HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Texas Releases STAR+PLUS RFP

- Florida Reaches $484 Million Settlement with Pharmacy Chain Over Opioid Claims

- Georgia Enacts Bill to Implement 85 Percent Minimum MLR Requirement for Medicaid Plans

- BCBS-Illinois Appoints Stephen Harris as President

- Kansas Senate Approves Bill to Extend KanCare Contracts Through 2024

- Minnesota DHS Recommends Actions to Improve Racial Equity, Health Outcomes in Medicaid

- New Mexico HCBS Providers to Receive Temporary 15 Percent Reimbursement Rate Increase

- Oklahoma Names Traylor Rains State Medicaid Director

- Rhode Island Medicaid Managed Care Bid Is Rejected After Missing Submission Deadline

- Biden Proposes Fix to Exchange ‘Family Glitch’ Impacting 5 Million Individuals

- CMS Finalizes 8.5 Percent Rate Increase for Medicare Advantage, Part D Plans

- Intermountain Healthcare, SCL Health Complete Merger

- UnitedHealth/Optum to Acquire Majority Stake in Kelsey-Seybold Clinic

- Federal Judge Dismisses Anthem’s Claims in PBM Lawsuit Against Cigna

In Focus
Texas Releases STAR+PLUS RFP
This week, our In Focus section reviews the Texas STAR+PLUS managed care services request for proposals (RFP) released on March 31, 2022, by the Texas Health and Human Services Commission (HHSC). The STAR+PLUS program, including the STAR+PLUS Home and Community-based Services (HCBS) program, provides acute care services and Long-Term Services and Supports (LTSS) to the aged and disabled.
Background
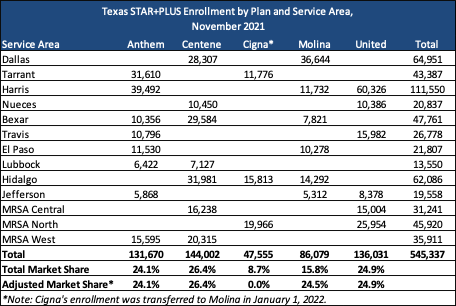
The STAR+PLUS program’s 540,000 beneficiaries are served by Anthem, Centene, Molina, and UnitedHealthcare. Cigna’s Texas STAR+PLUS Medicaid members (as well as the Medicare-Medicaid plan (MMP) members) were reassigned to Molina, effective January 1, 2022.
The STAR+PLUS program operates under a Section 1115 waiver and a Section 1915 waiver to expand the Medicaid managed care delivery system statewide and provide HCBS under a Medicaid managed care model.
The state threw out the previous awards for STAR+PLUS contracts in 2020 because of discrepancies in the evaluation and scoring of the bids. The STAR+PLUS contracts had been awarded to Aetna, Anthem/Amerigroup, Centene/Superior, El Paso Health, Molina, and UnitedHealthcare. Implementation was set to begin September 1, 2020. This marked the second time that year in which the procurement faced major setbacks because of problems with the procurement process.
Integration of acute care services and LTSS is an essential feature of STAR+PLUS. MCOs will also provide access to behavioral health services, such as mental health and substance use disorder counseling and treatment.
RFP
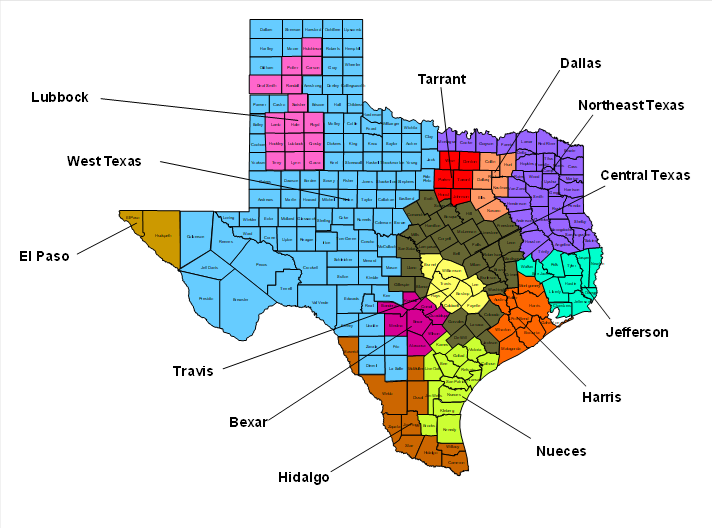
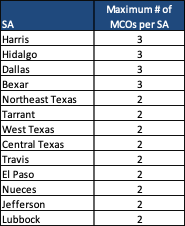
HHSC plans to award contracts to at least two managed care organizations (MCOs) in each of the state’s Service Areas (SAs). MCOs may bid on multiple SAs, and if chosen for an SA, must serve all counties within the SA. Contracts, worth a total of $10.3 billion per year, will run for six-years with three possible two-year renewal options.
