HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Illinois Requests Section 1115 Waiver Extension to Respond to HRSNs and Eliminate Inequities

- Arkansas Is Urged by Healthcare Groups to Pause Medicaid Redeterminations

- Delaware Medicaid Expenses Are Projected to Increase Despite Redeterminations

- Florida Releases Medicaid Prepaid Dental Program RFI, To Release RFP Summer 2023

- Florida Releases D-SNP RFI, Considers Moving 300,000 Medicaid Members from D-SNPs to SMMC

- Illinois to Address Social Determinants of Health in 1115 Behavioral Health Waiver Amendments

- Indiana Enacts Legislation to Reform Long-term Care

- North Dakota Releases Medicaid Enterprise Technical Systems Integrator RFP

- Ohio Releases PACE Expansion RFP

- Virginia to Release Medicaid NEMT RFP in September 2023

- Virginia Disenrolls 20,000 Medicaid Beneficiaries During Redeterminations

- Federal Appeals Court Temporarily Blocks Overturning of ACA Preventive Services Requirement

- Wisconsin Approves Humana’s Proposed Purchase of Inclusa

- Sentara to Consolidate Medicaid Plans in Virginia

In Focus
Illinois Requests Section 1115 Waiver Extension to Respond to HRSNs and Eliminate Inequities
This week our In Focus section reviews the Illinois Healthcare Transformation 1115 Waiver Extension request, posted for review on May 12, 2023.
In pursuing this waiver extension, Illinois joins a growing list of states taking advantage of new Centers for Medicare & Medicaid Services (CMS) policy flexibilities to address health-related social needs (HRSNs) through Medicaid and test community-driven initiatives that are focused on improving health equity, improving access to care, and promoting whole-person care.
The Illinois waiver incorporates two of the most significant new opportunities in the CMS demonstration waiver flexibilities by proposing to incorporate housing supports for people who are experiencing or at risk of homelessness. The waiver also would extend community reintegration services for justice-involved adults and youths for up to 90 days before their release from incarceration. For a full list of proposed benefits and demonstrations, see Table 1.
Table 1. Summary of Illinois Medicaid 1115 Waiver Extension
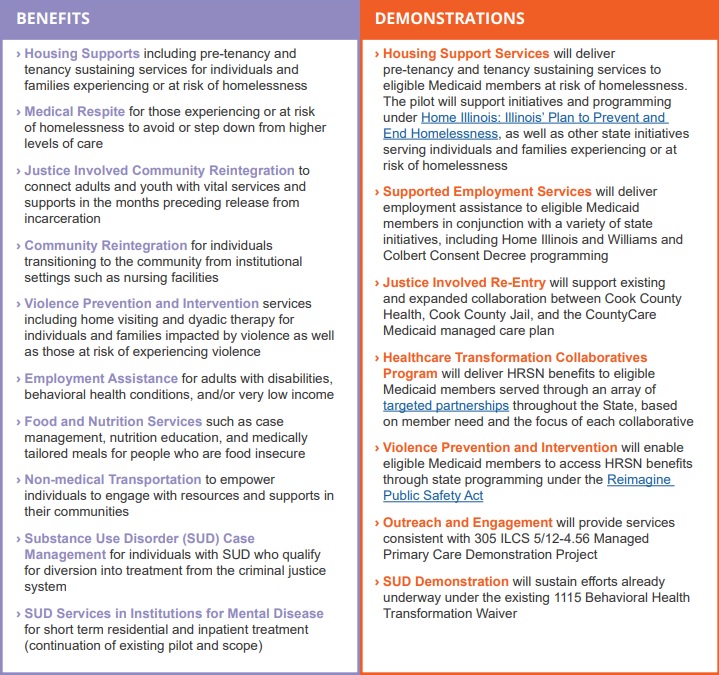
Source: Illinois Department of Health and Family Services. Illinois Healthcare Transformation Section 1115 Demonstration Extension Overview. Available at: https://hfs.illinois.gov/content/dam/soi/en/web/hfs/sitecollectiondocuments/1115demonstrationoverview05122023.pdf.
The Illinois waiver represents an unprecedented opportunity to demonstrate the long-term, positive impact of providing HRSN services to achieve health equity and create a sustainable, community-driven system for delivering those services. The demonstration proposes to offer a range of HRSN services that are focused on the unmet needs of people who are homeless and housing insecure, are justice-involved, have behavioral health conditions, are pregnant, are unemployed, are food insecure, and/or have been exposed to violence or are at risk of violence with the goal of eliminating health disparities.
The waiver projects a five-year total of $4.4 billion in HRSN services expenditures and another $800 million in HRSN-related infrastructure, indicating Illinois’ long-term commitment to healthcare transformation and to building an equitable, accessible, and high-quality delivery system.
For additional information, please email [email protected].
HMA Roundup
Arizona
Arizona Recovers $75 Million in Fraudulent Medicaid Payments. The Associated Press reported on May 17, 2023, that Arizona has recovered $75 million in fraudulent Medicaid payments, according to state Attorney General Kris Mayes. The payments involved billing for mental health treatment and addiction rehabilitation that was never provided. The state has also suspended Medicaid payments to more than 100 providers. Read More
Arkansas
