This week's roundup:
- In Focus: 2025 State of the State Addresses, Part 2: Evolving Healthcare Priorities Across the Nation
- Michigan Seeks Public Feedback on Behavioral Healthcare Access Ahead of PIHP Reprocurement
- Ohio Submits Section 1115 Demonstration to Add Work Requirements to Medicaid Expansion
- South Dakota Senate Advances Medicaid Expansion Funding 2026 Ballot Measure
- CMS Rescinds Medicaid, CHIP HRSN Guidance
- HHS Announces Policy Narrowing Public Input on Policies
- CVS Sells Medicare Shared Savings Program to Wellvana
- CareSource to Acquire New York-Based Long-Term Care Plan
- More News Here
In Focus
2025 State of the State Addresses, Part 2: Evolving Healthcare Priorities Across the Nation
This week, our In Focus section reviews priorities outlined in recent State of the State addresses, building on an earlier article: A Closer Look at Gubernatorial Healthcare Priorities: 2025 State of the State Address Overview. We examine specific proposals from the governors of Illinois, Indiana, New Mexico, and South Carolina, as detailed in the Health Management Associates Information Services (HMAIS) report, 2025 State of the States Overview. These states offer examples of the trending policy changes and investments governors intend to make, providing valuable insights into the evolving healthcare landscape.
Key Trends in Governors’ Budgets
State of the State addresses provide insights into governors’ priorities, reflecting state budgets, multiyear initiatives, and changes in federal policies and funding. These priorities signal strategic shifts healthcare stakeholders must navigate to remain aligned with the evolving state and federal policy landscapes. Common themes that Health Management Associates (HMA) is tracking this year include healthcare affordability, Medicaid work requirements, workforce shortages, and enhanced oversight of healthcare entities.
Highlights by State
Illinois Gov. J.B. Pritzker delivered a 2025 State of the State Address on February 19, 2025, during which he presented his executive budget proposal for fiscal year (FY) 2026 and discussed strengthening oversight of healthcare entities like pharmacy benefit managers (PBMs) and health insurers. Governor Pritzker introduced the Prescription Drug Affordability Act, which seeks to further regulate PBMs, reduce drug costs, and protect independent pharmacists. More specifically, it would give the state Department of Insurance full statutory authority to examine PBM records and require these organizations to comply with annual auditing and reporting requirements. The governor also called for a ban on prior authorization for behavioral healthcare and proposed requiring insurance companies to reimburse patients for reasonable travel costs for medical appointments when the distance they must travel exceeds network adequacy requirements.
Pritzker’s budget allocations include:
- $191.8 million to support the Certified Community Behavioral Health Clinic (CCBHC) Medicaid Demonstration Program
- $27.9 million to maintain the state’s maternal and child home health programs
- $27.7 million to support nonhospital facilities that provide psychiatric care to people younger than 21 years old
- $132 million for Medicaid-like coverage for undocumented adults ages 65 and older
- A shift in funding from the state’s Exchange to a State-Based Marketplace, which would end use of the federal platform
In addition, the budget plan eliminates funding for Medicaid-like coverage for undocumented adults ages 42−64, which cost approximately $420 million in one year.
Indiana Gov. Mike Braun delivered his address on January 29, 2025, during which he discussed his support for state legislation that would address healthcare costs. Governor Braun urged the legislature to pass multiple bills, including:
- House Bill (HB) 1003: Specifies that the state’s Medicaid Fraud Control Unit (MCFU) may investigate provider fraud, insurer fraud, and duplicate billing and would require more healthcare price transparency, stop anticompetitive practices that drive up prices, and put an end to surprise billing
- Senate Bill (SB) 3: Would mandate that third party administrators, PBMs, employee benefit consultants, and insurance providers acting on behalf of plan sponsors have a fiduciary duty to the plan sponsors
- HB 1004: Would bolster oversight of nonprofit hospital financials
The governor also encouraged the legislature to support efforts focused on PBM reforms.
