HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Michigan Releases Medicaid Managed Care RFP

- Alabama Releases Modular Electronic Visit Verification RFP

- California Submits Section 1115 Medicaid Waiver Amendment to Provide Rental Assistance

- Florida Legislators File Bills to Study Impact of Potential Medicaid Expansion on Individuals Aged 18 to 26

- Georgia Bidding Conference for Medicaid Managed Care Contracts Is Attended by Several Health Plans

- Georgia Democratic Leaders Call on Governor to Implement Full Medicaid Expansion

- Mississippi Medicaid Managed Care Procurement Stalls Following Protests from UnitedHealthcare, Elevance

- New Hampshire Providers to Receive Another Increase in Medicaid Payment Rates

- Pennsylvania Bill Would Reinstate Medicaid Coverage of Most Dental Services

- CMS Releases Final Rule to Increase Payments to ESRD Facilities by 2.1 Percent

- Bright Health Group, Friday Health Plans Owe $1.1 Billion in Exchange Risk-Adjustment Payments

In Focus
Michigan Releases Medicaid Managed Care RFP
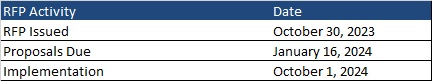
This week, our In Focus section reviews the Michigan Medicaid Managed Care Comprehensive Health Care Program (CHCP) request for proposals (RFP), which the Michigan Department of Health and Human Services released on October 30, 2023. CHCP covers 2.2 million Medicaid members and is worth approximately $15 billion.
MIHealthyLife
The rebid is part of MIHealthyLife, an initiative that the department launched in 2022 to strengthen Medicaid services through new Medicaid health plan contracts. At that time, Michigan Medicaid sought input from nearly 10,000 stakeholders in an effort to strengthen Medicaid managed care contracts and create a more equitable, coordinated, and person-centered system of care. Based on the feedback, the department designed the RFP with a focus on five strategic pillars:
• Serve the Whole Person, Coordinating Health and Health-Related Needs
• Give All Kids a Healthy Start
• Promote Health Equity and Reduce Racial and Ethnic Disparities
• Drive Innovation and Operational Excellence
• Engage Members, Families and Communities
RFP
Medicaid managed care organizations (MCOs) serve 10 regions, each consisting of multiple counties. MCOs will bid on one or more of the regions throughout the state. Each region requires at least two plans, with the exception of Region 1, a rural area that includes Michigan’s Upper Peninsula, where members are enrolled in a single plan.
As part of the MIHealthyLife initiative, the RFP will include the following changes:
• Prioritizing health equity by requiring Medicaid health plans to achieve National Committee for Quality Assurance Health Equity Accreditation
• Addressing social determinants of health through investment in and engagement with community-based organizations
• Increasing childhood immunization rates, including greater provider participation in the Vaccines for Children program
• Adopting a more person-centered approach to mental health coverage
• Ensuring access to health care providers by strengthening network requirements
• Increasing Medicaid Health Plan accountability and clarifying expectations to advance state priorities
Timeline
Proposals are due January 16, 2024, and implementation is anticipated to begin October 1, 2024. Contracts will run through September 30, 2029, with three one-year optional periods.
Current Market
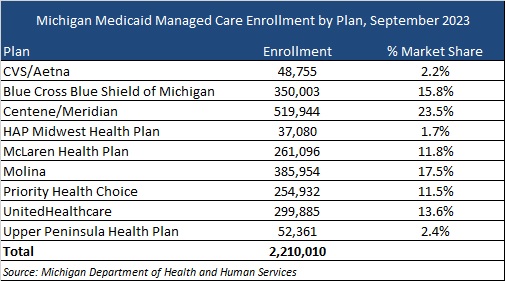
Michigan currently has nine plans, which serve more than 2.2 million Medicaid and expansion members. The table below provides a breakdown of the plan market share by enrollment.
HMA Roundup
Alabama
Alabama Releases Modular Electronic Visit Verification RFP. The Alabama Medicaid Agency released on October 25, 2023, a request for proposals (RFP) to reprocure a Modular Electronic Visit Verification vendor for home health and personal care services that require an in-home visit. The incumbent is HHAeXchange. Alabama will award one, two-year contract with three, two-year renewal options. Proposals are due December 27, and notification of intent to award will be announced February 28, 2024. The anticipated contract implementation date is July 1, 2024. Read More
California
California Submits Section 1115 Medicaid Waiver Amendment to Provide Rental Assistance. The Centers for Medicare & Medicaid Services (CMS) announced on October 20, 2023, that California has submitted for federal approval a Medicaid Section 1115 waiver amendment to provide up to six months of rental assistance for qualifying individuals who are homeless or at risk of homelessness. Public comments on amending the California Advancing and Innovating Medi-Cal (CalAIM) Section 1115 waiver are due by November 26, 2023. Read More
