HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- HMA Conference: Driving Change in Healthcare Delivery: HMA Spring Workshop Builds Towards Policy and Strategy Frameworks Necessary to Implement Value-based Care

- Wakely, an HMA Company, White Paper: Shadow Bundles are Coming Soon to MSSP and ACO REACH

- Alaska Receives CMS Approval to Extend Postpartum Medicaid Coverage to 12 Months

- California Awards More Than $10 Million to Residential SUD Treatment Facilities

- Florida House Agrees to Boost Physician Workforce, Increase Healthcare Innovation Grants, and Hospital At Home

- Indiana Plans to Transition 1,600 Children to Structured Family Caregiving Program

- Mississippi House Committee Advances Medicaid Expansion Bill with Work Requirement

- Montana Proposes Housing Assistance, Incentives, Re-entry Services for Medicaid Beneficiaries with Mental Health Disorders

- New Mexico Names Dana Flannery Medicaid Director

- North Carolina Legislators Push to Re-examine Law Granting Special Privileges to Hospital Authorities

- Ohio Nursing Home Associations Sue Medicaid Program Over Alleged Underfunding

- Oregon Receives Federal Approval for Limited HCBS for Seniors, Adults with Disabilities

- Texas Releases STAR Kids Draft RFP

- Washington House Considers Bill that Would Place Greater Oversight on Provider Consolidations

