This week our In Focus section reviews scenarios in which the federal Public Health Emergency (PHE) may expire. In the weeks ahead, the U.S. Secretary of Health and Human Services (HHS), Xavier Becerra, will be faced with the decision of whether to extend the PHE or to allow it to expire. Dozens of critical waivers and coverage flexibilities are currently linked to the federal PHE and have enabled patients, providers, and payors to receive, deliver, and pay for health care for nearly two years. To date, the PHE has been extended eight times, each for the maximum allowed 90 days. However, declining COVID-19 infection rates and actions by state governors to relax COVID-19-related public health measures have renewed pressure on the Biden Administration to signal how they will choose to act on April 16, 2022 when the current federal PHE expires.
We anticipate the Administration will extend the PHE beyond April 16th. However, one of a handful of scenarios may occur beyond April 16th. It is critical that stakeholders understand these scenarios and the implications of each. In this piece we focus on the overarching implications of these scenarios on the major Medicare, Medicaid and CHIP flexibilities. Patients, providers, and payors are all certain to feel the impact of these changes. In future documents we will consider specific policy issues in these programs.
Background: Pathways for federal flexibilities
The HHS Secretary first issued the COVID-19 PHE on January 31, 2020. Following that, on March 13, 2020, the President declared a national emergency for COVID-19. For over two years, the HHS Secretary and the President have continued to renew these declarations. Based on these actions, policymakers at the Centers for Medicare & Medicaid Services (CMS) and Congress have created flexibilities for patients and providers during the COVID-19 pandemic through one of three pathways. The expiration of the PHE will interact with the three pathways differently.
- Public Health Emergency Authority: HHS’ primary emergency authority is provided by declaring a public health emergency under section 319 of the Public Health Services Act. PHEs are authorized for up to 90 days and can be renewed in 90-day increments.[1] Through a series of interim final rules, CMS has provided numerous flexibilities, most of which will expire once the PHE ends.[2] Among these flexibilities are broader opportunities to utilize virtual care services, modified rules for Medicaid health home programs, and modifications to the calculations for Medicare Part C and D reimbursement.
- Section 1135 Authority: Section 1135 of the Social Security Act provides the HHS Secretary with specific emergency authorities, including the ability to waive or delay requirements for federal health insurance programs. Two conditions are required for the HHS Secretary to utilize Section 1135 waiver authority:
- The Secretary of HHS must have declared a PHE, and
- The President must have declared a national emergency under the National Emergencies Act (NEA) or the Stafford Act.
When both of these declarations are in place, as they have been during the COVID-19 pandemic, the Secretary may temporarily waive or modify certain Medicare, Medicaid, and Children’s Health Insurance Program (CHIP) requirements to ensure Medicare and Medicaid enrollees have sufficient access to health care items and services and to ensure providers who give such services in good faith can be reimbursed and exempted from sanctions (absent any determination of fraud or abuse).[3]
During the COVID-19 pandemic, CMS has used Sec. 1135 waiver authority extensively to issue blanket Medicare waivers and state-specific Medicaid waivers.[4] These waivers automatically expire when one or both of the emergency declarations expires. For example, under one current Section 1135 blanket waiver, providers are permitted to conduct certain health care services using audio-only communication technology and a broader array of health care providers are permitted to deliver telehealth services from a distant site.
- Statutory Authority. Congress passed several COVID-19 related bills providing flexibilities as well as funding to manage the emergency. Many of these flexibilities are linked directly to the timeline of the PHE. For example, the Families First Coronavirus Response Act (FFCRA) provides coverage under Medicare (traditional and Medicare Advantage) for COVID-19 testing and waives beneficiary cost sharing.[5] The FFCRA also increased the Medicaid matching rate (Federal Medical Assistance Percentage or FMAP) through the end of the quarter in which the PHE expires. In addition, the maintenance of Medicaid eligibility is required through the month in which the PHE expires.
PHE Scenario Planning
After more than two years living with COVID-19 and the related flexibilities, declining rates of infection and hospitalization have shifted policy debate towards identifying how and when to end the PHE and unwind the COVID-19 flexibilities. Secretary Becerra’s most recent federal PHE will expire on April 16, 2022. In addition, the Secretary has stated on multiple occasions that “when a decision is made to terminate the declaration or let it expire, HHS will provide states with 60 days’ notice prior to termination.”[6],[7] Given that the Secretary’s 60-day window prior to April 16, 2022, has passed, we anticipate the Secretary will extend the federal PHE beyond April 16, 2022. However, several potential scenarios may occur after April 16, and stakeholders should be prepared for each.