Florida
Florida Legislators File Bills to Study Impact of Potential Medicaid Expansion on Individuals Aged 18 to 26. Health News Florida reported on October 27, 2023, that Florida Representative Hillary Cassel (D-Dania Beach) and Senator Lori Berman (D-Boca Raton) filed separate bills that would require the Florida Agency for Health Care Administration to formally study the potential impact of Medicaid expansion on individuals aged 18 to 26. Specifically, the studies would assess the number of people who could obtain coverage, associated costs, and the use of expansion to address behavioral health needs. The Senate bill has been referred to the Health Policy, Appropriations on Health and Human Services, and Fiscal Policy committees. Read More
Florida Congressional Democrats Ask CMS to Monitor Their State’s Medicaid Eligibility Redeterminations Process. Florida Politics reported on October 30, 2023, that Florida Congressional Democrats asked the Centers for Medicare & Medicaid Services (CMS) to ensure their state follows proper protocols for Medicaid eligibility redeterminations. In a letter to CMS, lawmakers asked CMS to take action if it finds any unnecessary coverage losses. Florida has disenrolled over 730,000 beneficiaries since redeterminations resumed. Read More
Georgia
Georgia Bidding Conference for Medicaid Managed Care Contracts Is Attended by Several Health Plans. Health Payer Specialist reported on October 30, 2023, that Alliant HealthSolutions, AmeriHealth Caritas, CVS Health, Humana, Kaiser Permanente, Molina Healthcare, and UnitedHealth attended a bidding conference for Georgia’s recent request for proposals for the Georgia Families and Families 360° programs. Current incumbents Elevance, Centene, and CareSource also attended. Read More
Georgia Democratic Leaders Call on Governor to Implement Full Medicaid Expansion. Capitol Beat reported on October 25, 2023, that Georgia Democratic leaders are calling on Governor Brian Kemp to fully implement Medicaid expansion in Georgia, following slow enrollment in the state’s alternative expansion program Pathways to Coverage. The Pathways program includes work requirements and limits coverage to adults earning up to 100 percent of poverty. Read More
Kansas
Kansas Governor Calls For Medicaid Expansion Ahead of Legislative Session. KAKE reported on October 29, 2023, that Kansas Governor Laura Kelly will be making Medicaid expansion a top priority for the next legislative session. Polls show that about 70 to 80 percent of Kansans support expansion. Read More
Massachusetts
Massachusetts Submits MassHealth Section 1115 Amendment for Federal Approval. The Centers for Medicare & Medicaid Services announced on October 30, 2023, that Massachusetts submitted a waiver amendment to its MassHealth Medicaid and Children’s Health Insurance Plan Section 1115 Demonstration. The amendment seeks 12 months continuous eligibility for adults and 24 months continuous eligibility for individuals experiencing homelessness who are 65 and over; pre-release MassHealth services to individuals in certain public institutions; and expansion of Exchange subsidies. The waiver would also increase health-related social needs (HRSN) integration funding and expand HRSN services to include short-term post hospitalization housing and temporary housing for pregnant members and families, among other items. Public comments are open through November 20, 2023. Read More
Massachusetts Legislature Considers Medicaid Coverage of Doula Services. The Scope Boston reported on October 25, 2023, that Massachusetts lawmakers are considering legislation that would allow Medicaid coverage of doula services during pregnancy and up to 12 months postpartum. Another bill would standardize the doula certification process. The initiatives are aimed at addressing the high rate of serious birth complications among African-Americans in the state. Read More
Mississippi
Mississippi Medicaid Managed Care Procurement Stalls Following Protests from UnitedHealthcare, Elevance. Mississippi Today reported on October 27, 2023, that the Mississippi Medicaid managed care procurement remains stalled following protests from UnitedHealthcare and Elevance/Amerigroup. The two companies were not awarded contracts. The state has extended current contracts to June 2024. Read More
Montana
