HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Rhode Island Releases Medicaid Managed Care Program RFP

- Elizabeth Mitchell to Keynote HMA’s Spring Workshop on Value-based Care March 5-6 in Chicago

- Alabama Releases Medicaid Enterprise System Provider Management Services RFP

- Arizona Receives 3 Protests Against Medicaid ALTCS Awards

- California Medi-Cal MCO Tax Receives Federal Approval

- Florida Announces List of Bidders for Statewide Medicaid Prepaid Dental Program ITN

- Illinois to Release Medicaid Managed Care RFP in Spring 2024

- Iowa Lawmaker Files Bill to Extend Postpartum Medicaid Coverage to 12 Months

- Kansas Announces List of Bidders for Medicaid Managed Care RFP

- Missouri Lawmakers to Consider Medicaid Provider Tax Renewal

- Nebraska Lawmakers File Bill to Increase Medicaid Hospital Payment Rates

- New York Receives Federal Approval for Medicaid Section 1115 Waiver Amendment to Support Health Equity, Health-related Social Needs

- Oregon Medicaid CCOs to Invest $25 Million to Support Youth Behavioral Health Projects

- Washington Behavioral Health-related Outcomes Remain Similar Between Integrated, Carve-out Models, Study Finds

- West Virginia Medicaid Beneficiaries Face Barriers to Dental Care Access, Stakeholder Analysis Finds