- Redetermination Updates: Arkansas, Iowa, Mississippi

- CMS Releases Second Evaluation of Integrated Care for Kids Model

- CareSource Seeks to Enter Wisconsin Marketplace, Acquire Local ACA Co-op Plan

In Focus
Driving Change in Healthcare Delivery: HMA Spring Workshop Builds Towards Policy and Strategy Frameworks Necessary to Implement Value-based Care
Last chance to register! Online registration closes February 28.
Federal policy frameworks establishing alternative payment models in Medicare and Medicaid have been the kick-starter of value-based care (VBC) innovation in healthcare delivery. However, employers provide health insurance to most Americans, and very few employers – with the exception of jumbo, self-insured employers – have leaned heavily into VBC. Small- and medium-sized firms rely on brokers to find an affordable health insurance plan, and often lack the resources required to negotiate more. Though the tide has been changing, our fragmented payment system has yielded only a subset voluntarily taking substantial risk for patient outcomes.
It has been said that to truly transform our American healthcare system to pay for value – improved outcomes for lower cost – it would require better alignment across public and commercial payers to support care providers in shifting their business models to take risk.
Quality and cost information are critical to implement VBC payment and delivery systems. Federal initiatives in Medicare and Medicaid have opened the door for providers, payers, and innovators to use health information to improve outcomes, with patients more engaged and more in control; the “Universal Foundation” announced by the Centers for Medicare and Medicaid Services (CMS) in 2023 seeks to align quality measures across the more than 20 CMS quality initiatives; and policies included in the 21st Century Cures Act and CMS Interoperability and Patient Access rule are creating more transparency on price and quality.
By enabling an infrastructure to measure, digitize, and share cost and quality information, federal and state governments have set the stage for greater collaboration among all purchasers – including employers – and the healthcare delivery system to redesign care that addresses health related social needs and behavioral health, ensuring that healthcare is provided equitably and sustainably . As the care delivery system is better able to deliver high value care, more employers will demand this for their workforce to provide a better benefit to their workers.
These issues, and more, will be a part of the expert-led conversation on VBC at HMA’s 2024 Spring Workshop March 5-6, in Chicago. This workshop offers a unique opportunity for payers, government officials, community organizations, vendors, and providers to have an unvarnished conversation about the challenges, lessons, and opportunities in implementing VBC. The meeting is designed to share insights, change-oriented strategies and actions that advance VBC from top industry experts, health plan executives, state and federal leaders, and policy experts.
Our working sessions will feature solutions-focused conversations among peers:
- Care delivery measures that drive outcomes, equity, population health
- Payment & risk management models for payment, pricing, attribution
- Data that is interoperable, consumer focused, deploying technology that is aligned to deliver on strategic objectives
- Policy & Strategy Frameworks at federal, state, and local levels that incentivize VBC
The closing panel will look at ways to take action through policy and collaboration to move our industry toward more sustainable approaches to healthcare payment and delivery.
To learn more and register for this unique event, please visit HMA’s 2024 Spring Workshop page. Act fast – online registration ends Wednesday, February 28!
Shadow Bundles are Coming Soon to MSSP and ACO REACH
Wakely, an HMA Company, broke down in a February 2024 white paper what shadow bundles are and potential use case for accountable care organizations (ACOs) to engage specialists. In 2021, the Centers for Medicare & Medicaid Services (CMS) set a goal of getting 100 percent of Medicare and the vast majority of Medicaid beneficiaries in an ACO by 2030 and outlined their goals as part of their strategic refresh. CMS believes engaging specialists will be a critical next step in their goal. Providing shadow bundle data is a means for CMS to equip ACOs with better insights to manage specialty care. Read More
