HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Advancing Health Equity and Integrated Care for Rural Dual Eligibles

- Georgia Children on Medicaid, CHIP Face Behavioral Health Access Barriers

- Medicaid Dental News: Kentucky, New Hampshire, Nevada

- North Carolina Says Hospitals Profited from Medicare, Despite Claims of Losses

- PBM News: Ohio, Puerto Rico, Centene

- OR Seeks $1.5 Billion Increase in Medicaid Funds for 2023-25 Biennial Budget

- Pennsylvania Lawmakers Consider Prior Authorization Legislation

- States Leverage Medicaid Managed Care to Improve Health Equity, KFF Finds

- Community Medicare Advantage Plans Are Leaders in Quality, ACHP Finds

In Focus
Advancing Health Equity and Integrated Care for Rural Dual Eligibles
This week, our In Focus section highlights the Health Affairs article, Advancing Health Equity and Integrated Care for Rural Dual Eligibles, authored by Ellen Breslin, Samantha Di Paola, Susan McGeehan, Rebecca Kellenberg, and Andrea Maresca, Health Management Associates.
A public health crisis is growing more acute in rural America, disproportionately impacting individuals with both Medicaid and Medicare (the “dually eligible”). The rural health crisis is a health equity concern that affects all rural residents, including dually eligible individuals. There are 47 to 60 million people residing in rural areas. Twenty-one percent of dually eligible individuals live in rural areas—that’s about 2.6 million people. Based on these numbers, the authors calculate that the dual eligible population residing in rural communities accounts for about 5 percent of the total rural population. Dually eligible individuals living in rural areas are at risk of falling through the cracks.
Dually eligible individuals lack access to adequate medical, behavioral health, home-and community-based services (HCBS) and other social services; those living in rural areas face even steeper challenges. Since dually eligible individuals are among the poorest of all individuals covered under Medicare, they are at significant risk of paying a steep rural mortality penalty.
With these challenges there are opportunities for innovation for the dually eligible population living in rural communities. The US can reverse the mortality-disparity rate trajectory. Public and private entities are interested in revitalizing rural America, confronting the rural health crisis, and harnessing the power of rural communities. Investment in the rural health care sector is essential given it is a major economic driver of rural communities.
HMA is creating a toolkit with actionable solutions to improve access to services and integrated care and health equity for individuals dually eligible for Medicare and Medicaid who live in rural areas across the country. This project is a follow-on project to a previous HMA project supported by Arnold Ventures. In 2021, HMA prepared a brief, Medicare-Medicaid Integration: Essential Elements for Integrated Care Programs for Dually Eligible Individuals, to increase and promote enrollment in integrated care programs (ICPs) meeting dually eligible individuals’ needs and preferences. Interviewees including dually eligible individuals helped HMA to identify “access to needed services in rural areas” as an essential element of ICPs. In response, HMA started a new project to create a toolkit with actionable strategies to improve access to needed services and improve integrated care opportunities, specific to dually eligible rural residents’ needs.
HMA designed the toolkit around four values: 1) rural health equity is an imperative for dually eligible individuals, 2) actionable solutions and innovations must come from the community, 3) there is no single pathway to integration, and 4) Medicare and Medicaid flexibilities are critical to inspiring innovations to advance health equity, access, and integration. The toolkit will provide actionable solutions for states with and without integrated care programs for dually eligible individuals to increase access to needed supports and services, care coordination, and integrated care programs. We expect that states and rural communities will use the toolkit as a foundation for mapping a holistic plan to advance access to care coordination and integrated programs for dually eligible individuals residing in rural communities. Other states may employ contractual tools listed in the toolkit to expand access to providers and new services; strengthen partnerships among entities serving the community such as community-based organizations, providers, and health plans; and increase community-wide accountability for meeting dually eligible individuals’ whole person-centered needs. The toolkit is scheduled for an early 2023 release.