There will be a maximum number of MCOs selected per SA as follows:
MCOs must also submit a notice of intent to apply for a Dual-Eligible Special Needs Plan contract to the Centers for Medicare & Medicaid Services by November 2022 or, if the Texas Medicare-Medicaid Dual Demonstration is continued beyond 2023, a notice of intent to apply for a Dual Eligibles Medicare-Medicaid Plan (MMP) contract.
HHSC will implement a voluntary pilot program in STAR+PLUS to test person-centered strategies and improvements for covering intellectual and developmental disabilities (IDD) waiver services under a capitated model. The new pilot program, STAR+PLUS Pilot Program (SP3) will carve LTSS into the STAR+PLUS program for people with IDD, traumatic brain injuries (TBI), acquired brain injuries (ABI) and similar functional needs in one of the service areas (either Bexar, Medicaid Rural Service Area Northeast or Tarrant). It will operate for two years beginning September 1, 2023, and will then be evaluated. Pilot Program participation will be limited to one or two STAR+PLUS MCOs.
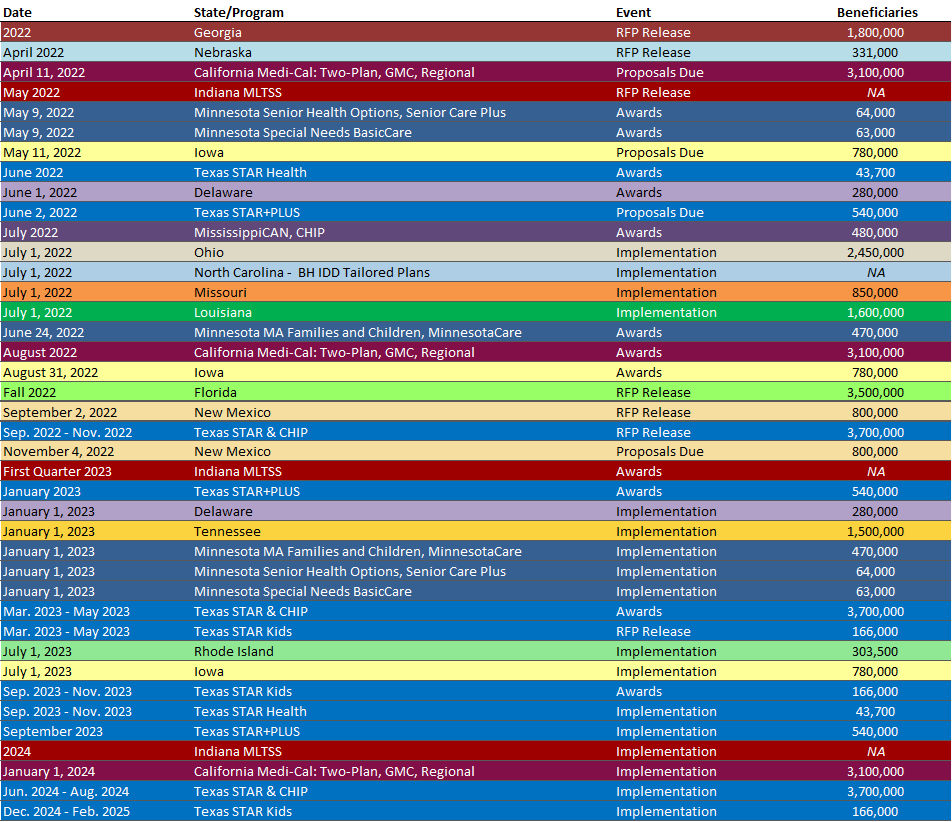
Timeline
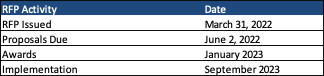
Proposals are due by June 2, 2022, and awards are expected in January 2023. Contract start date is September 2023.