HMA Roundup
Alaska
Alaska Receives CMS Approval to Extend Postpartum Medicaid Coverage to 12 Months. The Centers for Medicare & Medicaid Services (CMS) announced on February 23, 2024, that it has approved Alaska’s state plan amendment to extend postpartum Medicaid coverage from 60 days to 12 months, effective July 1, 2024. Read More
Arkansas
Arkansas Requests New Section 1115 Waiver for Transition-related IMD, Carceral Services. The Centers for Medicare & Medicaid Services (CMS) announced on February 28, 2024, that Arkansas has submitted a request for a new Medicaid Section 1115 demonstration, Opportunities to Test Transition-Related Strategies to Support Community Reentry from Incarceration and Institutions for Mental Disease. Under the demonstration program, medically necessary services will be covered for individuals during the first 90 days of incarceration or admission to an institution for mental disease (IMD) and the 90 days immediately prior to release from either setting. To support community reentry, the state would provide pre-release care coordination services, medication assisted treatment services, and a 30-day supply of prescription drugs to individuals leaving carceral settings. The federal comment period will be open through March 29, 2024.
Arkansas Disenrolls 3,255 Medicaid Beneficiaries During January Redeterminations. The Arkansas Department of Human Services announced in February 2024, that the state has disenrolled 3,255 Medicaid beneficiaries during January redeterminations, including 2,662 beneficiaries for procedural reasons. The state renewed Medicaid coverage for more than 35,865 beneficiaries.
California
California Awards More Than $10 Million to Residential SUD Treatment Facilities. The California Department of Health Care Services (DHCS) announced on February 22, 2024, that it has awarded more than $10 million to 25 residential substance use disorder (SUD) treatment facilities throughout the state. The funding will be used for costs associated with startup, recruitment, mentorship, and training programs to increase provider knowledge with prescribing medications for addiction treatment. Read More
Colorado
Colorado Submits Amended Application to Import Low-cost Prescriptions from Canada. Colorado Governor Jared Polis and the Colorado Department of Health Care Policy & Financing (HCPF) announced on February 27, 2024, the submission of Colorado’s amended application to the U.S. Food and Drug Administration (FDA) to import lower-cost drugs from Canada via Colorado’s Canadian Drug Importation Program. If approved, the program could save residents up to $51 million in its first three years. The state previously announced partnerships with three supply chain partners, AdiraMedica, Premier Pharmaceuticals, and Rocky Mountain Poison and Drug Safety, and released an initial application to the FDA in December 2022. Read More
Colorado Prescription Drug Affordability Board Votes to Consider Price Cap on Arthritis Drug. The Denver Post reported on February 24, 2024, that Colorado’s Prescription Drug Affordability Board voted to continue discussions to set a price ceiling on the arthritis drug Enbrel. The state will now enter a six-month process to determine a price and would be the first in the country to set a price ceiling on a drug. The price ceiling would limit how much pharmacies could pay for the drug, and patients and insurers would pay that value plus a handling fee. While the board agreed to proceed with discussions, it could decline to set a ceiling price. Read More
Delaware
Delaware Governor Requests Budget Increase for State Healthcare Programs. Delaware Public Media reported on February 24, 2024, that Delaware Governor John Carney requested that the state Department of Health and Social Services receive an 8.4 percent budget increase, including $84.2 million to address the end of the enhanced federal Medicaid funding linked to the COVID-19 public health emergency. The department is also requesting one-time supplemental funding totaling $10.4 million to help with the increased caseload for Medicaid redeterminations that are to be completed by July. Read More
Florida