HMA Roundup
Georgia
Georgia Children on Medicaid, CHIP Face Behavioral Health Access Barriers. The Atlanta Journal-Constitution reported on October 20, 2022, that Georgia children covered by Medicaid and the Children’s Health Insurance Program (PeachCare) face barriers to behavioral health care access, including low provider payments and shortages of safety-net beds. Read More
Kansas
Kansas Receives Federal Approval to Enhance Medicaid Hospital Assessment Program. Hays Post reported on October 20, 2022, that Kansas has received federal approval to enhance the state’s Medicaid hospital assessment program, which will bring in funds to support $341 million in Medicaid hospital reimbursement rates. The program is administered by the state’s Health Care Access Improvement Panel. Read More
Kentucky
Elevance Health Seeks Rehearing in Kentucky Medicaid Managed Care Contract Decision. Health Payer Specialist reported on October 24, 2022, that Elevance Health (formerly Anthem Blue Cross Blue Shield) has requested a rehearing of the recent decision by the Kentucky Court of Appeals to uphold the state’s 2020 selection of CVS Health/Aetna Better Health of Kentucky, Humana Health Plan, Centene/Wellcare Health Insurance of Kentucky, UnitedHealthcare, and Passport by Molina to serve as the state’s Medicaid managed care plans. Elevance was excluded from the award after being added as a sixth plan while the legal dispute was pending. Read More
Kentucky Extends Adult Medicaid Benefits to Include Dental, Vision, Hearing. The Associated Press reported on October 20, 2022, that Kentucky Governor Andy Beshear extended adult Medicaid benefits to include dental, vision, and hearing. Approximately 900,000 adults will be eligible for the new benefits, effective January 1, 2023. Total cost is $36 million annually, with the federal government covering 90 percent. Read More
Massachusetts
Massachusetts Recovers $71 Million in Medicaid Fraud Settlements. Massachusetts Attorney General Maura Healey announced on October 24, 2022, that the state recovered more than $71 million in the federal fiscal year ending September 30, 2022, through Medicaid fraud settlements with outpatient mental health providers, home health agencies, substance abuse treatment facilities, adult day health centers, skilled nursing facilities, and dental practices. Criminal charges were brought against certain providers and individuals for defrauding MassHealth, as well as for abuse, neglect, or financial exploitation of elders. Read More
Mississippi
Mississippi FFS Medicaid NEMT Services Have 3.5 Percent Utilization Rate. Y’all Politics reported on October 21, 2022, that about 3.5 percent of Mississippi Medicaid beneficiaries on average utilized non-emergency medical transportation (NEMT) monthly from February 2019 to February 2022, according to a report from the Mississippi Legislative PEER Committee. MTM has been the state’s fee-for-service (FFS) Medicaid NEMT broker since 2013. Read More
North Carolina
North Carolina Reports Hospitals Profited from Medicare, Despite Claims of Losses. Kaiser Health News reported on October 25, 2022, that North Carolina hospitals made $87 million in profits from Medicare in 2020, according to a report from the state treasurer’s office. The report adds that despite the profits, many hospitals have publicly claimed to be losing money on Medicare. Read More
New Hampshire
New Hampshire Dental Workforce Shortage Is Expected to Worsen With Extension of Coverage to Medicaid Adults. The Keene Sentinel reported on October 22, 2022, that New Hampshire dental offices are experiencing a workforce shortage, which is expected to increase when approximately 80,000 adult Medicaid beneficiaries become eligible for routine dental care on April 1, 2023. The state is working to determine Medicaid reimbursement rates for dentists. Currently, only 14 percent of dentists accept Medicaid patients. Read More