In making their decision about when to end the PHE HHS and CMS must consider the sensitivities and logistical issues involved in ending the COVID-19 waivers and flexibilities. This includes consideration for:
- minimizing disruptions in access to coverage and services for patients
- allowing for appropriate unwinding of processes implemented by providers and payers
- ensuring the ongoing sufficiency of reimbursement and coverage policies afforded to providers and payers
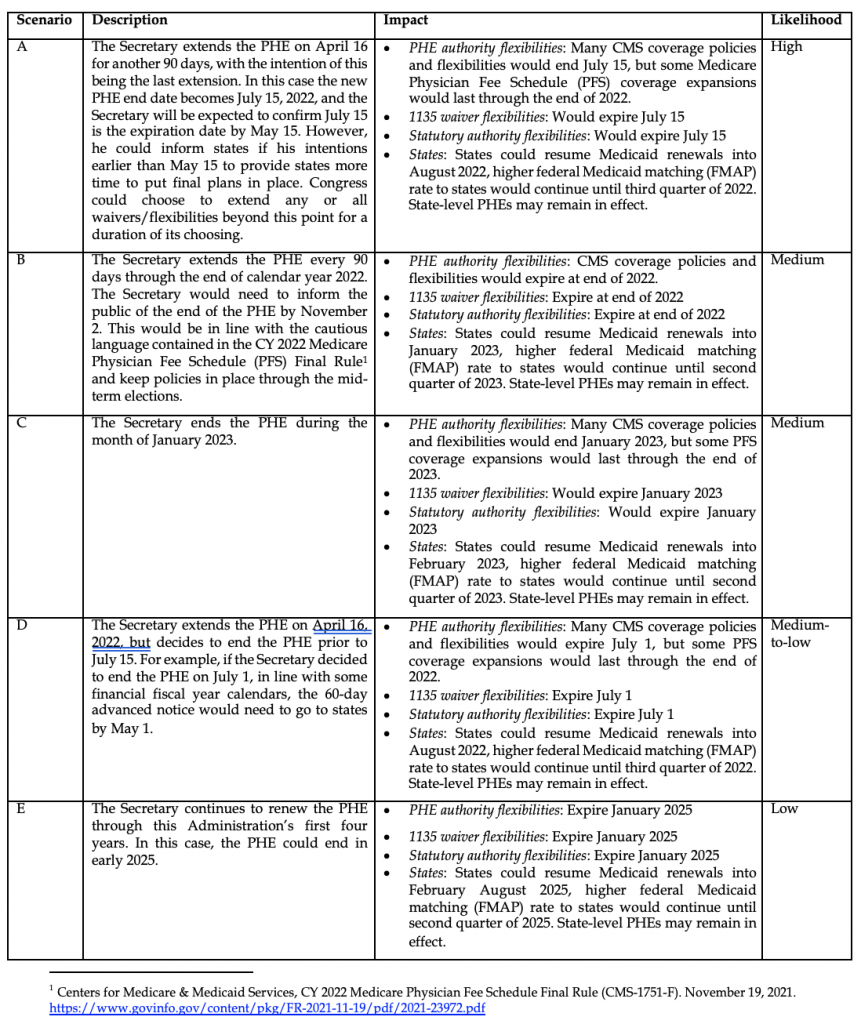
We outline five different scenarios federal policymakers may consider for ending the PHE and unwinding COVID-19 flexibilities. These scenarios will have varying impacts on patients, providers, plans, and other stakeholders as policymakers hope to “return to normal.” Further, Congress could act to temporarily extend any or all of the PHE waivers and flexibilities for a period of time after the expiration of the PHE.
Conclusion
While we have generally described potential end dates for the PHE and identified three major implications, there are other important nuances to these scenarios.
- If either or both the PHE and the national emergency declaration end, the Section 1135 waivers would also end. By contrast, if both declarations remain in place, HHS and CMS could choose to proactively begin to phase out the blanket and state-specific waivers.
- HHS and CMS could extend some of the flexibilities not directly linked to the emergency authorities. For example, HHS and CMS could extend certain enforcement discretion policies for some period of time.
- Congress could approve temporary statutory changes to the expiration timelines of any of the COVID-19 related flexibilities. For example, there is strong bipartisan support for Congress to enact additional changes to Medicare’s telehealth coverage and reimbursement policies. These telehealth policies are currently under consideration as Congress works to finalize the funding for federal fiscal year 2022. Similarly, stakeholders are also advocating for Congress to modify the statutory parameters for Medicaid’s higher federal matching rate and continuous coverage policy.
The end of the COVID-19 PHE declaration will result in a major shift in health care coverage and services as well as operations for the health care industry writ large. HMA experts are working with providers, payors, and other stakeholders to help them understand the impact of these scenarios and assist them in planning for the end of the PHE. We possess the tools needed to support providers, payors and other stakeholders as they implement an array of policy, procedural and operational changes to effectively manage the changes ahead.
For inquiries about how the potential expiration of the Federal Public Health Emergency might impact you and your patients/members/constituents please contact Zach Gaumer, Amy Bassano, and Andrea Maresca at Health Management Associates.
[1] HHS Office of the Assistant Secretary for Preparedness: https://www.phe.gov/Preparedness/legal/Pages/phedeclaration.aspx
[2] The CMS Interim Final Rules have effective dates: March 31, May 8, September 2 and November 2, 2020.
[3] HHS Office of the Assistant Secretary for Preparedness: https://www.phe.gov/Preparedness/legal/Pages/1135-waivers.aspx
[4] CMS COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers, Last updated May 24, 2021: https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf (Accessed 2/21/2022)
[5] Families First Coronavirus Response Act P.L. 116-127: congress.gov/bill/116th-congress/house-bill/6201/text
[6] As posted by Center for Children and Families: https://ccf.georgetown.edu/wp-content/uploads/2021/01/Public-Health-Emergency-Message-to-Governors.pdf
[7] Inside Health Policy, “Becerra Extends Public Health Emergency, COVID-19 Waivers,” December 18, 2021 (Behind pay wall)
[8] Centers for Medicare & Medicaid Services, CY 2022 Medicare Physician Fee Schedule Final Rule (CMS-1751-F). November 19, 2021. https://www.govinfo.gov/content/pkg/FR-2021-11-19/pdf/2021-23972.pdf