Florida Lawmakers Propose to Fully Fund Medicaid Program Following End of Federal COVID Funding. The Florida Policy Institute reported on February 26, 2024, that federal funding within Florida’s Senate and House Medicaid budget proposals decreased by 7.7 percent and 7.8 percent, respectively, for fiscal year 2025. The proposed budgets both decreased by approximately four percent (approximately $1.3 billion) due to end of the public health emergency enhanced federal funding, with the Senate proposing a budget of $33.1 billion and the House proposing $33.2 billion, matching historical spending. Although both legislative chambers proposed spending increases of more than $200 million to support KidCare programs, including to fully fund caseloads, the House allocates an additional $1.2 million to increase the income eligibility threshold for KidCare coverage. Overall, the Senate included more funding to provide care to individuals on various home and community-based services waitlists, although both chambers supported recurring funding for most programs. Read More
Florida House Agrees to Boost Physician Workforce, Increase Healthcare Innovation Grants, and Hospital At Home. Florida Politics reported on February 22, 2024, that the Florida House advanced two bills aimed at boosting the state’s healthcare workforce and supporting healthcare innovation. SB 7016, sponsored by Senate Health Policy Chairwoman Colleen Burton (R-Lakeland), directs $717 million to expand medical residency programs, increase the number of doctors in the state, and provide increased access to student loan programs. SB 7018, sponsored by Senator Gayle Harrell (R-Stuart), will direct $50 million in state funding for healthcare innovation grants over the next decade. Lawmakers also agreed to allow the state’s Agency for Health Care Administration to request federal approval for Medicaid reimbursement for “Hospital at Home” services. Both bills had previously been approved by the Senate and will now head to Governor Ron DeSantis for review. Read More
Indiana
Indiana Plans to Transition 1,600 Children to Structured Family Caregiving Program. The Indiana Capital Chronicle reported on February 23, 2024, that the Indiana Family and Social Services Administration (FSSA) shared in a Medicaid Advisory Committee meeting that 1,622 children would be affected by its proposed cut of the attendant care program. FSSA noted that the number of children receiving more than 60 hours of attendant care weekly increased from 10 percent in March 2022 to 47 percent in December 2023, and costs have increased from $9.3 million to $172 million in two years. The state plans to transition families into the Structured Family Caregiving program which uses a tiered per diem reimbursement policy. FSSA is taking other steps to address the state’s budget shortfall, including declining to implement a reimbursement increase for six provider categories. Read More
Iowa
Iowa Disenrolls 2,627 Medicaid Beneficiaries During January Redeterminations. The Iowa Department of Health and Human Services on February 8, 2024, reported that it has disenrolled 2,627 Medicaid beneficiaries during January redeterminations, of those 521 were due to procedural reasons. The state has renewed coverage for 8,767 beneficiaries in January.
Kansas
Kansas Expansion Plan Costs Could be Offset by American Rescue Plan Act Funds, Study Finds. The Kansas Reflector reported on February 22, 2024, that the Kansas Health Institute (KHI) projects Governor Laura Kelly’s Medicaid expansion plan will cover an additional 152,000 individuals in the first year of implementation. KHI’s analysis also shows that the state would be eligible for $509 million in federal funding to support the expansion, which will help to fully offset state costs for expansion during the first eight years. Governor Kelly’s expansion plans have faced opposition from the Republican-controlled legislature. Read More
Louisiana
Louisiana Medicaid Beneficiaries Experienced Increase in Access to Medications for Opioid Use Disorder Between 2018 and 2021, Study Finds. The Pew Charitable Trusts reported on February 26, 2024, that utilization of medications for opioid use disorder (MOUD) increased among Medicaid beneficiaries in Louisiana between 2018 and 2021 following numerous state policy changes, according to a Health Affairs study. Researchers found that the number of patients in residential treatment facilities receiving MOUD increased from 8 percent in 2018 to 42 percent in 2021 after lawmakers mandated that these facilities offer MOUD on-site to maintain operating licensure. Although overall use of MOUD increased from 21 percent in 2018 to 50 percent in 2021, individuals under age 20, non-white patients, and those living in rural areas had less access to MOUD than older, white, and urban populations. Read More