Nevada
Nevada Submits 1115 Waiver Application to Expand Medicaid Dental Coverage for Diabetic Adults. The Centers for Medicare & Medicaid Services announced on October 24, 2022, that Nevada submitted a Section 1115 waiver demonstration proposal to expand access to dental services for diabetic Medicaid enrollees over age 21. Choice of provider would be limited to participating federally qualified health centers. Public comments will be accepted through November 23, 2022. Read More
New York
New York Releases Health Care Facility Transformation Grants RFA. The New York State Department of Health (NYSDOH) released on October 20, 2022, a request for applications (RFA) for grants under the Statewide Health Care Facility Transformation Program IV for projects to improve population health, improve patient outcomes and experience, and transition to a value-based care model. The state has allocated $200 million in funding for these projects. Applications are due by December 29, 2022. Read More
Ohio
Ohio Implements Single Pharmacy Benefit Manager. The Columbus Dispatch reported on October 20, 2022, that Ohio implemented a single, statewide pharmacy benefit manager this month, with service provided by Gainwell Technologies. The contract is valued at $146 million over eight years and is expected to save the state at least $312 million over two. Read More
Oregon
Oregon Seeks $1.5 Billion Increase in Medicaid Funding for 2023-25 Biennial Budget. The Portland Business Journal reported on October 25, 2022, that the Oregon Health Authority (OHA) is seeking a $1.5 billion increase in Medicaid funding for the 2023-25 biennium budget. The additional funding will be used to cover 3.4 percent in cost growth for the state’s 15 coordinated care organizations, the Healthy Oregon program, and the loss of enhanced reimbursements during the pandemic. OHA is also requesting another $1.5 billion for additional programs, including efforts to eliminate health inequities and handle eligibility redeterminations. Read More
Pennsylvania
Pennsylvania Lawmakers Consider Prior Authorization Legislation. Becker’s Payer Issues reported on October 25, 2022, that the Pennsylvania House is considering legislation to establish prior authorization (PA) approval standards for both Medicaid and commercial insurance, including the creation of an electronic portal with PAs and accompanying paperwork. The bill was passed by the Senate in June 2022. Read More
Puerto Rico
Puerto Rico Selects Abarca to Serve as PBM for Medicaid Program. Abarca announced on October 20, 2022, it was selected to serve as the pharmacy benefit manager (PBM) for Vital (formerly Mi Salud), the Medicaid program for Puerto Rico. Abarca began its contract on May 1, 2022, instead of its scheduled implementation date of January 1, 2023, after Puerto Rico and the incumbent PBM failed to agree on a contract extension. Vital serves about 1.3 million Medicaid beneficiaries. Read More
National
Exchange Plan Enrollment Increases Among Black, Latino Individuals. The U.S. Department of Health and Human Services (HHS) announced on October 25, 2022, that the number of Black enrollees in Exchange plans increased by 49 percent between 2020 and 2022. In addition, Latino enrollment increased 53 percent, and American Indian and Alaska Native enrollment increased 6 percent. HHS attributed the rise to increased outreach and enhanced subsidies. Open enrollment for 2023 begins November 1. Read More