Montana Submits Section 1115 Medicaid Waiver Amendment to Cover Fertility Preservation Services. The Centers for Medicare & Medicaid Services (CMS) announced on October 26, 2023, that Montana submitted for federal approval a Medicaid waiver amendment to cover fertility preservation services for certain individuals with cancer ages 12 to 35. Public comments on amending the Montana Additional Services and Populations Section 1115 waiver are due by November 25, 2023. Read More
Nebraska
Nebraska Launches iServe Benefits Application Portal. The Star Herald reported on October 25, 2023, that Nebraska launched iServe Nebraska this month, providing a platform where individuals can use a single application for state benefits like Medicaid, childcare, food assistance, and other forms of economic assistance. Read More
New Hampshire
New Hampshire Providers to Receive Another Increase in Medicaid Payment Rates. The Portsmouth Herald reported on October 26, 2023, that several New Hampshire Medicaid providers will see another rate hike in January, on the heels of a three percent increase in July. The increases, part of a state budget allotment of $134 million (nearly $300 million including federal matching funds) for Medicaid rate hikes, will benefit home and community-based services providers, ambulance providers, children’s dental, and pregnancy care providers. Read More
New York
New York Announces $4 Million in Grant Funding for Mental Health Clinics. Crain’s New York Business reported on October 26, 2023, that the New York Office of Mental Health (OMH) will provide $4 million in grant funding to mental health clinics serving patients with serious needs in an effort to improve patient engagement, community-based efforts, and outreach to underserved populations. Licensed clinics can receive up to $49,500 each to support in-person or telehealth services. Grant applications are due by December 20. Read More
Oregon
Oregon Incorrectly Terminates Medicaid Coverage for 2,268 Beneficiaries. Oregon Public Broadcasting reported on October 27, 2023, that Oregon incorrectly disenrolled 2,268 Medicaid beneficiaries during September Medicaid eligibility redeterminations, including 619 children. Another 1,226 beneficiaries incorrectly received letters stating that their Medicaid coverage will be terminated at the end of October, and 11,700 people were wrongfully informed that they had coverage renewed through the end of the year. The state will send out new notices in November to all affected people. Read More
Pennsylvania
Pennsylvania Bill Would Reinstate Medicaid Coverage of Most Dental Services. WITF reported on October 26, 2023, that Pennsylvania Senator Jay Costa (D-Allegheny) sponsored a bill that would reinstate coverage of most types of Medicaid dental care. Pennsylvania eliminated the majority of Medicaid dental care coverage in 2011. Read More
Pennsylvania Long-term Care Facilities Await Funding, Face Staffing Shortages. WJAC Johnstown reported on October 31, 2023, that funding for Pennsylvania long-term care (LTC) facilities has been stalled pending passage of fiscal code legislative allowing budgeting funds to be distributed. The state legislature also passed a bill to address staffing shortages in LTC facilities, which will allow Certified Nurse Aids to train to become Certified Medication Aides. Read More
National
CMS Releases Final Rule to Increase Payments to ESRD Facilities by 2.1 Percent. The Centers for Medicare & Medicaid Services (CMS) issued on October 27, 2023, a final rule raising the end-stage renal disease (ESRD) prospective payment system base rate to $271.02, ultimately increasing total payments to ESRD facilities by approximately 2.1 percent. Additionally, the final rule will increase payments for certain new dialysis drugs. Read More
HRSA Requires 340B Registration for Offsite, Outpatient Hospital Facilities. Modern Healthcare reported on October 26, 2023, that several hospital offsite clinics are at risk of losing 340B drug discount program eligibility under a new policy implemented by the Health Resources and Services Administration (HRSA). Participating hospitals must now register offsite clinics with HRSA and list them on Medicare cost reports to qualify for 340B discounts, reversing a prior HRSA policy. Hospitals have 90 days to notify HRSA that they have started the process to comply with the new policy. Read More
