This week, our In Focus reviews the Louisiana Medicaid managed care organizations (MCOs) request for proposals (RFP), released by the Louisiana Department of Health (LDH) on February 25, 2019. Selected MCOs will manage health care services for more than 1.5 million Medicaid enrollees statewide, starting January 2020.
LDH intends to contract with up to four MCOs to provide full-risk, Medicaid-covered medical, preventive, and rehabilitative services. This is the third procurement for the managed care program, with contracts worth more than $8 billion.
Eligibility
According to the RFP, the following Medicaid populations will be automatically enrolled in Medicaid managed care:
- Children under 19 years old and optional groups of older children in the following categories:
- CHAMP-Child Program
- Deemed Eligible Child Program
- Youth Aging Out of Foster Care
- Former Foster Care Children
- Regular Medically Needy Program
- LaCHIP Program
- Blind/Disabled Children and Relation Populations
- Foster Care Children
- Parents and Caretaker Relatives
- Parents and Caretaker Relatives Program
- Regular Medically Needy Program
- Pregnant Women
- LaMOMS (CHAMP-Pregnant Women)
- LaCHIP Phase IV Program
- Breast and Cervical Cancer (BCC) Program participants
- Aged, Blind, and Disabled adults
- Continued Medicaid Program participants
- Tuberculosis (TB) Infected Individual Program participants
- Beneficiaries in the Adult Expansion category
The RFP also includes other mandatory MCO populations that receive certain services only.
The following Medicaid populations may voluntarily participate in Medicaid managed care by opting-in:
- Non-dually eligible individuals receiving services through the following 1915(c) Home and Community-Based Services (HCBS) waivers:
- Adult Day Health Care Waiver (ADHC)
- New Opportunities Waiver (NOW)
- Children’s Choice Waiver (CC)
- Residential Options Waiver (ROW)
- Supports Waiver
- Community Choices Waiver (CCW)
- Individuals under the age of 21 who are listed on the Office for Citizens with Developmental Disabilities’ (OCDD’s) Request for Services Registry
Evaluation
LDH is looking for MCOs that can best achieve a “Triple Aim” of better health, better care, and lower costs. MCOs that apply must have five years of experience in a Medicaid managed care program and must have been awarded a contract as a Medicaid MCO within the last 36 months for a population equal to or greater than Louisiana.
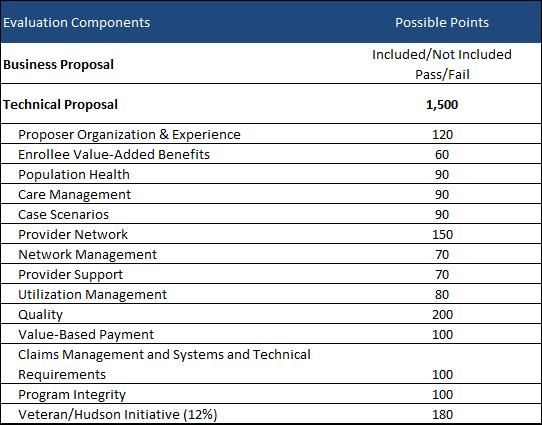
An evaluation team will score the plans pass/fail for the business proposal and out of 1,500 points for the technical proposal. Plans must score at least a total of 660 points and must score 50 percent of total available points in the following technical categories: Organization & Experience; Enrollee Value-Added Benefits; Population Health; Care Management; Case Scenarios; Provider Network; Network Management; Provider Support; Utilization Management; Quality; Value-Based Payment; Claims Management and Systems and Technical Requirements; and Program Integrity.
Plans with the highest scores will be chosen.
There is no competitive bidding process for capitation rates. LDH will establish a Per Member Per Month (PMPM)-actuarially sound, risk-adjusted rate.
Timeline
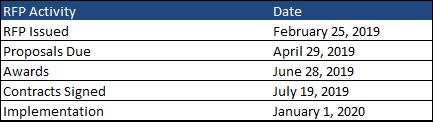
Proposals will be due April 29, 2019, with awards announced on June 28, 2019. The contracts will run from January 1, 2020, through December 31, 2022. LDH also has an option to extend the contract for up to 24 additional months.
Current Market
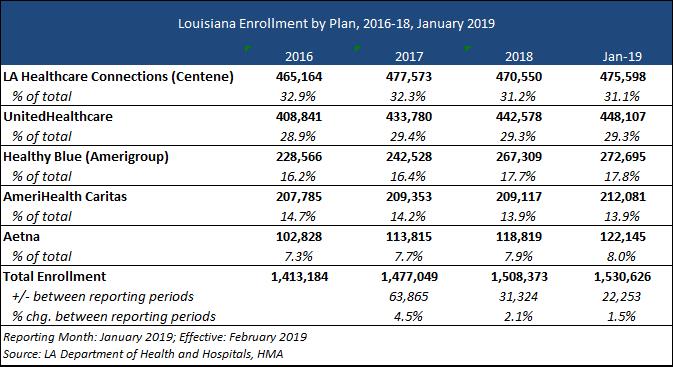
The Louisiana Medicaid managed care program has approximately 1.5 million members, as of January 2019. Louisiana Healthcare Connections (a Centene health plan) has the largest share of members at 31 percent, with UnitedHealthcare having the next largest market share with 29 percent of members.