States Are Leveraging Medicaid Managed Care to Improve Health Equity, KFF Medicaid Directors Survey Finds. The Kaiser Family Foundation (KFF) reported on October 25, 2022, that about a quarter of states are offering financial incentives to Medicaid managed care plans for improving health equity. According to KFF’s annual Medicaid directors survey, more than two-thirds of states have implemented at least one strategy to address health equity. The survey also found that states are reporting far more Medicaid benefit expansions than cuts, continued high telehealth utilization, and strong financial positions heading into fiscal 2023. Read More
Medicaid Enrollment to Fall Slightly in Fiscal 2023, KFF Survey Projects. The Kaiser Family Foundation reported on October 25, 2022, that Medicaid enrollment is expected to decline by 0.4 percent in fiscal 2023, following the end of the public health emergency (PHE), according to a survey of state Medicaid agencies. Enrollment growth slowed to 8.4 percent in fiscal 2022, following an increase of 11.2 percent in fiscal 2021. Medicaid spending rose 12.5 percent in fiscal 2022 and is projected to grow 4.2 percent in fiscal 2023. Read More
CMS Imposes Stricter Oversight for Poor-Performing Nursing Facilities. The Centers for Medicare & Medicaid Services (CMS) announced on October 21, 2022, revisions to the Special Focus Facility (SFF) Program, which monitors whether poor performing nursing homes are improving. The changes will extend the performance monitoring period and make it harder for facilities to graduate from the program. It will also terminate funding for facilities that do not demonstrate improvements. Additionally, CMS is instituting stricter enforcement policies for facilities that do not comply with regulations. Read More
Lawmakers Seek Expanded Medicare Coverage of Substance Use Treatment. Fierce Healthcare reported on October 21, 2022, that federal lawmakers are requesting that the Centers for Medicare & Medicaid Services (CMS) expand Medicare coverage of substance use disorder (SUD) treatment, including expanded use of residential substance use treatment services. The lawmakers cited a 2022 study that found only 11 percent of the 1.7 million beneficiaries with SUD received treatment, largely due to a lack of motivation and financial barriers. Read More
MACPAC Meeting Scheduled for October 27, 28. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on October 21, 2022, that its next meeting will be held on October 27-28. Among the topics for discussion will be race and ethnicity data collection, monitoring the unwinding of the continuous coverage requirement in Medicaid once the public health emergency ends, and trends in Medicaid drug spending and rebates. Read More
White House Announces Plan to Expand Access to SUD Medication-Assisted Treatment for Pregnant Women. The New York Times reported on October 21, 2022, that the White House Office of National Drug Control Policy announced a plan to expand access to medication-assisted treatment (MAT) of substance use disorder (SUD) among pregnant women. The plan also includes programs to train judges to incorporate MAT into sentencing for pregnant women with SUD, to increase access to medication for veterans, and to train employees of the Indian Health Service to screen for opioid use disorder among women of childbearing age. Read More
CMS Releases Ex Parte Medicaid Renewal Requirements Slide Deck. The Centers for Medicare & Medicaid Services (CMS) released on October 20, 2022, a slide deck providing states with strategies to improve ex parte renewal processes to increase the rate of Medicaid eligibility redeterminations at the end of the public health emergency. Ex parte renewals refer to utilizing beneficiary information available to the state agency without requiring additional information from the individual. Read More