Governor Braun’s proposed budget for the 2025−27 biennium recommends a general fund appropriation of more than $5 billion in FY 2025−26 and $5.3 billion in FY 2026−27 for the state Office of Medicaid Policy and Planning. Moreover, the state is still managing the effects of a nearly $1 billion shortfall it identified in the Medicaid budget in FY 2024. The Indiana Family and Social Services Administration predicts total Medicaid expenditures will reach nearly $21 billion in FY 2025, up 6.4 percent from $19 billion in 2024 and will likely increase by at least another $1 billion in both 2026 and 2027.
New Mexico Gov. Michelle Lujan Grisham delivered her 2025 State of the State Address on January 21, 2025, wherein she discussed the new state Health Care Authority (HCA), which launched in July 2024. According to Governor Grisham, the HCA has helped the state to increase Medicaid provider rates, create a Health Care Affordability Fund, and expand the Health Care Professional Loan Repayment Program. To continue with HCA’s work, the governor announced that in March 2025, the state will be sending more than $1 billion to New Mexico hospitals through the Medicaid provider tax. She also recommended that the state legislature approve $50 million in additional funding for the Rural Health Care Delivery Fund, which supports getting new and expanded primary, behavioral, maternal and child, and specialty healthcare services into rural areas.
In her proposed FY 2026 budget, the governor recommends:
- $13 million in recurring funds to increase reimbursement rates up to 150 percent of Medicare rates
- $5.3 million for the Program of All-Inclusive Care for the Elderly (PACE)
- $2.5 million for increased assisted living facility rates
- $2.9 million to increase behavioral health rates for non-Medicare equivalents
- $30 million annually over three years to expand Medicaid services, including medical respite for people who are homeless, food support for certain individuals who pregnant, infrastructure to provide medical services to people who are justice-involved, and infrastructure to provide housing and food supports.
In addition, the budget recommends a $100 million special appropriation to address behavioral health needs, which will fund the 988 program, an investment to secure a federal match for the CCBHC Initiative, more drug and alcohol treatment services at the New Mexico Behavioral Health Institute, and medical and behavioral health providers at the Corrections Department.
South Carolina Gov. Henry McMaster delivered his 2025 State of the State Address on January 29, 2025, in which he discussed the state’s siloed health and human services delivery system, which he said creates a difficult landscape to navigate for people with physical disabilities, special needs, and mental health issues. Governor McMaster said the state must make immediate changes to the Department of Mental Health and Department of Disabilities and Special Needs and proposed making the boards of commissioners that run the departments directly accountable to the governor.
The governor’s proposed FY 2025−26 budget highlighted his priority of reimplementing Medicaid work requirements through a Section 1115 demonstration waiver, which the state previously had in place during President Donald Trump’s first administration. Governor McMaster has already requested an expedited approval of the demonstration, which would expand Medicaid eligibility to 100 percent of the federal poverty level (FPL) for parents who are working or going to school. Under South Carolina’s existing eligibility rules, parents no longer qualify for Medicaid if they earn more than 67 percent of the FPL. The work and school requirements would only apply to parents with incomes of between 67 percent and 100 percent of the FPL.
The budget also recommends approximately $79 million in recurring funds to support the state’s Medicaid program. Those funds would be allocated as follows:
- $5.7 million toward increasing behavioral health provider payment rates
- $5.4 million toward increasing opioid use disorder provider reimbursement rates
- $10 million toward reducing waiting lists for home and community-based services
- $2.4 million toward intensive partial hospitalization and outpatient behavioral health programs
In addition, the budget recommends funding for the Department of Public Health and $1.6 million in nonrecurring funds and $625,000 in recurring funds for the Healthy Moms, Healthy Babies program and its mobile maternity care vehicle.