Massachusetts
Massachusetts Governor Suggests Steward Healthcare Transfer In-state Hospitals to New Operators. Fierce Healthcare reported on February 20, 2024, that Massachusetts Governor Maura Healey has suggested Steward Health Care imminently transfer its hospitals in the state to new operators unless sufficient staffing and supply levels are met and financial documents are disclosed. Healey also called on the system to comply with increased on-site state monitoring. The health system was given a three-day deadline to disclose system-level audited financial documents. Read More
Mississippi
Mississippi House Committee Advances Medicaid Expansion Bill with Work Requirement. Mississippi Today reported on February 27, 2024, that the Mississippi House Medicaid Committee has advanced a bill to implement a “private option” Medicaid expansion for working adults with incomes below 138 percent of the federal poverty line. Eligible adults will be able to choose between at least two qualified health plans through the Marketplace. The state would receive an extra $600 million in federal Medicaid funds during the first two years of expansion, which would cover the state’s share for four years. Hospitals and managed care organizations would then have increased taxes to cover the state’s 10 percent match. The bill will now move to the House for further consideration. Read More
Mississippi Disenrolls 5,409 Medicaid Beneficiaries During January Redeterminations. Mississippi State Department of Health released data showing it has disenrolled 5,409 Medicaid beneficiaries during January redeterminations. Of those disenrolled 3,660 were due to procedural reasons. The state has renewed coverage for 25,482 Medicaid beneficiaries.
Montana
Montana Proposes Housing Assistance, Incentives, Re-entry Services for Medicaid Beneficiaries with Mental Health Disorders. The Daily Montanan reported on February 26, 2024, that Montana is proposing to offer expanded Medicaid-funded behavioral health services through a section 1115 waiver amendment as part of the state’s Healing and Ending Addiction through Recovery and Treatment (HEART) program. The new services would include Tenancy Supports, Contingency Management, and Justice-Involved Reentry Services. The housing assistance and treatment incentive programs are expected to become available in the fall, and the pre-release services in late 2025. The federal public comment period is open through March 25. Read More
New Hampshire
New Hampshire Considers Penalties for Anthem Medicare Advantage Prescription Drug Contract. Health Payer Specialist reported on February 26, 2024, that New Hampshire Governor Chris Sununu is considering penalties or termination of the state’s Medicare Advantage prescription drug contract for state retirees with Elevance-owned Anthem Blue Cross Blue Shield, which began on January 1. The state alleges unfilled or incorrect prescriptions, extra steps required, delayed hold times, and unexpected charges. Read More
New Mexico
New Mexico Names Dana Flannery Medicaid Director. The New Mexico Human Services Department announced on February 27, 2024, that Dana Flannery has been named the director for the state’s Medicaid program. Flannery previously served as senior policy advisor and assistant director of Arizona’s Medicaid agency. Read More
New York
New York Grants VNS Health $34 Million Contract to Support Individuals with SMI. Crain’s New York reported on February 28, 2024, that Midtown-based home and community health care provider VNS Health has received a $34 million contract from the city Department of Health and Mental Hygiene for its intensive mobile treatment (IMT) program. The funds will allow for two more IMT teams, which provide treatment to seriously mentally ill (SMI) New Yorkers, including medication, substance-use care, and connections to housing. It is estimated that 837 individuals can be served by IMT teams in the city at any given time. Read More
North Carolina