Nearly 334,000 Providers Left Healthcare Workforce in 2021, Report Finds. Modern Healthcare reported on October 20, 2022, that nearly 334,000 providers left the healthcare workforce in 2021, driven by burnout and concerns related to the pandemic, according to a report by Definitive Healthcare. About 117,000 were physicians, 53,000 were nurse practitioners, and nearly 23,000 were physician assistants. Read More
Community Medicare Advantage Plans Are Leaders in Quality, ACHP Analysis Finds. Fierce Healthcare reported on October 20, 2022, that one-third of all five-star Medicare Advantage (MA) plans were not-for-profit community health plans, according to an analysis by the Alliance for Community Health Plans (ACHP). Overall, the number of plans that offer drug coverage receiving four or more stars declined by 17 percentage points. Read More
DOJ Seeks Further Information on CVS Health’s Planned Acquisition of Signify Health. Modern Healthcare reported on October 20, 2022, that the U.S. Department of Justice (DOJ) is seeking additional information prior to approving CVS Health’s proposed $8 billion acquisition of Signify Health, a provider of home health risk assessments. CVS announced plans to acquire Signify in September 2022. Read More
MACPAC Releases Inventory of Evaluations of Integrated Care Programs for Dual Eligible Beneficiaries. The Medicaid and CHIP Payment and Access Commission (MACPAC) released in October 2022, an inventory of evaluations of integrated care programs for dual eligible beneficiaries, which consists of reviews and abstracts of studies that evaluate the impacts of various programs, including Program of All-Inclusive Care for the Elderly (PACE), Financial Alignment Initiative (FAI), and Medicare Advantage dual eligible special needs plans (D-SNPs). Read More
Value-Based Care Providers Fare Better Financially During Pandemic, CMMI Director Says. Fierce Healthcare reported on October 19, 2022, that providers participating in value-based care payment programs fared better financially than other providers during the pandemic and were “better able to withstand the precipitous drop in volume,” according to Center for Medicare and Medicaid Innovation (CMMI) director Liz Fowler. She noted, however, that persistent staffing shortages are preventing more investment in value-based care. Read More
Industry News
Humana to Offer Medicare Advantage Plans in RI, WY in 2023. Humana announced on October 25, 2022, it will offer Medicare Advantage (MA) plans in Rhode Island and Wyoming, as well as 140 new counties across 17 states in 2023. With these additions, Humana will offer MA plans in 91 percent of U.S. counties. Read More
Centene Awards PBM Contract to Cigna/Express Scripts. Centene announced on October 25, 2022, that it has awarded a $40 billion pharmacy benefits management (PBM) contract to Cigna/Express Scripts, which is set to begin in 2024. The move comes after Centene settled lawsuits with multiple states concerning its in-house PBM operations. Read More
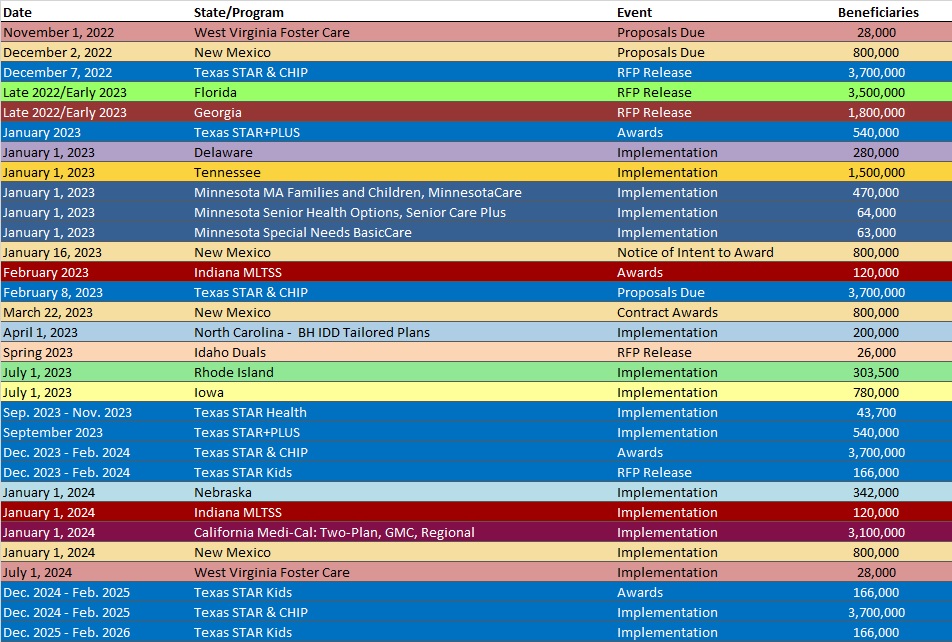
RFP Calendar
Company Announcements
HMA News & Events
WAKELY, AN HMA COMPANY, WHITE PAPERS
Inflation Reduction Act Review – Summary. The Inflation Reduction Act will have a substantial impact on pharmacy costs for Medicare managed care plans. To continue to be successful in the Medicare space, managed care plans will need to know how to optimize pharmacy strategies in this new environment. Read More
HMA WELCOMES
Caprice Knapp, Principal – Salt Lake City, UT
A health economist and evaluator, Caprice Knapp has more than 20 years’ experience working on Medicaid and the Children’s Health Insurance Program (CHIP) in the private sector, state and federal policymaking, and academics.