- CMS Releases ARPA State Spending Plan Summaries

- Health Insurance Marketplace Enrollment Exceeds 20 Million for 2024

- CVS Invests in WellBe Senior Medical

- Elevance Sues CMS Over Medicare Advantage Star Ratings System

- CMS to Terminate Medicare Advantage Plans in Arizona, North Carolina

In Focus
Rhode Island Releases Medicaid Managed Care Program RFP
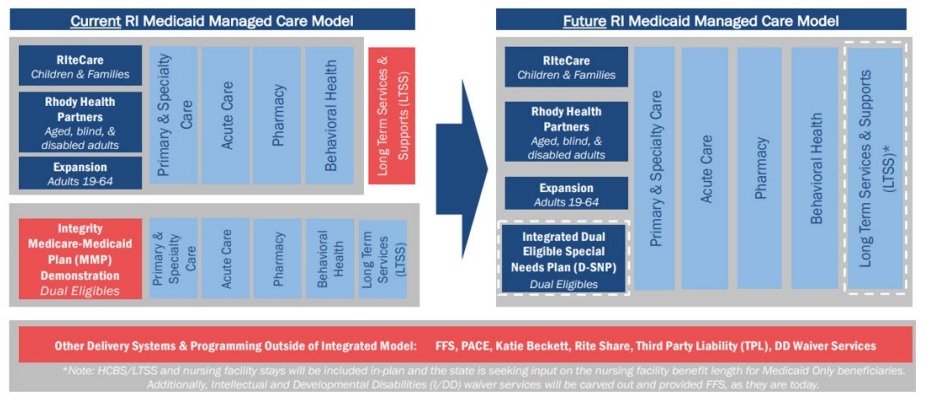
This week our In Focus section reviews the Rhode Island statewide, capitated risk-bearing Medicaid managed care program request for proposals (RFP), which the Rhode Island Executive Office of Health and Human Services (EOHHS) released December 15, 2023. New program changes will include carving in long-term services and supports (LTSS) as an in-plan benefit for all populations and expanding managed care to include people who are dually eligible for Medicare and Medicaid. Contracts are expected to be worth $2.3 billion.
Background
Rhode Island’s Medicaid managed care program, which operates under the authority of a Section 1115 waiver and Section 1932(a) state plan amendment, consists of the following programs:
- RIteCare, which serves children and families, including children with special healthcare needs
- Rhody Health Partners, which serves aged, blind, or disabled (ABD) adults
- Medicaid expansion, which serves childless adults ages 19 to 64
At present, full-benefit dual eligible (FBDE) members are not covered through the Medicaid managed care organization (MCO) contracts.
RFP
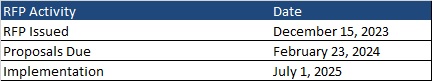
New contracts will be implemented in three phases, starting with enrollment of core populations and the addition of LTSS in-plan benefits to Medicaid managed care for Medicaid-only enrollees beginning July 1, 2025. In the second phase, current fully dual eligible members will transition to Medicaid managed care plans on January 1, 2026. All bidders will be required to offer an integrated Dual Eligible Special Needs Plan (D-SNP) and managed LTSS (MLTSS) plan to dually eligible members, as Rhode Island transitions from the Financial Alignment Initiative (FAI) Medicare-Medicaid Plan (MMP) Demonstration, which sunsets December 31, 2025. In addition, beginning January 1, 2027, default enrollment will begin for Medicaid members who become newly eligible for Medicare.
EOHHS will award contracts to two or three MCOs.
Other changes in the RFP include increasing oversight and accountability for the use of pharmacy benefit managers (PBMs); requiring that EOHHS approve contracts for MCO major subcontractors; reducing unnecessary prior authorizations, particularly for behavioral health services; increasing financial sanctions for noncompliant MCOs; and increasing investments in population health and health equity with a focus on the identification of health disparities; and other changes.
Timeline
Proposals are due February 23, 2024. The new contracts will take effect July 1, 2025, and will run through June 30, 2030, with an option to extend the agreement for up to five additional years.
Current Market
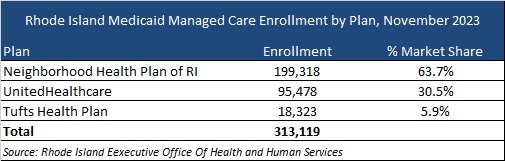
Neighborhood Health Plan, Tufts Health, and UnitedHealthcare served approximately 313,000 members as of November 2023. These MCOs have signed contract extensions through June 30, 2025.
Evaluation
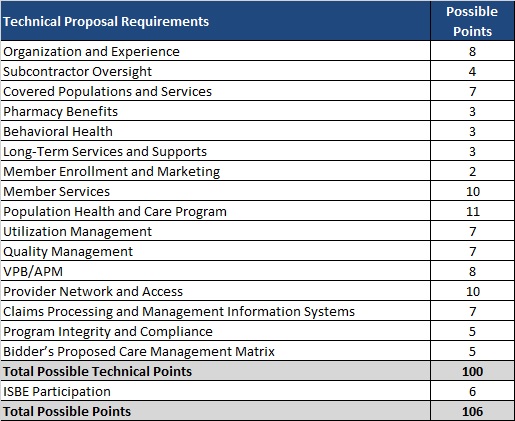
Rhode Island will not require cost proposals under this procurement, with capitation rates set by EOHHS actuaries. MCOs must meet the passing technical score of 85 points. Technical proposal requirements are shown below:
Elizabeth Mitchell to Keynote HMA’s Spring Workshop on Value-based Care March 5-6 in Chicago
Today HMA announce that Elizabeth Mitchell, President and CEO of Purchaser Business Group on Health (PBGH), will provide the keynote address “The Purchaser’s Dilemma: Why Employers Should Demand Value (and Why They Don’t)” at HMA’s 2024 Spring Workshop on value-based care, March 5-6 at the Fairmont in Chicago. In her role at PBGH, a nonprofit coalition representing nearly 40 private employers and public entities across the U.S. that collectively spend $350 billion annually purchasing healthcare services for more than 21 million Americans and their families, Mitchell represents a coalition of large purchasers – private employers and public entities – across the U.S. mobilizing to create functional health care markets that support high-quality affordable care that produces measurable outcomes. Register here.
HMA Roundup
Alabama
Alabama Releases Medicaid Enterprise System Provider Management Services RFP. The Alabama Medicaid Agency released on January 4, 2024, a request for proposals (RFP) seeking a Provider Management (PM) solutions contractor to modernize its provider enrollment and management services and integrate the solution into the state’s modular Medicaid Enterprise System (MES). The PM vendor will be responsible for enrolling, revalidating and maintaining provider management data. Proposals are due May 22, 2024, with intent to award on August 23, 2024. The contract will run for four years beginning February 1, 2025, with two two-year renewal options. Read More
Arizona
Arizona Receives 3 Protests Against Medicaid ALTCS Awards. The Arizona Health Care Cost Containment System announced on December 22, 2023, that Banner-University Family Care, Mercy Care Plan, and Blue Cross Blue Shield of Arizona Health Choice have filed protests over the contracts awarded for the Arizona Long Term Care System Elderly and Physically Disabled program. Arizona awarded contracts to Centene/Health Net Access and UnitedHealthcare Community Plan. Contracts will run from October 1, 2024, through September 30, 2027, with options not exceeding a total contract period of seven years. Read More