Evaluation
Technical proposals will be scored based on the following criteria:
- Delivers person-centered service coordination that connects member needs to effective care.
- Demonstrates an understanding of the unique elements of service coordination and the needs of the STAR+PLUS population, inclusive of individuals with physical, behavioral health, and intellectual or developmental needs.
- Demonstrates an effective, person-centered process and infrastructure to identify, assess, and respond to individual member’s needs and strengths.
- Demonstrates engagement of providers, member’s family, and community supports serving the member in the service coordination process.
- Supports successful transitions of care for members between programs, services, and settings.
- Demonstrates how data will be used to inform service coordination approaches and to measure success.
- Ensure members have timely access to the services they need.
- Demonstrates the ability to deliver person-centered services timely in the least restrictive and most appropriate integrated setting for individuals covered in the STAR+PLUS Program.
- Demonstrates use of innovative and proven strategies to promote access to providers and services, including addressing provider shortages and barriers to care in specific areas of the state.
- Demonstrates the ability to coordinate and ensure the delivery of the full array of services across programs and payers to support members’ needs and preferences in a holistic way.
- Demonstrates provision of member services and supports that are culturally and linguistically appropriate, accessible, and responsive to the needs of members in the STAR+PLUS Program.
- Demonstrates a proactive approach to outreach and education to support members in successfully managing their health and directing their Services.
- Encourage providers to participate in the Medicaid program.
- Demonstrates effective collaboration and communication with the provider community as evidenced by network participation and provider satisfaction.
- Demonstrates proactive strategies to streamline processes and reduce administrative burden for providers.
- Demonstrates transparent, efficient policies and processes for key business operations, such as credentialing, contracting, claims payment, and utilization management (UM).
- Demonstrates support to providers in complex clinical decision-making through decision-support tools, best practice guidelines, and UM approaches.
- Utilizes network development strategies and incentives that ensure appropriate access for members.
- Demonstrates supports to providers serving the member using technology, data, and processes and tools to better inform and improve care across programs.
- Ensure a sustainable Medicaid program by incentivizing value in the service delivery model and optimizing resources.
- Demonstrates proven strategies to monitor and manage healthcare quality and improve key quality metrics that align with the goals of the state.
- Demonstrates a system of care that identifies, invests in, and rewards desired outcomes with regards to access, high-value care, and community integration.
- Demonstrates advances in value-based care and delivery system reform and supports Providers through these transitions with necessary data and information.
- Demonstrates achievable cost efficiencies and program integrity through effective monitoring and control of spending and UM trends.
- Use data, technology, and reporting to facilitate and demonstrate strong performance and oversight.
- Demonstrates capability to meet all requirements related to access to services, service delivery, quality of care, operations, and financial performance.
- Demonstrates consistent, timely, and accurate delivery of data, analysis, and reporting.
- Demonstrates process improvements and cost efficiencies using automation and data solutions.
- Utilizes integrated systems and processes with the state and other vendors to facilitate appropriate member transitions.