In the private sector she was the federal policy director for Molina Healthcare, Inc. As an academic, she was an associate professor in the Department of Health Outcomes and Policy at the University of Florida (UF) conducting external quality review activities for Texas and Florida Medicaid and CHIP programs and maternal and child health research. In the policymaking arena, she worked in the Governor’s Office of State Planning and Budgeting in Colorado as well as the U.S. House of Representatives Energy and Commerce Committee as a Robert Wood Johnson Health Policy fellow. Most recently she was the North Dakota Medicaid Director from 2019 to 2022.
Caprice’s career has been focused on vulnerable populations, delivery system reform, and global health. Examples of her funded research topics include an assessment of Florida’s CHIP Reauthorization Grant; an evaluation of fertility-preservation decision making for adolescent girls with cancer; outcomes of concurrent models of pediatric palliative care; and an assessment of the quality, patient experiences, and costs of health and dental plans for children in Florida. Her global health projects also focus on maternal and child health and have been conducted in Africa, Asia, Europe, and South America.
At the University of Florida, Caprice earned a PhD in economics and completed postdoctoral training in health services research. She has authored more than 80 peer-reviewed publications, 60 government reports, and two books.
Carl Mueller, Senior Consultant – Columbus, OH
Carl Mueller is an experienced data and policy analyst with a strong understanding of and interest in healthcare delivery systems, Medicaid, health reform, and value-based payment programs.
Prior to joining HMA, he served as an episodes data scientist on the Episodes of Care program in the Strategic Planning and Innovation team within the Division of TennCare. In this role, he led technical implementation and evaluation of the Episodes of Care program and served as the subject matter expert on all episodes of care content and methodologies. In addition to this role, he has experience on cost estimates and financial modeling, most recently showing the fiscal impact of the program.
Prior to TennCare, he served as a policy analyst at the Hilltop Institute at the University of Maryland, Baltimore County (UMBC). In this capacity, he provided technical assistance to the State Medicaid agency on the Affordable Care Act, helped estimate the financial impact of the Medicaid expansion for Maryland and New Mexico, assisted in annual evaluations of Maryland’s Medicaid program (HealthChoice), and co-wrote policy briefs as part of the Hospital Community Benefit Program.
Prior to Hilltop, he served as a summer research associate with the Congressional Research Service, within the Health Insurance and Financing Section. In this role, he provided support for member briefings, policy papers, memorandums, and section-by-section analyses of health reform legislation.
Carl earned his bachelor’s degree in management from the University of Texas at Arlington and master’s degree in management (health administration focus) from the University of Maryland, University College. He is pursuing his PhD in public administration from Tennessee State University.
Jennifer Hodgson, Principal – Columbus, OH
Jennifer Hodgson is a licensed marriage and family therapist who maintained a private practice and taught in higher education for 24 years prior to joining HMA. The scope of her experience in higher education training environments includes medical education, resident training and fellowship programs (i.e., family medicine, internal medicine, psychiatry), as well as family therapy and medical family therapy master’s and doctoral programs. She co-developed the first Medical Family Therapy doctoral program in the nation and served as major professor to 21 doctoral students during her tenure at East Carolina University.
During her tenure in higher education, she also developed a strong skillset in helping training programs prepare for, apply, and maintain their professional accreditation and certifications. She has expertise designing, innovating, and delivering integrated care in primary, secondary, and tertiary care contexts.
One of Jennifer’s longest consulting contracts (17 years) was focused on developing policies and workflows for sustaining an integrated care model for a multi-clinic Federally Qualified Health Center (FQHC) with a large Latino population. Additional consulting work includes helping programs apply for and maintain accreditation, designing curriculums for medical and mental health providers around workforce retention, delivering training on effective leadership and supervision approaches, facilitating interdisciplinary collaboration, and integrating behavioral health in primary (e.g., FQHC, training, and private), secondary, and tertiary care contexts.
Jennifer has helped healthcare and school-based systems strategically plan and launch integrated behavioral healthcare programs, as well as hospital-based systems in thinking about family engagement through patent portals using proxy access. A strength of her work includes knowing how to partner with higher educational institutions to develop a pipeline of future medical and behavioral health professionals that will work in these contexts upon graduation.
