On September 15, 2020, the Centers for Medicare & Medicaid Services (CMS) released State Medicaid Director (SMD) letter #20-004 regarding value-based care (VBC) opportunities in Medicaid. [1] In the letter, CMS lays out a road map for state Medicaid agencies to adopt value-based payment (VBP). The SMD describes how states can use existing – or obtain new – authorities to adopt VBP. It lists examples of successful VBP designs in other states and identifies key enabling factors from its examination of lessons learned over the last ten years of investments in VBC activities.
The SMD reaffirms the framework maintained by the Health Care Payment Learning & Action Network (HCP-LAN) defining elements and categories of VBP. Figure 1 summarizes the HCP-LAN framework for categorizing VBPs.
CMS believes there is opportunity to expand VBP in Medicaid. Based on 2018 data reported by the HCP-LAN, CMS highlights that Medicaid participation in VBP greatly lags that of Medicare. In fact, CMS reports that while 90 percent of traditional Medicare payments were part of VBP arrangements in categories 2-4, only 32 percent of Medicaid payments were made under such arrangements in 2018.[2] 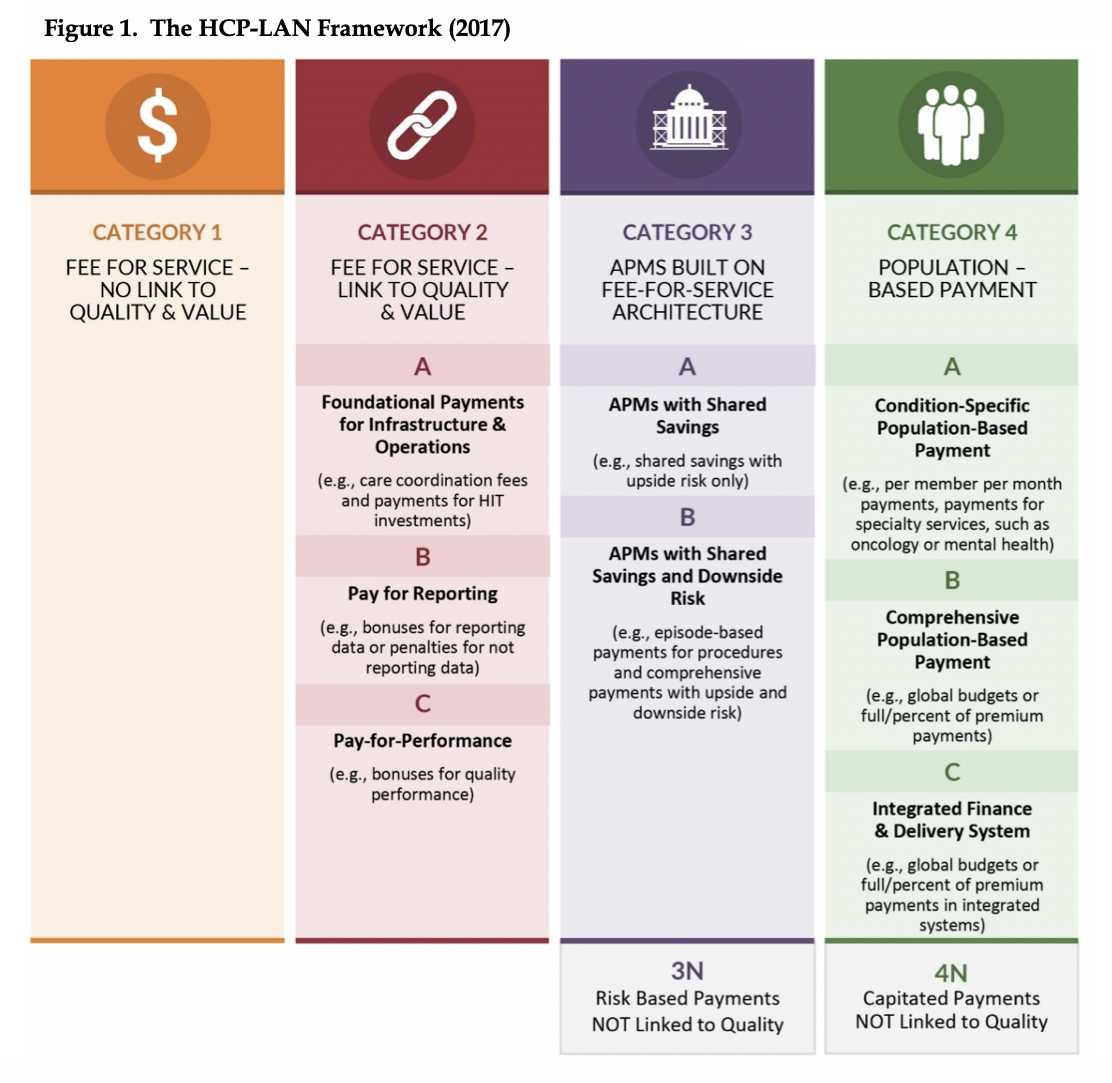
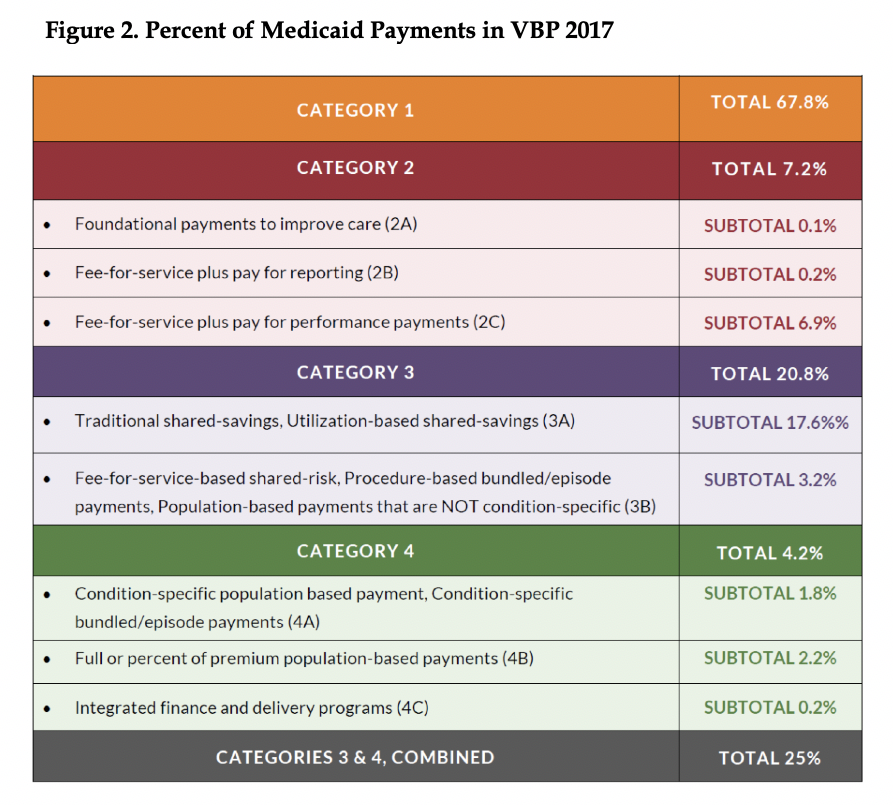