California
California Medi-Cal MCO Tax Receives Federal Approval. The California Department of Health Care Services (DHCS) announced on January 3, 2024, that the Centers for Medicare & Medicaid Services has approved the state’s Medi-Cal managed care organization (MCO) tax federal waiver application, which allows DHCS to utilize MCO tax revenue to implement provider rate increases and other investments to improve access to care, quality, and equity. Specifically, rates for primary care, maternity care, and non-specialty mental health services will be increased to at least 87.5 percent of Medicare rates effective January 1, 2024, while a second phase of increases and investments will go into effect January 1, 2025. The tax is expected to generate $19.4 billion in state funding from April 1, 2023, through December 31, 2026. Read More
Florida
Florida Announces List of Bidders for Statewide Medicaid Prepaid Dental Program ITN. The Florida Agency for Health Care Administration announced on January 8, 2024, the list of bidders for its Medicaid Prepaid Dental Program invitation to negotiate (ITN). The bidders are Avēsis of Florida, DentaQuest of Florida, Liberty Dental Plan of Florida, and Managed Care of North America (MCNA) Healthcare. Providers will have the opportunity to comment on respondents until January 22. Incumbents are DentaQuest, Liberty, and MCNA. Awards are anticipated to be announced March 29, 2024. Read More
Senate President Rejects Medicaid Expansion. The Florida Phoenix reported on January 9, 2024, that Florida Senate President Kathleen Passidomo (R-Naples) opposed discussions of Medicaid expansion during remarks on the first day of the 2024 legislative session. Passidomo’s comments come after Florida Representative Dotie Joseph (D-Miami-Dade) filed HB 1529, which would have expanded Medicaid effective July 1, 2024. Passidomo instead supports the “Live Healthy” legislation, a package of bills aimed at expanding access to care through retention of healthcare workers, a student loan reimbursement program, and more. Read More
Florida Secures Approval for Importation of Prescription Drugs from Canada. The Daytona Beach News-Journal reported on January 6, 2024, that the U.S. Food and Drug Administration (FDA) approved a plan to allow Florida to import cheaper prescription drugs from Canada for two years. The plan, which Florida proposed in 2020, is intended to increase availability of drugs to treat HIV/AIDS and mental illness in the Medicaid program, the prison system, and Florida Department of Children and Families facilities. Prior to importation, Florida must submit further information regarding the drugs and ensure that the drugs are FDA compliant. Read More
Florida Lawmaker Files Bill to Expand Medicaid. The Florida Phoenix reported on January 8, 2024, that Florida Representative Dotie Joseph (D-Miami-Dade) filed HB 1529, which would expand Medicaid, effective July 1, 2024. Democrats in the state legislature have indicated plans to focus on Medicaid expansion during the 2024 legislative session. Read More
Idaho
Idaho Governor Proposes Medicaid Expansion Work Requirement, Unveils Fiscal 2025 Medicaid Budget. The Idaho Capital Sun reported on January 9, 2024, that Idaho Governor Brad Little plans to pursue a work requirement for the state’s Medicaid expansion population after a previous attempt in 2019 failed to receive approval from the federal government. Democrats oppose the initiative and polls of potential voters showed that 73 percent of respondents did not want the Medicaid expansion program to change. Little also released the fiscal 2025 Medicaid budget, which consists of $4.7 billion and maintains the current spending level. Read More
Illinois
Illinois to Release Medicaid Managed Care RFP in Spring 2024. The Illinois Department of Healthcare and Family Services announced plans to re-procure its Medicaid managed care contracts in Spring 2024. Current contracts expire December 31, 2025. The incumbents are CVS/Aetna, Blue Cross Blue Shield of Illinois, Humana, Centene/Meridian Health Plan, Molina, and Cook County’s CountyCare Health Plan. Read More
Illinois Health and Social Services Costs Rise by 32 Percent Between 2019 and 2023, Report Finds. The Black Chronicle reported on January 5, 2024, that Illinois’ cost for health and social services increased from $31 billion in 2019 to $48.7 billion in 2023, representing a 32 percent increase in funding, according to an Illinois State Comptroller budget report. Health and social services include programs such as Medicaid and Temporary Assistance for Needy Families. Read More
Iowa
Iowa Lawmaker Files Bill to Extend Postpartum Medicaid Coverage to 12 Months. The Business Record reported on January 9, 2024, that Iowa Representative Ann Meyer (R-Fort Dodge) introduced a bill that would extend postpartum Medicaid coverage to 12 months. The state currently allows for 60 days of postpartum coverage and is one of three states that have not implemented a one-year extension of postpartum Medicaid coverage. The bill has been referred to the Health and Human Services committee. Read More
Kansas