Link to RFP
HMA Roundup
Connecticut
Senate Committee Advances Bill to Raise Medicaid Income, Asset Limits for Individuals with Disabilities. The Connecticut Mirror reported on April 1, 2022, that the Connecticut Senate Human Services committee advanced a bill (Senate Bill 283) to raise the income limit for non-working individuals with disabilities to 138 percent of poverty. The bill would also raise the asset limits from the current levels of $1,600 for an individual and $2,400 for a couple to $5,000 for an individual and $7,500 for a couple. Read More
Connecticut Advocates Want to Offer Medicaid to More Undocumented Children. The Connecticut Mirror reported on March 31, 2022, that advocates are calling on Connecticut lawmakers to offer Medicaid to undocumented children under age 18, compared to a state law enacted last year to offer Medicaid to undocumented children under age eight effective 2023. Children must come from households earning up to 323 percent of poverty to be eligible. Read More
Connecticut Releases RFP for Non-Emergency Medical Transportation Services. The Connecticut Department of Social Services released on March 30, 2022, a request for proposals (RFP) for Medicaid and Covered Connecticut non-emergency medical transportation services. The contract will begin on October 1, 2022, and run for three years, with two one-year extension options. A mandatory letter of intent is due on April 8, and proposals are due on May 18. Read More
District of Columbia
District of Columbia Has Nation’s Highest Hospital Admission Rate, KFF Analysis Finds. Becker’s Hospital Review reported on March 29, 2022, that the District of Columbia has the highest hospital admission rate in the country at 166 admissions per 1,000, according to a Kaiser Family Foundation analysis of 1999-20 survey data. Alaska had the lowest at 51. The national rate was 95. Read More
Florida
Florida Reaches $484 Million Settlement with Pharmacy Chain Over Opioid Claims. Fierce Healthcare reported on March 30, 2022, that CVS Health has reached a settlement with the state of Florida over claims related to opioid prescriptions. CVS, which will pay $484 million over 18 years, will no longer be a defendant in the state’s opioid lawsuit to be tried in April. Read More
Georgia
Georgia Recovers More Than $85 Million in Medicaid Fraud Cases Since 2016. Valdosta Today reported on April 6, 2022, that Georgia Attorney General Chris Carr announced the state’s Medicaid Fraud Division has recovered more than $85 million since 2016. More than $68 million came from civil recoveries, while $17 million came in criminal restitution orders. Read More
Legislature Approves Bill to Extend Postpartum Medicaid Coverage from 6 Months to 1 Year. The Valdosta Daily Times reported on April 6, 2022, that the Georgia legislature approved a bill (Senate Bill 338) to extend postpartum Medicaid coverage from six months to one year. The cost of $28.2 million is included in Governor Brian Kemp’s proposed fiscal 2023 budget. The bill now goes to Kemp for his signature. Read More
Governor Signs Bill to Implement 85 Percent Minimum MLR Requirement for Medicaid Plans. Capitol Beat News Service reported on April 4, 2022, that Georgia Governor Brian Kemp signed a bill (House Bill 1013) to institute an 85 percent minimum medical loss ratio (MLR) requirement for Medicaid plans in the state and require health plans to cover mental health and substance use treatment at parity with physical health. The legislation is backed by $183 million in the fiscal 2023 state budget. Read More
Illinois
BCBS-Illinois Appoints Stephen Harris as President. Blue Cross Blue Shield of Illinois (BCBS-IL) announced on March 31, 2022, the appointment of Stephen Harris as president, replacing Steve Hamman, who has left the company to pursue other interests. Harris most recently led the Medicaid business of BCBS-IL parent company Health Care Service Corporation. He also served a stint at Molina Healthcare. Read More
Kansas
Senate Approves Bill to Extend KanCare Contracts Through 2024. The Topeka Capital-Journal reported on April 2, 2022, that the Kansas Senate approved a bill that would require the state to extend existing Kansas Medicaid managed care contracts through December 2024. The Kansas House had previously passed a similar provision as part of a budget bill, but the provision was removed when the budget bill passed the Senate. The contracts are set to expire at the end of 2023, and the state has been preparing to release a request for proposals in October 2022. An extension would mean the next procurement would occur after the gubernatorial election. Read More
Minnesota