North Carolina Legislators Push to Re-examine Law Granting Special Privileges to Hospital Authorities. NC Health News reported on February 26, 2024, that North Carolina Senator Jim Burgin (R-Angier) and Representatives Donny Lambeth (R-Winston-Salem) and Larry Potts (R-Lexington), are calling for a re-examination of a state law that grants special privileges to hospital authorities such as Atrium Health. The law has provided hospitals such as Atrium with additional tax breaks, permission to make property owners sell to further hospital expansion, and protection from federal regulations such as antitrust damages. The legislators questioned the need for these multi-billion-dollar organizations to continue to receive these privileges and also suggested that such entities should have to perform the same transparent practices as other government entities. Read More
North Carolina Antitrust Lawsuit Against HCA, Mission Health May Proceed, Federal Judge Rules. Reuters reported on February 22, 2024, that a federal judge has denied HCA Healthcare’s motion to dismiss a class action lawsuit brought by North Carolina cities and counties related to its acquisition of Mission Health in 2019. The antitrust suit, filed in North Carolina federal court, alleges that HCA and its Mission Health system have monopolized healthcare markets in western North Carolina and artificially driven up costs for health plans. HCA denies any wrongdoing. Read More
Ohio
Ohio Nursing Home Associations Sue Medicaid Program Over Alleged Underfunding. McKnights Long-term Care News reported on February 23, 2024, that three Ohio associations have sued the Ohio Department of Medicaid (ODM) alleging that the department improperly calculated care quality incentives, resulting in financial losses of hundreds of millions of dollars. The Ohio Health Care Association, LeadingAge Ohio, and the Academy of Senior Health Services, claim that ODM’s calculation of $169 million in quality incentive increases comprises 29 percent of the increases for nursing homes passed by the state Legislature for nursing homes, rather than 60 percent. ODM maintains that this interpretation of the budget is incorrect. The Ohio Supreme Court directed the parties to pursue mediation prior to continuing further legal action. Read More
Oregon
Oregon Receives Federal Approval for Limited HCBS for Seniors, Adults with Disabilities. The Centers for Medicare & Medicaid Services (CMS) announced on February 23, 2024, that it has approved a new section 1115 demonstration named “Oregon Project Independence–Medicaid (OPI–M), which provides limited home and community-based services, including adult day services, transportation, emergency response, home delivered meals, and caregiver education training, for seniors and adults with disabilities. Eligibility standards have been expanded to include those who need assistance completing activities of daily living but do not require Medicaid nursing facility-level care and adults at risk of needing Medicaid long-term services and supports. Beneficiaries will be able to receive continuous Medicaid eligibility for up to two years. The demonstration program will run for five years, beginning on February 13, 2024. Read More
Rhode Island
Rhode Island Medicaid Managed Care Bidders Molina, Commonwealth Care Alliance Drop Out. Health Payer Specialist reported on February 28, 2024, that Molina Healthcare and Commonwealth Care Alliance have opted out of Rhode Island’s second Medicaid managed care bid, released in December 2023. Commonwealth Care Alliance cited the inclusion of services for individuals with the most significant healthcare needs as the reason for not responding. Blue Cross Blue Shield of Rhode Island, Neighborhood Health Plan of Rhode Island, Tufts/Point32Health, and UnitedHealthcare of New England all responded to the bid. The state is expected to award two or three Medicaid managed care organizations five-year contracts beginning July 1, 2025. The incumbents are Neighborhood Health Plan, Tufts, and UnitedHealthcare, serving approximately 372,000 members. Read More
South Dakota
South Dakota to Include Medicaid Work Requirement Resolution on November Ballot. ABC News reported on February 27, 2024, that the South Dakota legislature has agreed to place a Medicaid work requirement resolution on the November general election ballot, which would allow the state to apply work requirements to certain individuals in the Medicaid expansion population. The work requirement resolution, led by Senator Crabtree (R-Madison), Representative Venhuizen (R-Sioux Falls), and others, would exclude certain beneficiaries who have been diagnosed as physically or mentally disabled. The resolution passed the state House and Senate. If approved by voters, the state would need to secure approval from the federal government before implementing the policy.
Texas
