This week, our In Focus section reviews the Centers for Medicare & Medicaid Services (CMS) report to Congress on Non-emergency Medical Transportation (NEMT) in Medicaid, released June 20, 2023. CMS found that approximately 3 million to 4 million Medicaid beneficiaries used NEMT services annually between 2018 and 2021 and made recommendations related to Medicaid coverage of NEMT for medically necessary services.
Background
NEMT includes transportation services not limited to public transport, taxis, personal vehicle transport, non-emergency ambulances, air transport, and transportation network companies. Medicaid, unlike private insurers and Medicare, covers NEMT for any covered medical service for beneficiaries with an unmet transportation need. NEMT program administration varies from state to state and can be on a fee-for-service basis, carved out with third-party transportation brokers, or carved into the Medicaid risk-based managed care contracts. Under the Consolidated Appropriations Act, 2021, which made NEMT a statutory requirement, HHS must conduct and submit an analysis of nationwide Medicaid NEMT services to Congress. An initial report was submitted in June 2022.
Table 1. NEMT Service Delivery Models by State, 2018−2021
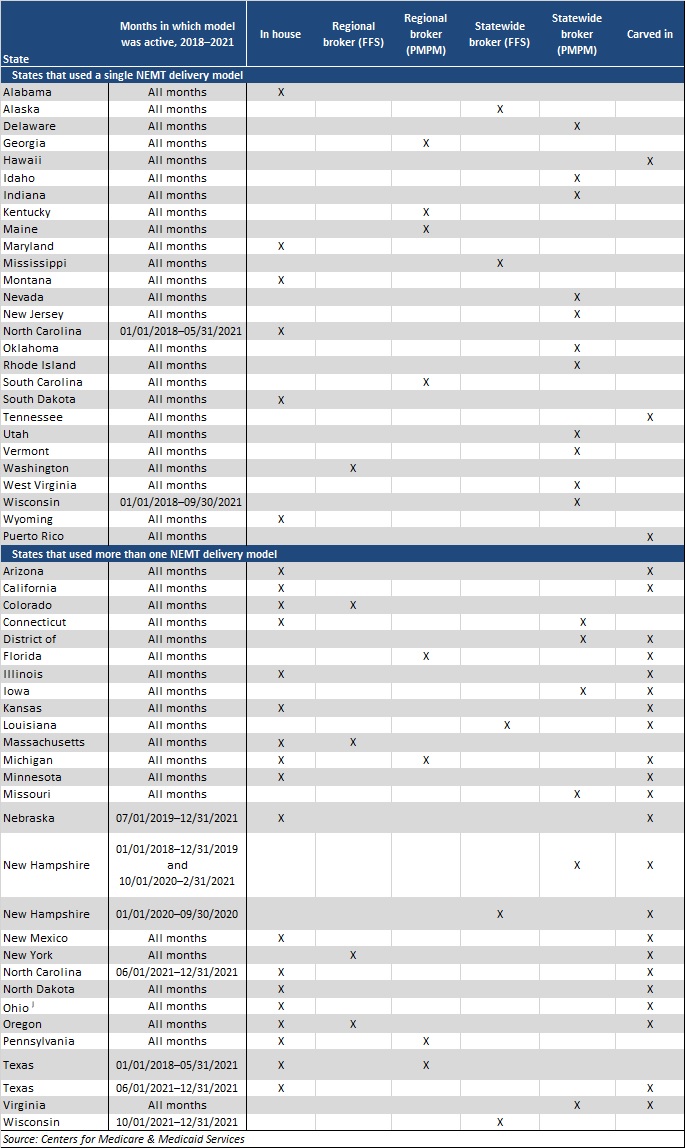
CMS conducted the analysis using Transformed Medicaid Statistical Information System (T-MSIS) data for calendar years 2018−2021. The analysis covered the number and percentage of Medicaid beneficiaries using NEMT, the average number of NEMT ride days, the types of medical services beneficiaries accessed when using NEMT, monthly trends in use of NEMT versus telehealth services before and during the COVID-19 public health emergency (PHE), and a comparison of the volume of NEMT services used by delivery model and state.