Kansas Announces List of Bidders for Medicaid Managed Care RFP. Health Payer Specialist reported on January 8, 2024, that the Kansas Department of Administration has released the list of bidders for its KanCare Medicaid and CHIP managed care request for proposals (RFP): CVS/Aetna, Blue Cross and Blue Shield of Kansas/Healthy Blue, CareSource, Centene/Sunflower State Health Plan, Molina, UCare, and UnitedHealthcare. Aetna, Centene, and UnitedHealthcare are incumbents. Awards are anticipated to be announced April 12, 2024. Read More
Missouri
Missouri Lawmakers to Consider Medicaid Provider Tax Renewal. The Missouri Independent reported on January 5, 2023, that Missouri’s legislature is scheduled to consider renewals of the ground ambulance, nursing facility, Medicaid managed care organization, hospital, pharmacy, and intermediate care facility for the intellectually disabled provider taxes, also known as Federal Reimbursement Allowances (FRAs) this year. The FRA program provides funding for Medicaid, including a tax on hospitals accounting for $2.2 billion in payments for Medicaid, and taxes on nursing homes, ambulance companies and pharmacies, worth about $560 million annually. Read More
Nebraska
Nebraska Lawmakers File Bill to Increase Medicaid Hospital Payment Rates. The Omaha World-Herald reported on January 9, 2024, that Nebraska Senator Mike Jacobson (R-North Platte) and 19 co-sponsors introduced a bill, titled the Hospital Quality Assurance and Access Assessment Act, that could garner more than $500 million in federal Medicaid dollars, raise Medicaid payment rates for hospitals, and reduce cuts in services. The bill would require hospitals to pay an assessment of up to 6 percent of net patient revenue, which would serve as the match for federal funding. Read More
New Hampshire
New Hampshire House Republicans Block Permanent Medicaid Expansion Legislation. The New Hampshire Bulletin reported on January 4, 2024, that New Hampshire House Republicans rejected legislation that would have permanently continued the state’s Medicaid expansion program, estimated to provide nearly 57,000 low-income residents health insurance. Last year the legislature agreed to language included in Senate Bill 263 which extends the Medicaid expansion program for seven years. Read More
New York
New York Receives Federal Approval for Medicaid Section 1115 Waiver Amendment to Support Health Equity, Health-related Social Needs. The Centers for Medicare & Medicaid Services (CMS) approved on January 9, 2024, an amendment to New York’s Medicaid Redesign Team Section 1115 waiver which will support health equity measures, address health-related social needs, and strengthen access to primary and behavioral health care. The demonstration will be funded using $7.5 billion over three years. The amendment is effective through March 31, 2027. Read More
Medicaid Enrollment Increase May Add $1.5 Billion to Fiscal 2024 Budget, Report Finds. The Office of the New York State Comptroller released on January 4, 2024, a report which found that New York may face an additional $1.5 billion in state share Medicaid costs in fiscal 2024 due to higher than anticipated enrollment levels. Medicaid enrollment is expected to surpass previous projections by 274,755 members by the end of 2024, which would increase spending by $1.1 billion. Costs would rise to approximately $1.5 billion if 10 percent of individuals who failed to renew coverage pursue renewal at a later time. Read More
Oregon
Oregon Medicaid CCOs to Invest $25 Million to Support Youth Behavioral Health Projects. The Oregon Capital Chronicle reported on January 4, 2024, that Oregon’s 16 Medicaid insurers, known as coordinated care organizations (CCOs), will provide a total of $25 million from their profits to fund youth behavioral health projects at the request of Oregon Governor Tina Kotek. The investment will fund more than 100 new beds in youth facilities across the state. Read More
Oregon Ombuds Program Recommends Improvements to Child, Youth Community-Based Mental Health. The Oregon Health Authority (OHA) announced on January 3, 2024, that the Ombuds Program, which provides recommendations for Oregon’s Medicaid programs, released its second half of 2023 report detailing areas of improvement regarding child and youth mental health. Specifically, the report suggests that OHA implement statewide networks for inpatient and outpatient mental health services, prioritize funding for community-based care, develop culturally specific services, strengthen the peer workforce, and create an independent advocacy office. The Ombuds Program will formally present recommendations to the Oregon Health Policy Board on January 9, 2024. Read More
South Carolina
South Carolina Reaches $25.9 Million Settlement With Centene Over Medicaid Allegations. Health Payer Intelligence reported on January 4, 2024, that Centene will pay South Carolina $25.9 million to settle allegations that the company overcharged the state’s Medicaid program for pharmacy services. The settlement also resolves allegations Centene misrepresented the true cost of services, failed to disclose discounts to South Carolina, and filed improper reporting to the state about its pharmacy benefit services. The agreement requires a commitment from Centene to comply with state laws and to provide full transparency related to pharmacy benefit claims payment. Centene agreed to the terms in the settlement but denies any wrongdoing. Read More
Washington