Minnesota DHS Recommends Actions to Improve Racial Equity, Health Outcomes in Medicaid. The Minnesota Department of Human Services (DHS) recommended on April 5, 2022, several actions to improve racial equity and health outcomes in Medicaid, including easier enrollment and renewal processes, expanded access to culturally relevant care, and community engagement in setting Medicaid policy. The recommendations were included in a report titled Building Racial Equity into the Walls of Minnesota Medicaid: A Focus on U.S.-born Black Minnesotans. Read More
New Mexico
New Mexico HCBS Providers to Receive Temporary 15 Percent Reimbursement Rate Increase. The New Mexico Human Services Department (HSD) announced on March 31, 2022, a temporary 15 percent reimbursement rate increase for home and community-based services provided to individuals with disabilities and severe behavioral health needs from May 1, 2021, through June 30, 2022. The cost is $130 million, with the funds provided through the American Rescue Plan Act. Read More
New Mexico Extends Postpartum Medicaid Coverage from 60 Days to 12 Months. The New Mexico Human Services Department announced on March 30, 2022, that postpartum Medicaid coverage will be extended from 60 days to 12 months, effective April 1, 2022. The extended coverage will impact an estimated 17,000 New Mexicans. Read More
New York
Opioid Overdose Deaths Increased 44 Percent in 2020, Report Finds. The New York State Department of Health reported on April 4, 2022, that New York had 4,233 overdose deaths involving opioids in 2020, up 44 percent from 2019, according the state’s Quarterly County Opioid Report for April 2022. New York state programs aimed at addressing opioid overdoses, including New York Matters, the Local Health Department Initiative, and more than 900 registered opioid overdose prevention Programs. Read More
Mitchell Katz to Continue to Lead New York City Health+Hospitals. New York City Health+Hospitals announced on March 30, 2022, that Mitchell Katz was renominated and confirmed to continue serving as president and chief executive, a post he has held since 2017. Read More
New York City Council Proposes Increased Funding for Mental Health, Safety Net Hospitals. Crain’s New York Business reported on April 5, 2022, that the New York City Council proposed a preliminary fiscal 2023 budget, including $107.7 million for mental health services, an additional $45 million in Hospital Stabilization Funds for safety net facilities, and $250 million to establish five new health centers across the city. Read More
New York Medicaid Failed to Provide HCBS for Children’s Mental Health, Class Action Lawsuit Claims. Bloomberg Law reported on March 31, 2022, the New York State Medicaid program failed to provide required access to intensive mental and behavioral home and community-based services (HCBS), according to a lawsuit filed on behalf of two classes of Medicaid-eligible children by Disability Rights New York, Children’s Rights, the National Health Law Program, and Proskauer Rose LLP. The lawsuit claims New York is in violation of the Medicaid Act and the Americans with Disabilities Act. Read More
North Carolina
North Carolina Health Plan to Provide Housing Assistance to Youth Aging Out of Foster Care. The Winston-Salem Journal reported on March 28, 2022, that Blue Cross Blue Shield of North Carolina’s Healthy Blue Medicaid plan will provide housing assistance to youth aging out of foster care. The initiative, which will be offered in collaboration with Children’s Home Society of NC/SaySo, will provide funding for deposits, rental assistance, arrears, and essential furniture. There are an estimated 12,000 children in foster care in North Carolina, with more than 450 aging out every year. Read More
Oklahoma
Oklahoma Names Traylor Rains State Medicaid Director. The Journal Record reported on March 30, 2022, that the Oklahoma Health Care Authority named Traylor Rains as Medicaid director. Rains, who previously served as deputy Medicaid director, replaces Melody Anthony, who is retiring. Read More
Rhode Island
Rhode Island Medicaid Managed Care Bid Is Rejected After Missing Submission Deadline. Health Payer Specialist reported on March 30, 2022, that the Rhode Island Department of Administration rejected Point32Health’s Medicaid managed care bid because it missed the submission deadline. Point32Health, previously Tufts Health Plan before its merger with Harvard Pilgrim Health Care, provides Medicaid coverage to 17,000 individuals in Rhode Island or about five percent of the state’s Medicaid population. Blue Cross Blue Shield of Rhode Island, Molina Healthcare, UnitedHealthcare, and Neighborhood Health Plan of Rhode Island are the other bidders. Read More
Tennessee