Senators Introduce Medicaid Bill to Permanently Cover Medication-assisted Treatment for Substance Use Disorder. U.S. Senator Maggie Hassan (D-NH) announced on October 30, 2023, the introduction of a bill to permanently provide Medicaid coverage for medication-assisted treatment for substance use disorder. The bill, co-sponsored by Marsha Blackburn (R-TN), would permanently extend coverage currently made available through the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT Act), which expires in 2025. Read More
Biden Administration Releases Proposed Rule to Improve Surprise Billing Dispute Resolution Process. The Centers for Medicare & Medicaid Services (CMS) announced on October 27, 2023, that the Biden Administration released a proposed rule aimed at improving the No Surprises Act independent dispute resolution process. The rule would strengthen communications between payers and providers, encourage open negotiations, and make other administrative changes. Read More
Senators Introduce Bill Ensuring 12-Month Continuous Medicaid, CHIP Coverage. The Sidney Daily News reported on October 26, 2023, that U.S. Senators Sherrod Brown (D-OH), Tammy Baldwin (D-WI), Elizabeth Warren (D-MA), and Sheldon Whitehouse (D-RI) introduced a bill ensuring 12-month continuous eligibility to all individuals on Medicaid and the Children’s Health Insurance Program (CHIP). The Stabilize Medicaid and CHIP Coverage Act bill is aimed at preventing coverage losses as a result of short-term changes to beneficiary incomes. Read More
CMS Nursing Home Staffing Proposal Faces Lawmaker Opposition. Modern Healthcare reported on October 25, 2023, that Republican lawmakers voiced opposition during a House Energy and Commerce Health Subcommittee hearing on proposed rules that would raise pay for home health workers and institute staffing minimums at nursing homes. Democrats at the hearing supported the rules, which were proposed by the Centers for Medicare & Medicaid Services (CMS). Read More
MACPAC Meeting Is Scheduled for November 2-3. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on October 27, 2023, that its next meeting will be held on November 2-3. Among the topics for discussion will be Medicaid continuous coverage unwinding, including data-informed efforts and outreach strategies by states. Read More
HHS Proposes New Rule to Penalize EHR Information Blocking by Providers. Fierce Healthcare reported on October 30, 2023, that health care providers determined by the Office of Inspector General to have committed information blocking will no longer be considered as meeting “meaningful use” requirements for electronic health records (EHR), according to a proposed rule from the U.S. Department of Health and Human Services (HHS). The rule targets providers participating in existing Centers for Medicare & Medicaid Services programs. The public comment period will be open through January 2, 2024. Read More
Medicaid, CHIP Enrollment Falls in July 2023, CMS Reports. The Centers for Medicare & Medicaid Services (CMS) reported on October 31, 2023, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) was approximately 91.5 million in July 2023, a decrease of 1.1 million from June 2023. Medicare enrollment was 66.2 million, up 144,137 from June 2023, including 32.3 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. Read More
Industry News
Bright Health Group, Friday Health Plans Owe $1.1 Billion in Exchange Risk-Adjustment Payments. Modern Healthcare reported on October 27, 2023, that health insurers Bright Health Group and Friday Health Plans owe approximately $1.1 billion in Exchange risk-adjustment pool payments in several states. Friday Health alone owes $741 million in Colorado, Georgia, Nevada, New Mexico, North Carolina, Oklahoma and Texas. Read More
Molina Selects Executives to Lead Company’s Medicaid Business. Becker’s Payer Issues reported on October 26, 2023, that Molina Healthcare announced that Dave Reynolds and Debra Bacon would lead the company’s Medicaid business. Reynolds currently serves as executive vice president of regional health plans, while Bacon works as executive vice president of Medicare and marketplace. Read More
CMS Awards General Dynamics Information Technology $450 Million Contract to Continue Management of Financial Accounting System. General Dynamics Information Technology announced on October 26, 2023, that it was awarded a $450 million contract from the Centers for Medicare & Medicaid Services (CMS) to continue to operate and modernize the Healthcare Integrated General Ledger Accounting System, which organizes federal financial accounting for all CMS programs. The contract has an eight-month base period with seven optional years. Read More
RFP Calendar