Texas Releases STAR Kids Draft RFP. The Texas Health and Human Services Commission released on February 15, 2024, a draft request for proposals (RFP) for the STAR Kids program, which provides Medicaid managed care to approximately 150,000 children and youth under age 21 with disabilities. The finalized RFP will be released on March 11 and proposals are due June 6. Texas plans to award contracts to a minimum of two plans for each service area, with awards expected in August 2025. Contracts will begin in September 2026 and run for six years with three two-year renewal options. Incumbents are CVS/Aetna, Elevance/Amerigroup, Blue Cross Blue Shield of Texas, Centene/Superior Health Plan, Community First Health Plan, Cook Children’s Health Plan, Driscoll Children’s Health Plan, Texas Children’s Health Plan, and UnitedHealthcare.
Texas County to Launch $23 Million Jail Diversion Program Focused on Individuals with Mental Illness. The Texas Tribune reported on February 26, 2024, that Travis County has partnered with county mental health provider Integral Care to launch a $23 million three-year pilot program aimed at diverting those with mental illness from incarceration to a treatment facility. The first phase of the program will launch in March and includes the development of a 90-day treatment program at a 25-bed facility to provide care to individuals in crisis. The county hopes to open a permanent, larger structure by 2029 or 2030. The number of jail bookings in the county increased from 22,068 in 2021 to 28,828 in 2023. Approximately 44 percent of individuals booked into the county’s jail have a mental health condition. Read More
Washington
Washington House Considers Bill that Would Place Greater Oversight on Provider Consolidations. The Seattle Times reported on February 23, 2024, that the Washington House of Representatives is considering a bill, sponsored by Senator Emily Randall (D-Bremerton), that calls for greater oversight of healthcare mergers and acquisitions to ensure that larger hospital systems are not cutting services, increasing costs, and reducing market competition. Washington’s independent providers and small hospital systems have steadily lost money and have struggled to remain in operation. A report, prepared by Health Management Associates and published by the state Office of the Insurance Commissioner, found that healthcare consolidations may have contributed to a 49 percent increase in premiums and a 79 percent increase in deductibles between 2010 and 2020. The Senate has already passed the bill, which awaits review in the House Rules Committee. Read More
Wisconsin
CareSource Seeks to Enter Wisconsin Marketplace, Acquire Local ACA Co-op Plan. The Dayton Daily News reported on February 27, 2024, that CareSource is looking to partner with Wisconsin-based Marketplace plan, Common Ground Healthcare Cooperative, as it seeks to enter the Wisconsin Marketplace. Common Ground, an Affordable Care Act (ACA) co-op, would become a subsidiary of CareSource and exit the co-op program if the deal is approved. CareSource most recently entered the Ohio Marketplace with plans geared towards individuals with diabetes. Read More
National
CMS Releases Second Evaluation of Integrated Care for Kids Model. The Centers for Medicare & Medicaid Services (CMS) released on February 16, 2024, an evaluation report examining the performance of the Integrated Care for Kids Model, aimed at improving care and saving costs for Medicaid beneficiaries aged 20 and under, in 2022. The report found that the model’s award recipients, which include Illinois, Ohio, New York, Connecticut, New Jersey, and North Carolina, are currently implementing programs tailored to their regions, such as Alternative Payment Models (APMs) designed to integrate services and enhance care coordination. Recipients had access to varying levels of resources and noted that APM development took longer than anticipated, though all made progress with implementation. All recipients began needs screening during the first implementation year and utilized administrative data and direct screening for need determination. Read More