Senator Pushes Back on Proposal to Offer D-SNP Contract to Plan After Failed Bid. The Tennessee Lookout reported on April 4, 2022, that Tennessee Senator Todd Gardenhire (R-Chattanooga) said he would be reluctant to offer Centene a dual-eligible special needs plan (D-SNP) contract after the company failed to win a bid during the last procurement process. The question arose after Gardenhire sponsored a separate bill touching on D-SNP enrollment. A House version of the bill would require the state to contract with a fourth managed care organization that failed to win in the most recent bidding. Read More
Tennessee Medicaid Medication Therapy Management Pilot Delivers Varied Results, Study Shows. The American Journal of Managed Care published a study on March 31, 2022, that found the Tennessee Medicaid medication therapy management pilot program delivered mixed results. The study found that the program did not demonstrate cost savings or across the board medication use from 2018-2020; however, it did result in fewer emergency department visits and increased medication adherence for chronic conditions like asthma, diabetes, and hypertension. Read More
National
HHS Releases RFI on Health Information Security. Modern Healthcare reported on April 5, 2022, that the U.S. Department of Health and Human Services released a request for information regarding ways to ensure the privacy and security of health information at healthcare organizations. Comments are due by June 6, 2022. Read More
Biden Proposes Fix to Exchange ‘Family Glitch’ Impacting 5 Million Individuals. President Biden announced on April 5, 2022, a proposed rule that would provide Exchange plan subsidies to family members of workers who are offered affordable self-only employer coverage but unaffordable family coverage. Under current regulations, employer-based health insurance is defined as “affordable” based solely on the employee’s coverage options and not the family’s. The so-called “family glitch” impacts about 5 million people, with nearly 1 million expected to see more affordable coverage under the rule change. Read More
CMS Finalizes 8.5 Percent Rate Increase for Medicare Advantage, Part D Plans. Fierce Healthcare reported on April 4, 2022, that the Centers for Medicare & Medicaid Services (CMS) finalized an 8.5 percent increase in rates for Medicare Advantage and Part D plans in 2023. The advance notice released by CMS in February had proposed a 7.98 percent increase. Read More
CMS, Medicaid Directors Release State Resources for End of PHE. The Centers for Medicare & Medicaid Services (CMS) released on April 4, 2022, tools developed with the National Association of Medicaid Directors and others to aid state Medicaid agencies in the return to pre-pandemic operations when the public health emergency (PHE) ends. The tools outline steps states can take to ensure fair eligibility hearings and provides a summary of best practices. Read More
MACPAC Virtual Meeting Scheduled for April 7-8. The Medicaid and CHIP Payment and Access Commission (MACPAC) will hold its next virtual public meeting April 7-8, 2022. Registration is available on the MACPAC website, and public comments will be accepted during the meeting. Recommendations and draft chapters will be discussed to include in MACPAC’s June report to Congress addressing:
- Access monitoring in Medicaid
- Medicaid’s role in advancing health equity
- Access to vaccines for adults enrolled in Medicaid
- Oversight of managed care directed payments
- Encouraging health IT adoption in behavioral health
Other topics to be covered include:
- a review of the Centers for Medicare & Medicaid Services Request for Information on access to care and coverage in Medicaid and the State Children’s Health Insurance Program;
- an updated analysis on the health effects of when people lose Medicaid coverage and whether they are able to get coverage in health insurance exchanges;
- an analysis of Medicaid managed care procurement practices across states; and
- a review of reports to Congress by the Secretary of the U.S. Department of Health and Human Services regarding managed care coverage of services in institutions for mental diseases and best practices for prescription drug monitoring programs. Read More
3.4 Million Exchange Members Would Lose Coverage Without Enhanced Premium Tax Credits, Study Says. Fierce Healthcare reported on April 1, 2022, that 3.4 million Exchange members would lose coverage if Congress does not extend enhanced premium tax credits beyond 2022, according to a report from the U.S. Office of the Assistant Secretary for Planning and Evaluation, which advises the Secretary of the U.S. Department of Health and Human Services. States are considering backup plans for outreach to members at risk of losing coverage. Read More