Arkansas Is Urged by Healthcare Groups to Pause Medicaid Redeterminations. KUAR reported on May 15, 2023, that a coalition of 23 national healthcare groups have urged Arkansas Governor Sarah Huckabee Sanders to pause the state’s Medicaid eligibility redeterminations process. In its request, the coalition cited a high rate of procedural terminations of Medicaid eligibility. The state recently announced that almost 73,000 Medicaid beneficiaries have been disenrolled so far. Organizations in the coalition include the American Cancer Society, American Heart Association, American Lung Association, and March of Dimes. Read More
California
California Governor Proposes Re-imposing Tax on Managed Care Organizations. The Associated Press reported on May 12, 2023, that California Governor Gavin Newsom wants to re-impose a tax on managed care organizations, which would bring in additional revenues of $19.5 billion by 2026. The original tax expired in 2022. Newsom made the request in his fiscal 2024 budget proposal, which calls for further expansion of Medi-Cal eligibility and Medicaid provider payment increases. Read More
Connecticut
Connecticut Advocates Urge State to Extend Medicaid Coverage to Undocumented Individuals Up to Age 26. Connecticut Public Radio reported on May 10, 2023, that Connecticut healthcare providers and advocates are urging the state to extend Medicaid coverage to individuals up to age 26, regardless of immigration status. Currently, children up to age 12 can receive coverage. The state legislature is considering two separate bills, one that would raise the age to 15 and one to 18. Read More
Delaware
Delaware Medicaid Expenses Are Projected to Increase Despite Redeterminations. Delaware Public Media reported on May 15, 2023, that Medicaid expenditures in Delaware are projected to increase despite redeterminations, according to a budget forecast from the state’s Economic and Financial Advisory Council. The forecast expects enrollment of high-cost Medicaid beneficiaries to grow, while low utilizers will likely be the ones who lose coverage because of redeterminations. Read More
Florida
Florida Releases Medicaid Prepaid Dental Program RFI, To Release RFP Summer 2023. The Florida Agency for Health Care Administration released on May 15, 2023, a request for information (RFI) for the state’s statewide Medicaid prepaid dental program. Currently three plans — DentaQuest, Liberty, and MCNA Dental — serve the 4.8 million Medicaid members. The state is seeking information on improving integration, utilizing value-based payment designs, achieving cost savings, and implementing innovative delivery methods among other ideas and practices. Responses are due May 30. The request for proposals (RFP) is expected to be released summer 2023. Read More
Florida Releases D-SNP RFI, Considers Moving 300,000 Medicaid Members from D-SNPs to SMMC. The Florida Agency for Health Care Administration released on May 15, 2023, a request for information (RFI) for the state’s dual-eligible special needs plan (D-SNP) program. Currently, the state contracts with 27 D-SNPs covering 600,000 members. Of these members, half are eligible for full Medicaid benefits. Florida is considering moving the responsibility for providing Medicaid services from the D-SNP contracts to the Florida Statewide Medicaid Managed Care (SMMC) program. Enrollment into the SMMC program would be mandatory for the full benefit dual-eligibles. As a result, D-SNP contracts would become Coordination-Only D-SNPs and D-SNPs would no longer receive a capitation rate for their full dual members. Over 300,000 members would be shifted to the Medicaid managed care program. The RFI is seeking information on whether the state should continue with Highly Integrated and Fully Integrated D-SNP contracts or move to Coordination-Only contracts. Responses are due May 30. Read More
Florida Enacts Legislation to Track Undocumented Patients Receiving Care at Medicaid Funded Hospitals. Florida Politics reported on May 10, 2023, that Florida Governor Ron DeSantis signed a bill (Senate Bill 1718) that requires hospitals receiving Medicaid funding to ask patients if they are undocumented when they seek care and to submit the results quarterly. DeSantis has also said he will not take advantage of the recent federal rule that makes Deferred Action for Childhood Arrivals (DACA) recipients eligible for Medicaid and Exchange coverage. Read More
