMAIS subscriber to gain access, contact Andrea Maresca at amaresca@healthmanagement.com.
Industry News
Point32Health to Acquire Health New England. Point32Health announced on February 15, 2024, that it will acquire Health New England, a subsidiary of Baystate Health. Health New England offers plans in the commercial, Medicaid, and Medicare markets, and serves approximately 180,000 individuals in Massachusetts. Point32Health offers various plans to 1.9 million individuals across five states and owns Harvard Pilgrim Health Care and Tufts Health Plan. The agreement is subject to regulatory approval. Read More
Bon Secours Mercy Health Enters Joint Venture with Compassus. Modern Healthcare reported on February 16, 2024, that Bon Secours Mercy Health is entering into a 50-50 joint venture with Tennessee-based Compassus, which provides home health, hospice, palliative care and infusion services in 29 states. Bon Secours Mercy Health will transition management of 10 home health agencies and 11 hospice operations in five states to Compassus. Financial terms for the joint venture have not been disclosed and are subject to approval from state and federal regulators. The deal is expected to close in the second quarter of 2024. Read More
Community Health Systems Announces Potential $1 Billion Divestiture of Facilities. Modern Healthcare reported on February 21, 2024, that Tennessee-based Community Health Systems is considering selling more than $1 billion worth of facilities in the next few years, with at least one divestment expected to close within the year. Community Health Systems operates 71 hospitals and more than 1,000 care sites, and plans to use proceeds from the deals to make investments in core markets, debt management, and acquisitions. Read More
Brightside Announces New Medicaid, Medicare Partnerships to Expand Telehealth for Mental Health Services. Brightside Health announced on February 21, 2024, several new and expanded contracts with various payers to provide online mental health care services to serve Medicaid and Medicare beneficiaries. Brightside will newly contract with CareOregon to serve Medicaid members and with Blue Shield of California to serve Medicare Advantage members. The company will expand its contracts with Blue Cross and Blue Shield of Texas to include Medicare Advantage members and expand its contract with Centene state by state. Finally, Brightside will expand traditional Medicare to include Texas, California, Delaware, Arizona, New York, Washington, Florida, North Carolina, Michigan, and Illinois. Read More
Cigna, Centene Announce New Programs to Increase Access to Healthy Food. Health Payer Specialist reported on February 16, 2024, that Cigna Healthcare is partnering with HelloFresh’s Meals with Meaning Program to provide free meal kits for those experiencing food insecurity. Centene’s WellCare of North Carolina is enrolling its Medicaid members with chronic conditions and complex health needs into the Eat Well program, providing more than 1,600 North Carolinians with prepaid debit cards, worth $80 a month, to buy fruits and vegetables. Read More
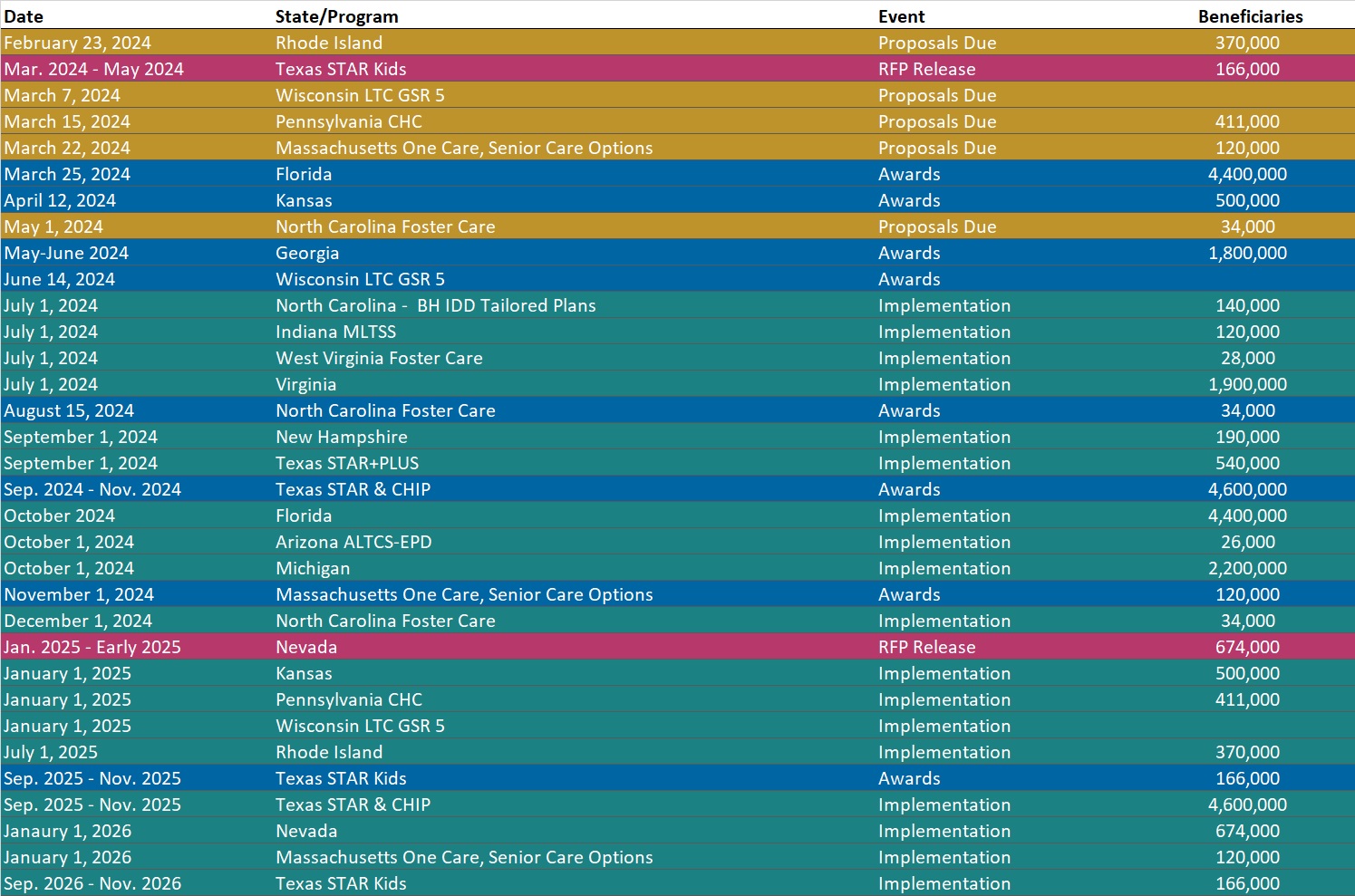
RFP Calendar
HMA News & Events
HMA Webinars:
Substance Use Disorder (SUD) Ecosystem of Care: Pivoting to Save Lives – An Overview. Wednesday, February 28, 2024, 12 PM ET. Join us for part 1 of our 5-part webinar series, “Substance Use Disorder Ecosystem of Care: Pivoting to Save Lives.” This session will introduce overarching themes of the webinar series, including the diverse pathways within the continuum of care and unravel a comprehensive framework that spans prevention, early intervention, treatment, and long-term care. The webinar will also delve into the intricate network of support systems designed to maintain life and resource individuals on their unique recovery journey, examining what is working and what we can leave behind to pivot toward what matters.
Substance Use Disorder (SUD) Ecosystem of Care: Pivoting to Save Lives Part 2 — The Role of Health Promotion and Harm Reduction Strategies. Thursday, March 14, 2024, 12 PM ET. Join us for part 2 of our 5-part webinar series, “Substance Use Disorder Ecosystem of Care: Pivoting to Save Lives.” This session offers a look at the services and support that comprise a system of care for people who are not yet in treatment. These services are often community-based and involve outreach, engagement, and meeting people where they are. As people enter treatment, experience relapse, or choose to move through different treatment modalities, health promotion and harm reduction can serve as a safety net to keep people continuously engaged.
The New Technology Add-on Payment (NTAP) Program: What Life Sciences Companies Should Know About Medicare’s Time-Limited Program in 2024. Wednesday, March 6, 2024, 12:30 PM. For biopharmaceutical, medical device, and diagnostic manufacturers, navigating market access and reimbursement in the inpatient hospital setting is a challenge in the Medicare program, where most technologies are bundled into an existing payment rate. This bundled payment methodology means that providers often lack incentives to adopt new medical technologies not already reflected in their costs. Since 2001, the Centers for Medicare & Medicaid Services have offered manufacturers of new, groundbreaking technologies the ability to apply for a New Technology Add-on Payment (NTAP) designation for their drug, device, or diagnostic that will provide hospitals with extra payments when they use the product for the 2-3 year period after market entry of product. These add-on payments are often critical in a hospital’s decision to adopt new technologies. Join Foley Hoag and The Moran Company, an HMA Company, on March 6 for a webinar dissecting the upcoming NTAP application process in 2024 and the frequently asked questions surrounding this time-limited program.
Wakely, an HMA Company, White Papers:
Impacts of the Medicare Prescription Payment Plan. CMS’s release of the August 21st HPMS memo includes draft guidance on the Medicare Prescription Payment Plan (M3P), which is a payment structure introduced in the IRA designed to spread member cost-sharing for prescription drugs across the plan year. The M3P requires all plans to offer this alternative payment plan to their members and will debut in plan year 2025. This program is designed to help elevate the financial burden of members who incur high out-of-pocket pharmacy costs early in the plan year, but at what cost to the plan sponsor? Read More