Connect With Us
HMAIS has prepared a comprehensive report summarizing each State of the State address and governors’ proposed budgets, which is available to HMAIS subscribers. It also comprises a section highlighting trends in the issues covered in each speech, including maternal health, substance use disorder, Medicaid work requirements, prescription drug prices, and provider rates.
HMA supports healthcare stakeholders in responding to these developments, offering strategic guidance and expertise to help navigate the evolving policy landscape and align with the shifting priorities outlined in these addresses. Contact Andrea Maresca and Maddie McCarthy for more information about the report or to connect with one of HMA’s state policy and market experts.
HMA Roundup
Maryland
Maryland Lawmakers Introduce Bill to Require Medicaid Coverage of Weight Loss Drugs. CBS News reported on March 4, 2025, that Maryland Senate Minority Leader Steve Hershey (R-Kent) and Senator John Mautz (R-Talbot) have introduced a bill seeking Medicaid coverage of weight loss drugs. Senate Bill 867 would require Medicaid to provide comprehensive coverage for obesity treatment, including behavioral therapy, bariatric surgery, and any drug approved by the Food and Drug Administration (FDA) for use in chronic weight management for patients with obesity. The Maryland Department of Health estimates covering this treatment would cost more than $200 million per year, but the bill sponsors argue the cost would be lower. If passed, coverage would begin July 1, 2026.
Maryland Medicaid Managed Care Plan Loses NCQA Accreditation. The Associated Press reported on February 28, 2025, that the National Committee for Quality Assurance has suspended the accreditation of Priority Partners, Maryland’s largest Medicaid managed care organization serving 350,000, nearly a quarter, of the state’s enrollees. The suspension will not affect benefits for current enrollees, however. Beginning March 17, 2025, enrollees will have a 60-day window to switch to another plan, and Priority Partners will not be able to take on new enrollees. Details of the suspension are not public, but it will remain in place until Priority Partners implements a corrective action plan and undergoes a resurvey.
Massachusetts
Massachusetts Medicaid Agency Suspends Enrollment in MCO. The Boston Globe reported on March 4, 2025, that MassHealth suspended the Medicaid managed care organization Commonwealth Care Alliance (CCA) from taking on new enrollees in November 2024 as the insurer faces ongoing multimillion dollar operating losses. MassHealth is monitoring CCA’s financial situation. Disability advocates suggest MassHealth should appoint a receiver to oversee the insurer. CCA serves nearly 50,000 Massachusetts residents dually enrolled in Medicaid and Medicare.
Michigan
Michigan Seeks Public Feedback on Behavioral Healthcare Access Ahead of PIHP Reprocurement. The Michigan Department of Health and Human Services (MDHHS) announced on February 28, 2025, that it is seeking public feedback to identify opportunities to improve behavioral healthcare services and supports provided by Pre-Paid Inpatient Health Plans (PIHPs) as the state moves toward reprocuring the PIHP contracts. The state invites current Medicaid enrollees and other stakeholders such as advocacy groups, providers, and federally recognized tribal governments to complete an online survey that will inform MDHHS on where it should focus their efforts. The survey is open until March 31, 2025.
Minnesota
Minnesota Appoints Shireen Gandhi as Temporary Commissioner of DHS. The Minnesota Department of Human Services (DHS) announced on February 28, 2025, that Shireen Gandhi has been appointed to serve as temporary commissioner of DHS, until a permanent commissioner is appointed. Gandhi joined DHS in 2017 and succeeds Jodi Harpstead.
Mississippi
Mississippi Medicaid Costs Rise to $8.1 Billion as Lawmakers Weigh Policy Changes. The Magnolia Tribune reported on March 4, 2025, that at a legislative hearing, Mississippi Medicaid Director Cindy Bradshaw warned lawmakers that the program’s budget has grown from $6 billion five years ago to $8.1 billion in 2025, with projections reaching $9.9 billion within five years. She cautioned that each percent reduction in federal funding could cost the state an additional $83 million annually. Lawmakers raised concerns over enrollment errors, delayed reimbursements, and the lack of pregnancy test requirements for presumptive eligibility.