CMS Delays Deadline for Updated Access Monitoring Review Plans Submission. The Centers for Medicare & Medicaid Services (CMS) announced on March 31, 2022, it is delaying the requirement that state agencies submit updated Medicaid access monitoring review plans from October 1, 2022, to October 1, 2024. CMS cited the demands of the public health emergency on state Medicaid agencies in its decision. Read More
Access to Network Providers Varies Significantly Between Medicaid, State Exchange Plans, Study Says. Fierce Healthcare reported on March 31, 2022, that access to in-network providers varies significantly between Medicaid and Exchange plans, driven by differences in physician network standards, according to a Georgetown University study. The study also found that there are limited federal regulations to ensure access to primary health care and rural health clinics. Read More
GAO Calls on CMS to Assess Quality of Medicaid Telehealth Services. The U.S. Government Accountability Office (GAO) released a report on March 31, 2022, calling on federal regulators to collect and analyze information on the quality of Medicaid telehealth services, which expanded exponentially during the COVID-19 pandemic. The report says that 32.5 million services were delivered via telehealth to about 4.9 million Medicaid beneficiaries in five selected states from March 2020 through February 2021, compared with 2.1 million telehealth services delivered to about 455,000 beneficiaries in the 12 months prior to the pandemic. Read More
CMS to Provide $110 Million MFP Funds to Expand Access to HCBS. The Centers for Medicare & Medicaid Services (CMS) announced on March 31, 2022, that it will provide more than $110 million to expand access to home and community-based services (HCBS) through Medicaid’s Money Follows the Person (MFP) program. Individual awards of up to $5 million will be available for more than 20 states and territories not currently participating in MFP. Read More
CMS Proposes Permanent Cap on Annual Hospice Wage Index Adjustments. Modern Healthcare reported on March 30, 2022, that the Centers for Medicare & Medicaid Services (CMS) is looking to permanently cap annual hospice wage index adjustments so payments never decrease more than five percent from the prior year, according to a proposed rule. CMS also proposed a 2.7 percent increase in hospice payments for fiscal 2023, which would provide an additional $580 million in reimbursements. CMS will accept comments on the proposed rule until May 31. Read More
HHS Reduces Medicare Appeals Backlog by 88 Percent. Becker’s Hospital Review reported on March 31, 2022, that the U.S. Department of Health and Human Services (HHS) has reduced its Medicare appeals backlog by 88 percent. At the end of the first quarter of 2022, a total of 52,641 appeals remained pending at the Office of Medicare Hearings and Appeals. HHS is required to reduce its backlog as the result of a 2018 federal court ruling. Read More
Industry News
Intermountain Healthcare, SCL Health Complete Merger. Fierce Healthcare reported on April 5, 2022, that Salt Lake City, UT-based Intermountain Healthcare completed its merger with Colorado-based SCL Health, establishing a not-for-profit organization with 33 hospitals, 385 clinics, and a health plan serving 1 million members. Intermountain president and chief executive Marc Harrison will lead the new organization, which will continue to operate under the Intermountain Healthcare name. Mike Leavitt, co-chairman of HMA, has been named chairman of Intermountain, which now operates in Utah, Idaho, Nevada, Colorado, Montana, Wyoming, and Kansas. Read More
UnitedHealth to Pay $650 Million Breakup Fee if Acquisition of Change Healthcare Fails to Close. Health Payer Specialist reported on April 5, 2022, that UnitedHealth Group will pay a $650 million breakup fee if its proposed acquisition of Change Healthcare fails to be completed. United has also extended the time required to complete the $13 billion deal, which is opposed by antitrust regulators. Read More
Health Plan Foundation Awards $7 Million Grant to Address Health Disparities. Health Payer Specialist reported on April 4, 2022, that the Anthem Foundation awarded a $7 million grant over three years to Creating Healthier Communities, an organization that creates partnerships to address health inequities. The grant seeks to address high preterm birth rates among pregnant Black women in Indiana, Georgia, and Ohio. Read More