Congress to Remove PBM, Site-neutrality Measures from Upcoming Healthcare Legislation. Modern Healthcare reported on February 26, 2024, that Congress is expected to cut proposed legislation aimed at requiring increased transparency from pharmacy benefit managers (PBMs) and limiting their forms of compensation, as well as site-neutrality legislation that would prevent hospitals from charging the same amount for injections in outpatient as in inpatient settings. An extension of the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act of 2018 may also be cut. Instead, lawmakers would include measures that would address a Medicare cut to physician payments, delay $16 billion in reductions to Medicaid disproportionate share hospital payments for safety-net facilities, and fund federally qualified health centers. Read More
HHS Releases Two Reports Detailing HIPAA Compliance, Enforcement Efforts. The U.S. Department of Health & Human Services (HHS) Office for Civil Rights (OCR) released on February 14, 2024, two reports highlighting Health Insurance Portability and Accountability Act (HIPAA) compliance and enforcement efforts. The 2022 report on HIPAA Privacy, Security, and Breach Notification identifies 30,435 complaints alleging HIPAA violations, the method utilized to resolve complaints, and the outcome of OCR’s review of complaints. The report on Breaches of Unsecured Protected Health Information identifies the number and types of breaches of unsecured protected health information reported to HHS in 2022, actions taken to resolve breaches, and the need for health entities to comply with various HIPAA security requirements. Read More
Industry News
UPMC President, CEO Diane Holder To Retire After More Than 40 Years. UPMC announced on February 26, 2024, that Diane Holder is retiring from her roles as president and chief executive of UPMC Health Plan; president of Insurance Services; and president of Community and Ambulatory Services Division, effective at the end of 2024. Holder spent more than 40 years of her career at UPMC. Read More
UnitedHealth to Face Antitrust Investigation by DOJ. Health Payer Specialist reported on February 27, 2024, that the U.S. Department of Justice (DOJ) has launched an antitrust investigation into UnitedHealth Group out of concerns around UnitedHealth’s acquisitions and its impact on rivals and consumers. As part of the investigation, regulators are requesting information from physician groups and other healthcare industry representatives about relationships between UnitedHealthcare and its services group, Optum. Read More
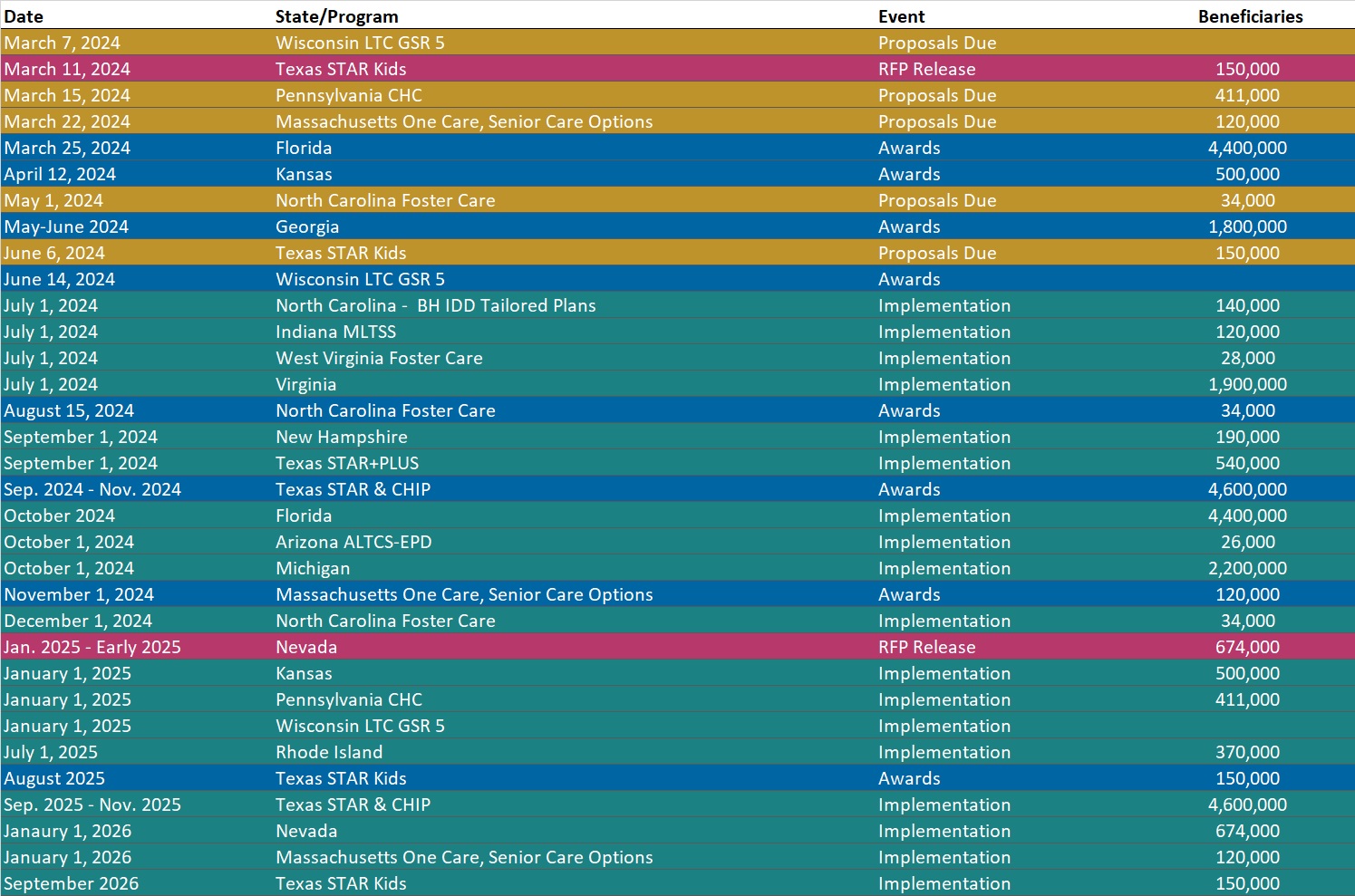
RFP Calendar
Company Announcements
MCG Press Release:
MCG Releases 28th Edition of Care Guidelines with Updates to Support Compliance with CMS’ 2024 Medicare Advantage Final Rule. Read More
HMA News & Events
HMA Webinars:
Substance Use Disorder (SUD) Ecosystem of Care: Pivoting to Save Lives Part 2 — The Role of Health Promotion and Harm Reduction Strategies. Thursday, March 14, 2024, 12 PM ET. Join us for part 2 of our 5-part webinar series, “Substance Use Disorder Ecosystem of Care: Pivoting to Save Lives.” This session offers a look at the services and support that comprise a system of care for people who are not yet in treatment. These services are often community-based and involve outreach, engagement, and meeting people where they are. As people enter treatment, experience relapse, or choose to move through different treatment modalities, health promotion and harm reduction can serve as a safety net to keep people continuously engaged. Register Here
The New Technology Add-on Payment (NTAP) Program: What Life Sciences Companies Should Know About Medicare’s Time-Limited Program in 2024. Wednesday, March 6, 2024, 12:30 PM. For biopharmaceutical, medical device, and diagnostic manufacturers, navigating market access and reimbursement in the inpatient hospital setting is a challenge in the Medicare program, where most technologies are bundled into an existing payment rate. This bundled payment methodology means that providers often lack incentives to adopt new medical technologies not already reflected in their costs. Since 2001, the Centers for Medicare & Medicaid Services have offered manufacturers of new, groundbreaking technologies the ability to apply for a New Technology Add-on Payment (NTAP) designation for their drug, device, or diagnostic that will provide hospitals with extra payments when they use the product for the 2-3 year period after market entry of product. These add-on payments are often critical in a hospital’s decision to adopt new technologies. Join Foley Hoag and The Moran Company, an HMA Company, on March 6 for a webinar dissecting the upcoming NTAP application process in 2024 and the frequently asked questions surrounding this time-limited program.