Missouri
Missouri House Passes Bill to Cover Hearing Aids, Cochlear Implants for All Medicaid Members. The Salem News Online reported on March 3, 2025, that the Missouri House passed a bill, sponsored by Representative Cameron Parker (R-Campbell), expanding Medicaid coverage for hearing aids and cochlear implants to all eligible adults. Coverage is currently limited to children, pregnant women, and the blind, and expanding coverage will cost an estimated $10.6 million in the first year. A similar bill stalled in the Senate last year.
Montana
Montana Senate Approves Medicaid Expansion Renewal Bill with Work Requirements. The Associated Press reported on February 27, 2025, that the Montana Senate approved House Bill 245, which would renew Medicaid expansion and remove the Medicaid expansion sunset provision. The expansion also includes a work requirement that the state would need a federal waiver to put into action. The bill now moves to Governor Greg Gianforte for approval.
North Carolina
North Carolina Lawmakers Propose Bill to Increase Medicaid Dental Reimbursements. NC Health News reported on February 28, 2025, that North Carolina House Representative Brian Biggs (R-Trinity) introduced, along with other lawmakers, House Bill 60 to raise Medicaid dental reimbursement rates from 34 percent of charges to 46 percent, aiming to address the shortage of dentists accepting Medicaid patients. North Carolina’s Medicaid expansion, which launched in 2023, has covered $28.6 million in dental claims. The bill would require $52 million in state funds, matched by $95 million in federal contributions.
Ohio
Ohio Submits Section 1115 Demonstration to Add Work Requirements to Medicaid Expansion. The Ohio Department of Medicaid announced on February 28, 2025, that it has submitted a Section 1115 Group VIII Demonstration application to the Centers for Medicare & Medicaid Services (CMS), which would implement Medicaid work requirements for some expansion beneficiaries. If approved by CMS, beneficiaries would have to meet at least one of the requirements under the new demonstration, including being at least fifty-five years of age, employed, enrolled in school or an occupational training program, in a recovery program, or having intensive physical health care needs or serious mental illness. The application requests a January 1, 2026, start date.
Oregon
Oregon House Passes Bill to Extend Hospital, Insurer Taxes Through 2032 to Fund Medicaid. The Oregonian reported on February 27, 2025, that the Oregon House approved House Bill 2010, renewing taxes on hospitals and health insurers to secure $2.1 billion in funding for the state’s Medicaid program, Oregon Health Plan. The state’s hospital tax is set to expire in September, and the health insurance tax in 2026, but the bill would extend both through 2032. The bill now heads to the Senate for further consideration.
South Dakota
South Dakota Senate Advances Medicaid Expansion Funding 2026 Ballot Measure. South Dakota Searchlight reported on March 3, 2025, that the South Dakota Senate approved a 2026 ballot measure, House Joint Resolution 5001, sponsored by Representative Tony Venhuizen (R-Sioux Falls), the Lieutenant Governor of South Dakota, on whether to continue Medicaid expansion if federal funding drops below 90 percent. Medicaid expansion was passed by voters in 2022 and currently covers 30,000 residents. The measure does not require signature from the Governor.
Vermont
Vermont Medicaid Audits Show Opportunity to Improve Fraud Prevention, Health Outcome Evaluation. Vermont Biz reported on February 27, 2025, that two audits of the state Medicaid program, performed by Vermont State Auditor Doug Hoffer, showed that the state could improve its prevention of fraud, waste, and abuse, and also improve its evaluation of the Blueprint for Health program, a Patient-Centered Medical Home model that provides care coordination. The audit on the Department of Vermont Health Access’ (DVHA) Special Investigative Unit (SIU), found that SIU identified $1.2 million in improper payments, nearly $517,000 of which will not be recovered due to DVHA management decisions, and identified programmatic risks within DVHA. The audit recommends that DVHA work with SIU to address its recommendations more directly. The Blueprint audit found that the program has not had a sufficient evaluation of its effectiveness that is supported by evidence and lacks a strategic plan. The state auditor recommends Blueprint officials recommit to evaluating the effectiveness of the program.