Illinois
Illinois Senate Committee Advances Bill to Prevent Generic Drug Price Gouging in Medicaid. Health News Illinois reported on May 17, 2023, that the Illinois Senate Health and Human Services Committee advanced a bill (House Bill 3957) that allows state agencies to notify the attorney general of potential price gouging of generic drugs covered by Medicaid. The attorney general’s office would then decide whether to investigate the manufacturer or wholesale drug distributer. Read More
Illinois to Address Social Determinants of Health in 1115 Behavioral Health Waiver Amendments. Health News Illinois reported on May 15, 2023, that Illinois Medicaid Administrator Kelly Cunningham is working to amend the state’s 1115 behavioral health waiver to include pilot programs to address social determinants of health, including food and nutrition programs, employment assistance, non-medical transportation, and community reintegration for individuals previously in carceral settings. The waiver was originally approved in 2018 with a focus on substance use disorder services. Public hearings will be held on May 19, 22, and 25. Read More
House Passes Bill to Create State-based Insurance Exchange. Health News Illinois reported on May 11, 2023, that the Illinois House passed a bill (House Bill 579) to create a state-based health insurance Exchange for the 2026 plan year. The bill now goes to the Senate for consideration. Read More
Indiana
Indiana Enacts Legislation to Reform Long-term Care. JD Supra reported on May 12, 2023, that Indiana Governor Eric Holcomb signed legislation (House Enrolled Act 1461) to reform long-term care by improving oversight of facility staffing and workforce. The legislation will require the state to conduct individual eligibility assessments to determine proper levels of care under the Medicaid aged and disabled waiver, allow facilities to increase the number of comprehensive care and Medicaid-certified beds, and develop a plan to expand and improve rural access to services. Read More
Maryland
Maryland Launches Public Awareness Campaign for Medicaid Redeterminations Process. WBOC reported on May 12, 2023, that Maryland launched a public awareness campaign concerning the Medicaid eligibility redeterminations process. The campaign includes social media, direct communications, and digital ads in multiple languages. Read More
Michigan
Michigan Legislature Considers Bills to Address Nursing Shortages in Hospitals. Modern Healthcare reported on May 11, 2023, that the Michigan legislature is considering bills aimed at reducing the nursing shortage through improvements in retainment and recruitment by requiring hospitals to meet nurse-to-patient staffing ratios and end mandatory overtime as a regular practice. The package of bills is backed by the Michigan Nurses Association. Read More
Governor Directs State Departments to Assist Medicaid Beneficiaries During Redeterminations. FOX 17 reported on May 11, 2023, that Michigan Governor Gretchen Whitmer signed an executive directive that requires all state departments to help Medicaid beneficiaries stay covered during eligibility redeterminations. The state will conduct outreach efforts to beneficiaries, create online resources, hire additional staff, and reach out to business owners to ensure employees are aware of coverage options. Read More
New Hampshire
New Hampshire Senate Committee Advances $119 Million to Increase Medicaid Provider Reimbursement Rates. The New Hampshire Bulletin reported on May 16, 2023, that the New Hampshire Senate Finance Committee advanced a budget that includes $119 million to increase Medicaid reimbursement rates for providers. A version approved by the House included $134 million. The budget will now go to a full Senate vote. Read More
Business Leaders Urge Legislature to Make Medicaid Expansion Permanent. WMUR reported on May 9, 2023, that New Hampshire business leaders are urging the state legislature to make Medicaid expansion permanent. Lawmakers are currently debating a reauthorization of the program. Read More
North Dakota