Figures 2 displays the percent of Medicaid payments in VBP arrangements in 2017, by HCP-LAN category. Figure 3 shows the percent of payments by payer in VBP arrangements in 2017, by HCP-LAN category.[3],[4]
Based on results of multiple evaluation and rapid cycle reports across the last ten years of innovation activities, CMS identifies the following factors as being important to success of VBP design and operations: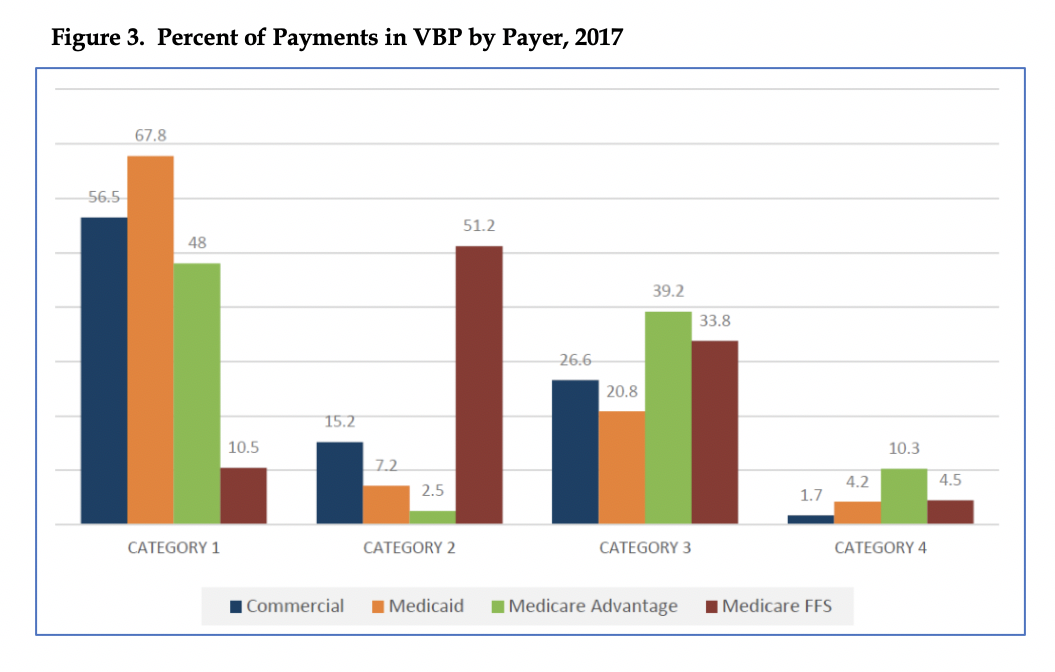

CMS goes on to say that states can facilitate shifts to VBP by:
- Participating in multi-payer efforts
- Conducting delivery system readiness reviews
- Supporting robust health information exchange and technology
- Seeking extensive stakeholder engagement
- Targeting quality measure selection
- Focusing on sustainability and continued aligned incentives
There are three payment strategies for state’s consideration described in Table 1 of the SMD letter (included for ease of reference below):
- Payment models built on a fee-for-service architecture
- Episodes of care payments
- Payments involving total cost of care accountability
HMA staff have extensive experience in the design and implementation of VBPs for State Medicaid Agencies and on behalf of Medicaid MCOs. In fact, HMA staff provided technical assistance in both the design and implementation of VBPs in the