National
CMS Rescinds Medicaid, CHIP HRSN Guidance. The Centers for Medicare & Medicaid Services (CMS) released on March 4, 2025, an informational bulletin rescinding Medicaid and CHIP guidance on health-related social needs (HRSN). The guidance includes Coverage of Services and Supports to Address Health-Related Social Needs in Medicaid and the Children’s Health Insurance Program, originally released on November 16, 2023, and the Coverage of Services and Supports to Address Health-Related Social Needs in Medicaid and the Children’s Health Insurance Program, released in December 2024. CMS will consider applications to cover HRSN services from states on a case-by-case basis.
HHS Announces Policy Narrowing Public Input on Policies. Modern Healthcare reported on February 28, 2025, that the Health and Human Services Department (HHS) is ending a 54-year-old transparency practice, reducing public notice and comments on federal healthcare policymaking by following only the minimum requirements of the Administrative Procedures Act of 1946. The department will no longer require public input on policies related to agency management, personnel, public property, loans, grants, benefits, or contracts. Although certain Medicare rules will still require public review, HHS will now decide case by case when public input is needed.
Special Needs Plan Enrollment Rises 10.1 Percent During 2025 Enrollment Period. Modern Healthcare reported on March 3, 2025, that Medicare Special Needs Plan (SNP) enrollment rose 10.1 percent in February 2025 to 7.3 million, compared to the previous year, exceeding expectations despite a slowing Medicare Advantage market. Dual Eligible Special Needs Plans D-SNPs, covering Medicare-Medicaid beneficiaries, now make up 83 percent of all SNP enrollments and remain the most profitable for insurers.
GOP Congress Members Consider Plan to Prevent States from Using Insurer, Provider Taxes for Medicaid Match Funds. Politico reported on February 28, 2025, that Republican lawmakers are considering preventing states from using provider and insurer taxes to raise money to cover their share of Medicaid funds. The proposal is gaining momentum as the House Energy and Commerce Committee looks for ways to reach the $880 billion federal savings necessitated by the budget resolution passed on February 25. House Speaker Mike Johnson (R-LA) said Congress would not impose federal spending caps based on state Medicaid enrollment or reduce the percentage of Medicaid spending the federal government will match to reach that goal. Without the taxes, states could face an estimated $612 billion budget shortfall over the next decade.
Federal Judge Temporarily Blocks Trump Administration Layoffs. Health Payer Specialist reported on February 28, 2025, that U.S. District Judge William Alsup has temporarily blocked the Trump administration’s order to fire thousands of probationary federal workers. The judge’s ruling said the order, which came from the Office of Personnel Management, was likely illegal, and that the office does not have the authority to direct other agencies to hire and fire employees. The U.S. Department of Health and Human Services expected to lose approximately 5,200 probationary employees, approximately a third of its workforce. An additional court hearing on the matter will take place March 13.
Medicaid Spending Cap Could Threaten Coverage for 15 Million Beneficiaries, KFF Finds. KFF released on February 26, 2025, an analysis which found that if Congress imposes a per capita cap on federal Medicaid spending, federal contributions could drop by $532 billion over 10 years, potentially forcing states to cut their own spending and eligibility—resulting in up to 15 million people losing coverage by 2034. According to KFF, if this cap is combined with eliminating the enhanced federal matching rate for Medicaid expansion, federal savings could rise even higher, ranging from $1 trillion to $2.1 trillion, and coverage losses could reach 30 million enrollees. This proposal is part of broader efforts by House Republicans to reduce Medicaid spending to help finance extended tax cuts.