North Dakota Releases Medicaid Enterprise Technical Systems Integrator RFP. The North Dakota Department of Human Services released on May 15, 2023, a request for proposals (RFP) for a Medicaid Enterprise Technical Systems Integrator. The state is looking to modernize existing integration platforms, implement modern integration, and identify and access management capabilities. Responses are due on September 1, and awards will be announced the week of March 25, 2024. The contract is anticipated to begin on April 8, 2024. Read More
Ohio
Ohio Releases PACE Expansion RFP. The Ohio Department of Aging released on May 11, 2023, a request for proposals (RFP) for its Program of All-Inclusive Care for the Elderly (PACE) expansion to Franklin, Hamilton, Montgomery, Lorain, Lucas, and Summit counties. Proposals are due on July 19. The state’s current PACE site is in Cleveland and managed by McGregor PACE Center for Senior Independence. Read More
Oklahoma
Oklahoma Nursing Homes, Long-term Care Facilities Urge Lawmakers to Increase Medicaid Reimbursement Rates. The Oklahoman reported on May 11, 2023, that Oklahoma nursing homes and long-term care facilities are urging lawmakers to increase Medicaid reimbursement rates. These facilities will face a 20 percent reduction in funding after the COVID-19 emergency ends. Read More
Texas
Texas Proposes Use of Alternate Data Set to Reassess Uncompensated Care Pool. The Centers for Medicare & Medicaid Services announced on May 17, 2023, that Texas proposed a waiver amendment allowing it to use alternate data sets to reassess its uncompensated care pool. The state is requesting the change to address the potential impact of COVID-19 on data typically used. The federal comment period will be open until June 16. Read More
Virginia
Virginia to Release Medicaid NEMT RFP in September 2023. The Virginia Department of Medical Assistance Services announced on May 15, 2023, plans to release a request for proposals (RFP) for its Medicaid non-emergency medical transportation (NEMT) program on September 1, 2023. Read More
Virginia to Study Program that Pays Family Members to Care for Medicaid Beneficiaries with Disabilities. The Virginia Mercury reported on May 15, 2023, that the Virginia Department of Medical Assistance Services will study a Maryland waiver program that allows the state to pay family members who care for individuals with disabilities. Virginia began a similar program during COVID-19, but it is scheduled to end in fall 2023. Read More
Virginia Disenrolls 20,000 Medicaid Beneficiaries During Redeterminations. Virginia Mercury reported on May 11, 2023, that Virginia has disenrolled 20,000 Medicaid beneficiaries since redeterminations began in April. An estimated 300,000 beneficiaries could lose coverage once the process is finished. Read More
Wisconsin
Wisconsin County Recommends Using $500,000 in ARPA Funding to Help with Medicaid Redeterminations. Milwaukee Journal Sentinel reported on May 11, 2023, the Milwaukee County American Rescue Plan Act (ARPA) Task Force recommended allocating $500,000 in ARPA funding to help with the Medicaid redeterminations process. About 44 percent of the county’s population is covered by Medicaid, with an estimated 90,000 to lose coverage during redeterminations. Wisconsin will begin the process in June. Read More
National
U.S. Representatives Reintroduce Bill to Expand Access to Virtual Mental Health Care for Medicare Beneficiaries. Fierce Healthcare reported on May 16, 2023, that U.S. Representatives Doris Matsui (D-CA) and Bill Johnson (R-OH) reintroduced a bill to eliminate a requirement that doctors see Medicare beneficiaries in person within six months of a virtual visit for mental and behavioral health concerns. The bill is supported by the American Medical Association and the American Psychiatric Association. Read More
Federal Appeals Court Temporarily Blocks Overturning of ACA Preventive Services Requirement. The New York Times reported on May 15, 2023, that a federal appeals court temporarily blocked a decision overturning the Affordable Care Act (ACA) requirement that health plans cover certain preventive health services. Services will be available while the appeals process is ongoing. Read More