Her skillset in designing and implementing programs includes leading needs assessments and providing technical assistance to ensure quality and fidelity are maintained. This expertise includes her ability to train and develop quality metrics at the clinical, operational, financial, and educational levels, and conduct research to study lived experiences, outcomes, and inform program/service delivery improvements.
Jennifer has co-written and co-edited textbooks, book chapters, peer-reviewed articles, and other non-peer-reviewed works that focus on growing and training the behavioral health workforce and integrated care delivery systems. She has secured millions of dollars in grant funding at local and federal levels to help support her areas of work.
She completed her post-doctoral fellowship in medical family therapy at the University of Rochester and earned her Doctor of Philosophy in human development and family studies from Iowa State University. She received a Master of Science in applied family and child studies from Northern Illinois University and a Bachelor of Science in psychology from the University of Akron. In October 2022, she was awarded the Collaborative Family Healthcare Association’s “Family Oriented Care Award” for her commitment to ensuring our healthcare system is responsive to the needs of individuals and families.
Lida Riedlinger, Senior Consultant – Albany, NY
Lida Riedlinger uses her healthcare compliance, enterprise risk management, organizational development and leadership expertise to help organizations navigate the changing public health sector.
She is passionate about organization innovation and leadership development at all levels; cross functional workgroups, middle management and new supervisors, and provides executive coaching, strategic planning, and board development training in addition to consulting related to leadership transitions and succession planning. Executives and senior leaders gain clarity on their purpose, values, and business objectives to develop engaged accountable teams and improved performance.
Prior to joining HMA, Lida served as chief compliance officer for a multi-faceted Federally Qualified Health Center (FQHC) serving over 103,000 unique patients in western New York. In this role, she led the creation and implementation of a fully functioning healthcare compliance program that met federal Health Resources and Services Administration (HRSA), New York State Office of Medicaid Inspector General (OMIG) and New York State Department of Health (DOH) regulatory requirements. This work included development of a sub-recipient oversight and monitoring program for two area hospitals. Also, as part of this role she was responsible for the organizational and staff training in all matters of corporate compliance as required by New York State Office of Medicaid Inspector General (OMIG) related to fraud, waste and abuse which includes dissemination and attestation of the code of conduct and conflict of interest disclosure forms annually to all board members and staff. She was responsible for training strategy and curriculum content development that includes new staff orientation and annual mandatory risk management trainings that are relevant and meet all regulatory requirements.
Previously Lida worked as an independent consultant providing organizational consulting and executive coaching services for innovation, transformation, transition, and renewal. She also served as president and chief executive officer of Compeer Inc., which develops, delivers, and supports model programs that inspire and engage communities. This includes more than 4,000 volunteers serving people with mental health challenges by providing a trained supportive mentor from the community to help ease loneliness and isolation.
The National Institute of Mental Health selected Compeer as a model program in 1982 and funded the development of similar programs throughout the nation, Canada and Australia. Some of Lida’s key accomplishments while at Compeer were recruitment and development of an independent governing body that provides for strategy, governance and sustainability for the Compeer organization and the affiliated programs and constituent communities. This involved operational budget management of Compeer Inc., board level fund raising, relationship management with private foundations for fund development, and organizational strategic transition.
She was also instrumental in establishing Compeer on the Substance Abuse and Mental Health Services Administration (SAMSHA) National Registry of Evidence Based Programs and Practices for community based mental health programs. She facilitated strategic visioning and planning sessions for the Australian National Compeer Conference in Melbourne Australia in March 2012 and organized leadership participation in regional conferences of New York and Pennsylvania Compeer affiliates.
Lida is a fellow of the Northstar Network Healthcare Business Academy and certified in healthcare compliance through the Health Care Compliance Association (HCCA). She is certified in trauma informed care for primary care providers and community-based services through the Substance Abuse and Mental Health Services Administration (SAMHSA).