Lawmakers Push for PBM Reform in House Subcommittee Hearing. Modern Healthcare reported on February 26, 2025, that the House Energy and Commerce Committee’s Health Subcommittee renewed efforts at a hearing to reinstate rules on pharmacy benefit managers (PBMs). Lawmakers are planning to reintroduce legislation that is designed to lower prescription drug prices by enhancing transparency, banning practices like spread pricing, and requiring PBMs to pass along negotiated discounts. This legislation is unlikely to be included in the government funding bill needed by March 14. However, some Representatives are seeking to bring the legislation directly to the floor for a vote.
Industry News
CVS Sells Medicare Shared Savings Program to Wellvana. CVS Health reported on March 4, 2025, that it has sold its Medicare shared savings program to Nashville, Tennessee-based Wellvana in an all-stock deal, retaining a minority stake in the firm. Wellvana manages care for 1 million Medicare members across 40 states. The financial terms of the deal were not disclosed.
CareSource to Acquire New York-Based Long-Term Care Plan. CareSource announced on March 4, 2025, that it is planning to acquire ElderServe Health for an undisclosed amount through a change-of-control transaction. ElderServe is a long-term care plan based in New York and serves approximately 20,000 older adults and adults with disabilities, primarily dual eligibles.
UnitedHealth Group Eases Prior Authorization for Medicare Advantage, Dual Special Needs Plans in 2025. Modern Healthcare reported on March 3, 2025, that UnitedHealth Group will cut nearly 10 percent of prior authorization requirements in 2025, starting April 1, as part of its ongoing effort to streamline approvals. The changes will remove pre-approval for home health services in Medicare Advantage and dual special needs plans across 36 states and Washington, D.C. Other insurers, including Cigna and Blue Cross Blue Shield, have also started rolling back prior authorization requirements.
Special Master Recommends Dismissal of DOJ Case Against UnitedHealth Over Medicare Advantage Payments. KFF Health News reported on March 4, 2025, that a special master ruled that the Justice Department did not provide sufficient evidence to support its claim that UnitedHealth received over $2 billion in Medicare Advantage overpayments. The recommendation to dismiss the case can be appealed. The DOJ alleged the insurer’s coding practices led to higher payments, while the ruling found the claims were speculative. The ruling comes as UnitedHealth faces an ongoing Senate investigation into its Medicare Advantage billing practices.
Health Plan Annual Reports Show Dialed-Back DEI, Publicity as Risk Factor. Modern Healthcare reported on March 3, 2025, that health plans’ 2024 annual reports, filed for investors with the Securities and Exchange Commission, show that insurers are dialing back or eliminating diversity, equity, and inclusion (DEI) policies to be more in line with President Donald Trump’s executive order banning DEI policies in the federal space and encouraging federal workers to discourage DEI policies in the private sector. The reports also show that payers are considering how negative publicity can be a risk factor for financial performance, as well as public safety for employees.