Washington Behavioral Health-related Outcomes Remain Similar Between Integrated, Carve-out Models, Study Finds. Behavioral Health Business reported on January 3, 2024, that there were no significant changes in Washington’s behavioral health-related utilization or quality when comparing integrated managed care (IMC) in Washington Medicaid and behavioral carve-out models between 2014 and 2019, according to a study published in JAMA. Washington had a staggered rollout of the IMC program that began in 2016. The study authors suggest that states seeking to improve clinical integration may need to also focus on investments in workforce recruitment and training and strengthening contracting and data analytics. Read More
West Virginia
West Virginia Medicaid Beneficiaries Face Barriers to Dental Care Access, Stakeholder Analysis Finds. WV News reported on January 5, 2024, that West Virginia Medicaid beneficiaries face several barriers to dental care, including long wait times and provider shortages, according to a recent mystery shopper analysis conducted by the West Virginia Oral Health Coalition and Harmony Health Foundation. The analysis, which examined care sites in 36 of the state’s 55 counties, found that 28.5 percent of dental care sites accepted Medicaid recipients. Barriers to access were greater for individuals in rural areas or individuals with intellectual and developmental disabilities (IDD). The analysis included recommendations to incorporate mobile dental practices, interprofessional oral health care, training focused on treating individuals with IDD, and expansion of dental coverage through the state legislature. Read More
National
Health Insurance Marketplace Enrollment Exceeds 20 Million for 2024. The Centers for Medicare & Medicaid Services announced on January 10, 2024, that nearly 20.4 million individuals have enrolled in a health insurance Marketplace plan for 2024, including 15.5 million for the 32 states using Healthcare.gov. Approximately 3.7 million people (18 percent) are new Marketplace consumers for 2024, and approximately 16.6 million (82 percent) are returning consumers. The Marketplace open enrollment period for HealthCare.gov ends January 16, 2024. Read More
CMS Releases ARPA State Spending Plan Summaries. The Centers for Medicare & Medicaid Services (CMS) announced on January 8, 2024, the release of the American Rescue Plan Act (ARPA) state spending plan summaries of Medicaid expenditures for home and community-based services between October 1, 2022, and December 31, 2022. Read More
Industry News
CVS Invests in WellBe Senior Medical. Modern Healthcare reported on January 8, 2024, that CVS Health Ventures invested an undisclosed amount in senior primary care provider WellBe Senior Medical, intended to accelerate WellBe’s national expansion. WellBe has been contracting with Aetna since 2020 in a capitated risk arrangement to provide home-based healthcare to Medicare Advantage members with chronic conditions. WellBe currently serves 107,000 Medicare Advantage beneficiaries in Illinois, Georgia, Utah, Ohio, West Virginia, and Pennsylvania. Read More
Elevance Sues CMS Over Medicare Advantage Star Ratings System. Modern Healthcare reported on January 8, 2024, that Elevance Health and its subsidiairies filed a lawsuit against the Centers for Medicare & Medicaid Services (CMS) in an effort to overturn recent changes to the Medicare Advantage star ratings system. Elevance criticized the rating system’s introduction of the Tukey Outer Fence Outlier Deletion Method to maintain stability and alleges CMS did not follow proper administrative procedures when promulgating the rules. The lawsuit also claims the guardrail requirement is applied to simulated 2023 cut points instead of actual 2023 cut points, which decreases the star ratings. CMS have not yet responded to the lawsuit. Read More
CMS to Terminate Medicare Advantage Plans in Arizona, North Carolina. Modern Healthcare reported on January 8, 2024, that the Centers for Medicare & Medicaid Services (CMS) will terminate Centene Medicare Advantage (MA) plans WellCare Health Insurance of Arizona and WellCare Health Insurance of North Carolina due to poor star ratings. The two plans, which comprised less than 2 percent of Centene’s MA membership, will suspend enrollment and marketing effective January 12 and be officially terminated on December 31. Read More
AmeriHealth Caritas Names Kelly Munson as President, CEO. AmeriHealth Caritas announced on January 8, 2024, that Kelly Munson has been named president and chief executive, effective February 1. Munson previously served as president of CVS-owned Aetna Medicaid. Read More
Rite Aid Sale of PBM Elixer Solutions to MedImpact Healthcare Systems Moves Forward. Modern Healthcare reported on January 9, 2024, that a bankruptcy court approved the sale of Rite Aid’s pharmacy benefit manager (PBM) Elixer Solutions to MedImpact Healthcare Systems for $575 million. The transaction, expected to close in the first quarter of 2024, follows Rite Aid’s filing for Chapter 11 bankruptcy protection last October. Read More
Elevance Health to Acquire Paragon Healthcare. Elevance Health announced on January 4, 2024, that it will acquire Paragon Healthcare, an ambulatory and home infusion provider to more than 35,000 individuals across eight states. The acquisition is expected to close in the first half of 2024. Paragon Healthcare will operate within Carelon, Elevance’s health services subsidiary. Read More
Acentra Health Acquires EAP Consultants. Virginia-based Acentra Health announced on January 4, 2024, that it has acquired Georgia-based EAP Consultants, a workplace mental health and well-being company known as Espyr. Acentra plans to serve new and existing clients in government health care agencies with Espyr’s portfolio of employee assistance programs providing mental health and well-being services. Read More
RFP Calendar

HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Alabama Medicaid Fee for Service vs. Managed Care Penetration, 2014-22
- MLRs at Arizona Medicaid MCOs Average 88.3%, 2022 Data
- California Medicaid Managed Care Enrollment is Up 8.3%, Jun-23 Data
- Colorado RAE Enrollment is Down 16.7%, Nov-23 Data
- Idaho Medicaid Fee for Service vs. Managed Care Penetration, 2014-22
- Louisiana Medicaid Fee for Service vs. Managed Care Penetration, 2014-22
- Maryland Medicaid Managed Care Enrollment Is Down 1.1%, Oct-23 Data
- Missouri Medicaid Managed Care Enrollment is Down 2.2%, Nov-23 Data
- Nebraska Medicaid Fee for Service vs. Managed Care Penetration, 2014-22
- New Jersey Medicaid Fee for Service vs. Managed Care Penetration, 2014-22
- Rhode Island Medicaid Fee for Service vs. Managed Care Penetration, 2014-22
- Tennessee Medicaid Managed Care Enrollment is Down 4.1%, Nov-23 Data
- Washington Medicaid Managed Care Enrollment is Down 9.8%, Sep-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alabama Medicaid Enterprise System Provider Management Services RFP, Jan-24
- Alabama Medicaid Agency Integrated Care Networks RFP and Related Documents, 2023
- Kansas KanCare Medicaid & CHIP Capitated Managed Care RFP and Bidders List, 2023-24
- New Jersey D-SNP Contracts, 2016-22
- New Mexico Turquoise Care Managed Care RFP, Proposals, Evaluation Materials, and Related Documents, 2022-23
Medicaid Program Reports, Data, and Updates:
- Alabama Medicaid Agency Annual Reports, 2012-21
- Illinois Interim Annual Comprehensive Financial Report, SFY 2023
- New York Medicaid Redesign Team (MRT) 1115 Waiver, Proposed Amendments, Approval, Denial, and Related Documents, 2015-24
- New York Medicaid Continuous Coverage Unwinding Financial Risks Report, Jan-24
- Oregon Health Authority Ombuds Program Report, 2Q23
- Rhode Island Medicaid Managed Care Rate Certifications, SFY 2024
- Rhode Island Medicaid Expenditure Reports, SFY 2020-22
- Texas HHS Permanency Planning and Family-based Alternatives Reports, 2020-24
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected].