HMA News & Events
Upcoming HMA Webinar:
Opportunities for State Regulators to Shape Policy and Regulation of Treatment for Substance Use Disorder. Thursday, November 2, 2023, 12 p.m. ET. Rescheduled from June 20, 2023. Health Management Associates (HMA) is offering a 3-part series of webinars looking at the effect of proposed regulations on delivery of opioid treatment services to the population facing addiction issues. In this third and final webinar, HMA consultants will highlight opportunities for state regulators to shape policy and regulation of SUD treatment. New federal regulations encourage significant changes to how opioid treatment is provided, with the goal of expanding access and improving patient-centered care. State regulators will need to adapt their regulatory practices and work closely with Medicaid agencies and treatment providers so the new regulations can achieve their intended goals. This webinar will discuss how State Opioid Treatment Authorities (SOTAs), licensing entities, and state Medicaid agencies will need to work together to craft updated regulations, facility licensing, and reimbursement practices that advance person-centered care.
Partnership in Action: A Collective Impact Approach to Implementing Workforce Solutions. Tuesday, November 7, 2023, 4 p.m. ET. The behavioral health workforce crisis is one of the most pressing challenges facing us today. The demand for mental health services has surged, yet the workforce shortage persists, resulting in unequal access to care and unmet demand. Communities and organizations throughout the country have identified challenges and devised innovative approaches to tackle the issue. Nonetheless, these strategies often lack coordination and dissemination, hindering their potential for widespread impact. Over the past two years, The College for Behavioral Health Leadership, The National Council for Mental Wellbeing, and Health Management Associates have been working together to develop a new approach to addressing the workforce crisis. This approach is built upon a collective impact framework designed to unify stakeholders across sectors, leveraging existing recommendations and innovative solutions to tackle the crisis.
Wakely, an HMA Company White Paper:
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arizona Medicaid Managed Care Enrollment is Down 10.2%, Sep-23 Data
- Florida Medicaid Managed Care Enrollment is Down 5.8%, Jun-23 Data
- Illinois Dual Demo Enrollment is Up 5.6%, Aug-23 Data
- Illinois Medicaid Managed Care Enrollment is Up 1.6%, Aug-23 Data
- Washington Medicaid Managed Care Enrollment is Down 6.4%, Jul-23 Data
- Washington Medicaid Managed Care Enrollment is Down 9.1%, Aug-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Alabama Modular Electronic Visit Verification RFP, Oct-23
- Michigan Comprehensive Health Care Program RFP, Oct-23
- New York Mental Health Outpatient Treatment and Rehabilitative Services (MHOTRS) Clinic Enhancement Grants RFA, Oct-23
- Oregon Medicaid Unwinding Policy Adaptation RFP, Oct-23
Medicaid Program Reports, Data, and Updates:
- California BH-CONNECT Section 1115 Waiver Documents, 2023
- California CalAIM 1115 Waiver and Related Documents, 2021-23
- Florida OIR Quarterly Managed Care Reports, 2020-23
- Hawaii Quest Integration 1115 Waiver Documents, 2018-23
- Massachusetts MassHealth Section 1115 Waiver Documents, 2021-23
- Montana Section 1115 Waiver for Additional Services and Populations (WASP) (Formerly Basic Medicaid Waiver) Documents, 2017-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio at [email protected].