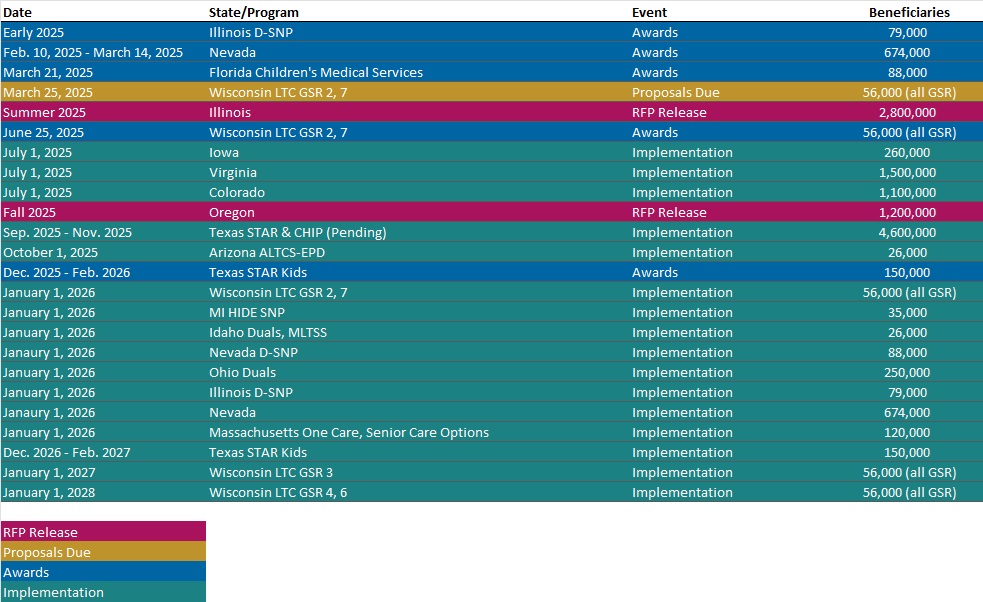
RFP Calendar
Company Announcements
MCG Press Release
MCG Releases 29th Edition of Care Guidelines with Updates for Observation Care and Cellular Therapy: Updates in MCG’s 29th edition of the nationally recognized guidelines were driven by recent regulatory changes in Medicare Advantage, new diagnoses with criteria for observation care, and growing evidence to support new cellular and gene therapies. Read More.
HMA News & Events
HMA Report
Analyzing the Impact of Policies to Exclude Certain Orphan Drugs from the Drug Price Negotiation Program of the Inflation Reduction Act. Rare Disease Day is observed globally each year on February 28 to raise awareness, access, and diagnosis to therapies for people with rare diseases. Today HMA releases a report titled Analyzing the Impact of Policies to Exclude Certain Orphan Drugs from the Drug Price Negotiation Program of the Inflation Reduction Act, that examines how many orphan drugs the ORPHAN Cures Act might affect and the percentage of Medicare Part B and Part D spending that is attributable to these drugs. Using that information, we estimated how the legislation would affect federal spending, applying the same assumptions and methodology that the Congressional Budget Office (CBO) uses in a 10-year budget score. Read More
Leavitt Partners, an HMA Company, Report
Kill the Clipboard: A Federal Policy and Industry Roadmap to Accelerate Innovation and Cut Administrative Waste. With the transition to a new administration, there is an opportunity to build on the work that has been done to date and accelerate our need to move to a more interoperable, patient-centered, digital health focused model of care. Now is the time to provide space for new innovations so we can help solve our most pressing health challenges and meaningfully advance health care data exchange across the country. Leavitt Partners digital health and interoperability leaders Ryan Howells and David Lee worked over the last few months with a group of leading payers, providers, consumers, digital health companies, national networks, and others on a set of specific recommendations the new administration and the industry can adopt to save billions of dollars in administrative costs, lower the burden on consumers and providers, and modernize our health care data exchange ecosystem. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES
(Exclusive Access for HMAIS Subscribers):
HMAIS Reports
- 2025 State of the State Addresses, Part 2: Evolving Healthcare Priorities Across the Nation
- Updated Medicaid Managed Care Rate Certifications Inventory
- Updated Federal Regulatory Tracker
- Updated HMA Federal Health Policy Snapshot
- Updated New York State Overview
Medicaid Data
Medicaid Enrollment and Financial data from Arizona, Colorado, Georgia, Maryland, and New York.
Public Documents:
Medicaid Rate Certifications, External Quality Reports, Spending Reports, Medicaid Advisory Committee Meeting Materials, Section 1115 Waivers, and other key documents from the following states: Delaware, Indiana, Minnesota, Ohio, Oklahoma, Tennessee, Texas, Vermont, West Virginia, and Wyoming.
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at amaresca@healthmanagement.com.