The T-MSIS data has some limitations and may not capture all Medicaid NEMT provided to beneficiaries due to differences in billing practices across states and providers. For example, if states claim certain medical service expenditures as administrative expenditures, T-MSIS will not capture it. Further, the number of ride days undercounts the total number of NEMT rides, as beneficiaries may receive multiple NEMT rides in a day. Because of these and other limitations, the data represents a subset of the NEMT that the Medicaid program covers.
Findings
Approximately 3−4 million Medicaid beneficiaries used NEMT annually in 2018−2021, representing 4−5 percent of Medicaid beneficiaries. Alaska, Minnesota, Arizona, Maine, and Wisconsin had the highest percentage of Medicaid beneficiaries who used NEMT, with up to nearly 11 percent in Alaska in 2021.
States that used a capitated broker model to deliver NEMT saw the highest use of these services. However, on average, states that used in-house NEMT delivery model claimed a relatively high percentage of NEMT expenditures as administrative expenditures, and NEMT administrative expenditures generally are not captured in the T-MSIS data.
Figure 1. Number of NEMT Ride Days per 10,000 Beneficiaries, by Delivery Model and Beneficiary Subgroup, 2021
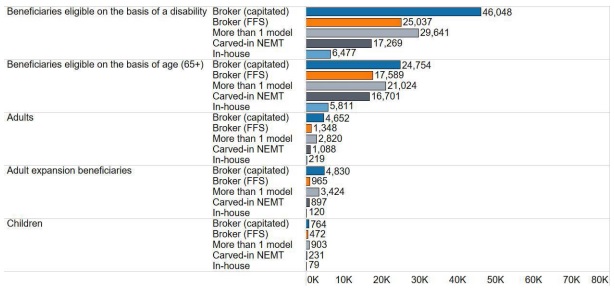
Medicaid enrollees with the highest NEMT usage rates included individuals in Money Follows the Person, receiving Section 1915c home- and community-based services, dually eligible for Medicare and Medicaid, and aging adults and people with disabilities. In addition, Medicaid members with certain physical and mental health conditions and those with a substance use disorder had higher rates of usage compared with the average Medicaid members. Medicaid enrollees in remote areas also used NEMT at the highest rates.
During the COVID-19 PHE, rates of NEMT dropped from 3.9 million beneficiaries, or 5 percent of all Medicaid members in 2019, to 3.5 million (4 percent) in 2020 and 3.3 million (4 percent) in 2021. In 2019−2020, the total number of annual NEMT ride days dropped by 37 percent, from 81.3 million to 53.1 million, but increased by more than 4 percent (to 55.5 million) in 2021. On average, the monthly number of NEMT ride days in 2021 remained about 30 percent below pre-PHE levels, and the number of beneficiaries using NEMT remained 23 percent below pre-PHE levels. The COVID-19 PHE caused telehealth to sharply increase. Throughout the PHE, telehealth was used more frequently than NEMT to access certain services.
Recommendations
CMS found that public transit was rarely used for NEMT, even though more than one-third of beneficiaries live in large, urban areas. In the report, CMS recommends that states should find opportunities to improve operations between NEMT and public transit networks to better coordinate services for beneficiaries.
CMS also recommends that states further examine the role of NEMT in improving the use of timely preventive care. Beneficiaries used NEMT to access preventive services at the highest rate of all service types examined. The analysis found some evidence that use of NEMT increases access to preventive services and is cost-effective, implying that increasing the uptake of NEMT may confer cost savings to states and the federal government.
Finally, CMS recommends that states increase awareness of the NEMT benefit. Medicaid beneficiaries’ knowledge of the benefit is low. CMS urges states to work with health plans and providers to share information with beneficiaries about the availability of NEMT.