She earned her bachelor’s degree in communications design from the Rochester Institute of Technology.
Sharon Castro, Senior Consultant – Tallahassee, FL
Sharon Castro has over 20 years of experience in quality and accreditation and has been a National Committee for Quality Assurance (NCQA) surveyor since 2013.
Prior to joining HMA she worked as director for quality at various large managed care organizations such as Cigna, Kaiser Permanente, and Molina Healthcare. In this role she was responsible for regulatory and accreditation programs for commercial, Medicare, and Medicaid, including long-term services and supports and Marketplace lines of business.
Sharon has subject matter expertise in Centers for Medicare and Medicaid Services (CMS) requirements, NCQA standards and guidelines for health plan accreditation, health equity, utilization management, and credentialing among others, and state regulations. She has led the development and submission of the Centers for Medicare Special Needs Plans Model of Care achieving high scores.
She has successfully led organizations through other NCQA programs: Multicultural Healthcare Distinction and Patient Centered Medical Home (PCMH), Diabetes and Heart/Stroke recognition. As an NCQA surveyor she audits health plans, credentialing verification organizations and other types of organizations’ documentation and files against accreditation/certification/recognition requirements.
Sharon received a bachelor’s degree in information systems from the University of Phoenix, a master’s degree in project management from Colorado Technical University and a master’s degree in public health/health promotion and education from Walden University.
She is from the beautiful Caribbean island of Puerto Rico and enjoys going to the theater to watch musicals and traveling.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- California Medicaid Managed Care Enrollment is Up 7.3%, Jul-22 Data
- California Dual Demo Enrollment is Down 3.4%, Jul-22 Data
- Indiana Medicaid Managed Care Enrollment Is Up 5.6%, Jun-22 Data
- Indiana Medicaid Managed Care Enrollment Is Up 6%, Jul-22 Data
- Kansas Medicaid Managed Care Enrollment is Up 3.3%, Jun-22 Data
- Kansas Medicaid Managed Care Enrollment is Up 3.8%, Jul-22 Data
- Kansas Medicaid Managed Care Enrollment is Up 4.2%, Aug-22 Data
- Louisiana Medicaid Managed Care Enrollment is Up 3.6%, Jul-22 Data
- Michigan Medicaid Managed Care Enrollment is Up 1.8%, May-22 Data
- Michigan Dual Demo Enrollment is Down 1.9%, May-22 Data
- New Jersey Medicaid Managed Care Enrollment is Up 4.1%, Jul-22 Data
- New Mexico Medicaid Managed Care Enrollment is Up 1.6%, Jul-22 Data
- North Carolina Medicaid Managed Care Enrollment is Up 3.6%, Jul-22 Data
- Ohio Medicaid Managed Care Enrollment is Up 0.8%, May-22 Data
- Washington Medicaid Managed Care Enrollment is Up 3.1%, Jul-22 Data
- Wisconsin Medicaid Managed Care Enrollment is Up 3.6%, Jun-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Delaware HCBS for Individuals with Intellectual and Developmental Disabilities RFP, Oct-22
- Georgia Integration Platform Maintenance and Operations RFI, Oct-22
- Nebraska Heritage Health Medicaid Managed Care RFP, Awards, Scoring, Proposals, and Protest, Oct-22
- New York Statewide Health Care Facility Transformation Program RFA, Oct-22
Medicaid Program Reports, Data, and Updates:
- Maryland Medicaid HITECH Operational Advanced Planning Documents, FY2021-23
- Mississippi Report to Legislature on Medicaid FFS Non-Emergency Medical Transportation Services, Oct-22
- North Carolina Treasurers’ Office Report on Hospital Medicare Profits, Oct-22
- South Dakota Medicaid HITECH Implementation Advanced Planning Documents, 2011-21
- West Virginia Mountain Health Promise Foster Care Contract, SFY 2023
- West Virginia Mountain Health Promise Legislative Report, Jul-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