U.S. Senate Committee Advances Bill to Regulate PBMs. Modern Healthcare reported on May 11, 2023, that the U.S. Senate Health, Education, Labor, and Pensions Committee advanced a bill that would regulate pharmacy benefit managers (PBMs) by banning spread pricing and requiring PBMs to pass along drugmaker rebates. The bill would also require PBMs to disclose prices they pay to pharmaceutical companies for drugs, fees they pay pharmacists to fill prescriptions, and what they earn from drug company copayment assistance programs. Read More
U.S. Senate Committee Holds Hearing on High Prescription Drug Prices. Health Payer Specialist reported on May 10, 2023, that the U.S. Senate Health, Education, Labor and Pensions Committee held a hearing on high prescription drug prices with pharmaceutical companies and pharmacy benefit managers (PBMs). The PBMs that testified included Cigna/Express Scripts, UnitedHealth/Optum, and CVS Health. The pharmaceutical companies included Eli Lily, Sanofi, and Novo Nordisk. Read More
Industry News
Wisconsin Approves Humana’s Proposed Purchase of Inclusa. The Wisconsin State Journal reported on May 11, 2023, that Wisconsin has approved Humana’s proposed purchase of Inclusa, one of the state’s four Family Care Medicaid long-term services and supports plans. The state is also reviewing the planned purchase of My Choice Wisconsin, another Family Care plan, by Molina Healthcare. Read More
Sentara to Consolidate Medicaid Plans in Virginia. Sentara announced on May 10, 2023, that it will consolidate its Virginia Premier and Optima Health Medicaid plans into a single plan under the Optima Health name, effective July 1. The combined plan will serve nearly 750,000 Medicaid beneficiaries in Virginia. Read More
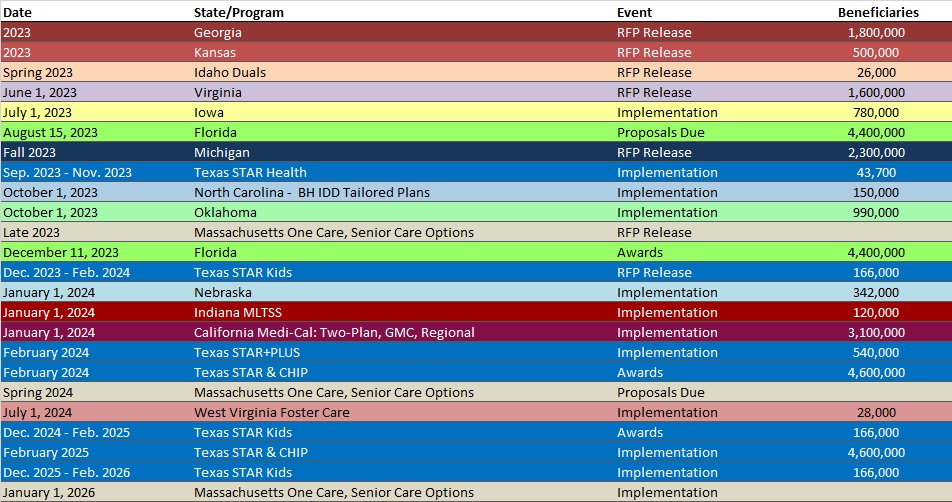
RFP Calendar
HMA News & Events
Upcoming HMA Webinar:
Using 1115 Justice Waivers to Improve Carceral Healthcare Delivery Information. HMA’s 4-part webinar series on 1115 Justice Waivers: Building Bridges of Health for Persons Leaving Carceral Settings, is designed to help plans and other stakeholders improve the long-term health outcomes of individuals. Part 2 will focus on the carceral settings operational healthcare practices, including intake screenings to aid in risk assignment and facilitate community re-entry. Thursday, May 18, 2023, 2 PM ET/11 AM PT. Click here to register.
Opportunities for Opioid Treatment Providers to Improve Patient Outcomes. HMA’s 3-part webinar series on New Rules in Treatment of Opioid Addiction is aimed at helping stakeholders prepare for new federal rules that will change how medications are delivered to persons with opioid use disorders. Part 1 addresses changes in clinical and business practices and payment structures that will enable providers to implement new treatment programs and other flexibilities to improve patient outcomes. Tues. May 23, 2023, 3pm ET. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arizona Medicaid Managed Care Enrollment is Up 1.4%, Mar-23 Data
- Illinois Medicaid Managed Care Enrollment is Up 1.3%, Apr-23 Data
- Illinois Dual Demo Enrollment is Down 3.8%, Apr-23 Data
- Missouri Medicaid Managed Care Enrollment is Up 6.3%, Apr-23 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 0.6%, Jan-23 Data
- Pennsylvania Medicaid Managed Care Enrollment is Up 1.1%, Feb-23 Data
- Puerto Rico Medicaid Managed Care Enrollment is Up 0.7%, Feb-23 Data
- Puerto Rico Medicaid Managed Care Enrollment is Up 0.6%, Mar-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Florida D-SNP RFI, May-23
- Florida Medicaid Prepaid Dental Program RFI, May-23
- North Dakota Medicaid Enterprise Systems Integrator RFP, May-23
- Ohio PACE Expansion RFP, May-23
Medicaid Program Reports, Data, and Updates:
- Mississippi Medicaid External Quality Review Reports, 2019-23
- New York Medicaid Pharmacy Managed Care to FFS Transition Presentations, 2020-23
- Oregon Health Care Payment Arrangements Report, 2021
- Oregon Prescription Drug Affordability Board Meeting Materials, Apr-23
- Pennsylvania MLTSS Subcommittee Meeting Materials, 2021-23
- Texas Plan for Unwinding Continuous Coverage and Enrollment Reports, May-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