UnitedHealth/Optum to Acquire Majority Stake in Kelsey-Seybold Clinic. Health Payer Specialist reported on April 4, 2022, that UnitedHealth Group’s Optum division will acquire a majority stake in Kelsey-Seybold Clinic, a Texas-based provider with 30 clinics and more than 500 physicians. Kelsey-Seybold also operates a Medicare Advantage plan. Private equity firm TPG Capital owns a minority stake. Read More
Federal Judge Dismisses Anthem’s Claims in PBM Lawsuit Against Cigna. Health Payer Specialist reported on April 4, 2021, that a federal judge dismissed claims by Anthem that it was owed $14.8 billion in a lawsuit against Express Scripts, the pharmacy benefit management arm of Cigna. According to U.S. District Judge Edgardo Ramos, Express Scripts agreed to negotiate good faith drug pricing in a contract with Anthem, not guarantee competitive prices. Read More
Hospital Group Launches Health Equity Roadmap. Fierce Healthcare reported on March 31, 2022, that the American Hospital Association launched an interactive health equity roadmap for its members. The roadmap offers an equity transformation assessment, customized action plan, and virtual community of peers. Read More
Health Plan Foundation Announces $15 Million Investment in Health Equity. The Independence Blue Cross Foundation announced on March 30, 2022, a $15 million investment over five years to create the Institute for Health Equity as part of an effort to address policies and practices contributing to health disparities in the Philadelphia-area. The Institute will initially focus on digital health, cultural competence in medicine, and maternal health. Read More
AHN Acquires Majority Stake in TCM Home Health. The Pittsburgh Business Times reported on March 30, 2022, that AHN Healthcare@Home, an Allegheny Health Network subsidiary, acquired a 60 percent stake in TCM Home Health, serving Washington and Pennsylvania. Graham Health Care Group owns the remaining 40 percent. The acquisition closed on March 7. Read More
Amulet Capital Partners Invests in Lighthouse Behavioral Health Solutions. Amulet Capital Partners announced on March 30, 2022, an investment in Lighthouse Behavioral Health Solutions, an outpatient substance use disorder and mental health treatment facility network. Amulet is a middle-market private equity investment firm based in Greenwich, CT. Read More
Vistria Group Secures Majority Stake in Professional Health Care Network. The Vistria Group announced on March 30, 2022, a majority investment in Professional Health Care Network, an Arizona-based home health management solutions and care coordination provider serving more than 950,000 lives in the western U.S. Read More
RFP Calendar
HMA News & Events
CMS and State Discussions: HMA Finds Additional Stakeholder Engagement Needed to Support Medicaid PHE Unwinding. On April 4, 2022, CMS published two new resources addressing Medicaid’s Public Health Emergency (PHE) “unwinding” activities. Today’s post focuses on CMS’ summary of promising state practices for unwinding planning efforts. Read More
New this week on HMA Information Services (HMAIS):
Medicaid Data
- District of Columbia Medicaid Managed Care Enrollment is Flat, Jan-22 Data
- Hawaii Medicaid Managed Care Enrollment is Up 11.4%, Oct-21 Data
- Missouri Medicaid Managed Care Enrollment is Up 2.3%, Feb-22 Data
- New Jersey Medicaid Managed Care Enrollment is Up 1%, Feb-22 Data
- New Mexico Medicaid Managed Care Enrollment is Up 6%, Nov-21 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 0.8%, Jan-22 Data
- Tennessee Medicaid Managed Care Enrollment is Up 1%, Feb-22 Data
- Washington Medicaid Managed Care Enrollment is Up 0.9%, Feb-22 Data
- Wisconsin Medicaid Managed Care Enrollment is Up 9.4%, Oct-21 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Colorado Medicaid eConsult Program ITN, Apr-22
- Connecticut Non-Emergency Medical Transportation RFP, Mar-22
- Mississippi Pharmacy PDL, Supplemental Rebate, Rate Setting and Programmatic Review and Assessment of Core Components RFP and Related Documents, 2021-22
- Mississippi Support and Hosting of the Medicaid Eligibility System RFP, Apr-22
- Texas STAR+PLUS Managed Care RFP
- Virginia DMAS Program Integrity Provider Oversight RFI, Apr-22
- Washington Cascade Care Public Option Plans RFA, Proposals, Award, and Related Documents, 2020-22
Medicaid Program Reports, Data and Updates:
- Minnesota Building Racial Equity Into the Walls of Minnesota Medicaid Report, Feb-22
- Nebraska Division of Behavioral Health Strategic Plan, 2022-24
- New York DOH County Opioid Quarterly Report, Apr-22
- Ohio Joint Medicaid Oversight Committee Meeting Materials, 2017-22
- Ohio OBM Monthly Financial Reports, 2021
- Ohio OBM Monthly Financial Reports, 2022
- Oregon Medicaid Advisory Committee Meeting Materials, Feb-22
- Pennsylvania Maternal Mortality Review 2021 Report, Jan-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