states highlighted in the SMD letter. HMA continues to support these states and managed care organizations in the monitoring of VBPs and creating roadmaps for movement along the continuum of VPB categories. If your state is interested in assessing its VBP opportunities, contact our expert VPB team for a consultation at [email protected].
Link: https://www.medicaid.gov/Federal-Policy-Guidance/Downloads/smd20004.pdf
[1] SMD #20-004. Re: Value-Based Care Opportunities in Medicaid. September 15, 2020. https://www.medicaid.gov/Federal-Policy-Guidance/Downloads/smd20004.pdf. Accessed September 19, 2020.
[2] Cited as in SMD#20-004: “These rates are calculated by summing HCP-LAN categories 2, 3, and 4 from the CY2018 payment results tables (p.18 and p.20) in the HCP-LAN 2019 Methodology and Results report.”
[3] APM Measurement. Progress of Alternative Payment Models. LAN Insights into APM Adoption. 2018. Health Care Payment Learning & Action Network (HCP-LAN). http://hcp-lan.org/workproducts/apm-discussion-2018.pdf. Accessed September 21, 2020.
[4] APM Measurement. Progress of Alternative Payment Models. 2019 Methodology and Results Report. 2019. Health Care Payment Learning & Action Network (HCP-LAN). http://hcp-lan.org/workproducts/apm-methodology-2019.pdf. Accessed September 21, 2020.