This week, our In Focus reviews the Massachusetts One Care Dual Demonstration 2.0 request for responses (RFR), released by the Massachusetts Executive Office of Health and Human Services (EOHHS). One Care will cover Medicare and Medicaid dual eligible adults with disabilities ages 21 through 64 and includes medical, behavioral, Long-term Services and Supports (LTSS), community supports, and care management services statewide.
One Care
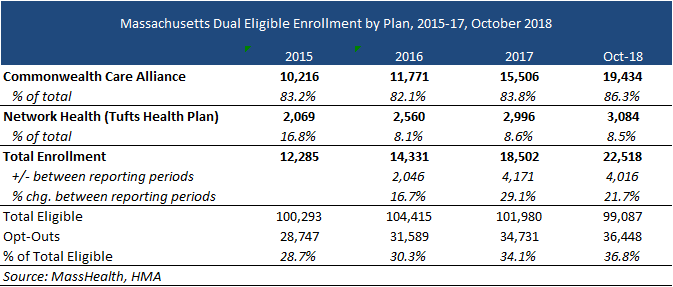
One Care launched in 2013 as an 1115 duals demonstration waiver (both a capitated model demonstration under the Financial Alignment Initiative and a state demonstration to integrate care for dual eligible individuals). The current program serves approximately 22,500 members through Tufts Health Plan and Commonwealth Care Alliance. One Care will focus on integrated care management and care coordination through an Interdisciplinary Care Team (ICT). Plans will have flexibility to innovate around care delivery and to provide a range of community-based services as a way to promote independent living and alternatives to high-cost traditional services. Goals will focus on the following:
-Integrated Care Management
- Employ best practices in complex care management, practice-based care management, and flexible community-based supports;
- Improve linkages for ICTs to effectively communicate and coordinate care at the enrollee’s direction;
- Further engage and empower enrollees in leading or self-directing their care, including through engagement with their ICTs and care planning processes; and
- Engage providers through the care model to partner with One Care Plans using innovative approaches.
-Innovative Provider Contracting and Purchasing
- Leverage value-based purchasing approaches that incorporate quality benchmarks and/or specific outcomes in the payment models (i.e. quantitatively valuing quality and outcome improvements);
- Develop population-health based preventive approaches and proactive strategies to shift utilization from acute and other facility settings to community settings;
- Design alternative care approaches to reduce and avoid unnecessary acute, emergency, and hospital-based care; and
- Design and invest in alternative care approaches that prevent, avoid, delay, and reduce unnecessary nursing facility admissions and care, including returning Enrollees from nursing facilities to the community.
-Community Living and Engagement
- Support individuals with disabilities to live independently in the community;
- Deepen support for individuals with Intellectual or Developmental Disabilities (ID/D) and Autism Spectrum Disorder (ASD) and their families;
- Facilitate effective communication access and address accessibility; and
- Partner with community-based experts to develop effective strategies to promote community living, and rebalancing, and to engage enrollees.
Outcomes, Social Determinants, and Health Disparities
- Improve Enrollee outcomes and quality of life;
- Address social determinants of health;
- Identify and address health disparities and inequities; and
- Strategically partner with housing Providers, including to more effectively support chronically homeless populations.
-Eligibility and Enrollment
- Proactively address eligibility churn, including through deemed continued eligibility;
- Drive self-selected enrollment;
- Find and meaningfully engage individuals who may be hard to locate; and
- Improve Enrollee engagement and satisfaction to reduce voluntary disenrollments.
Eligible Populations
One Care plans will serve dual eligible beneficiaries who are:
- Adults with physical disabilities;
- Adults with Intellectual or Developmental Disabilities (ID/D)
- Adults with Serious Mental Illness (SMI)
- Adults with Substance Use Disorders (SUD)
- Adults with disabilities who have multiple chronic illnesses or functional or cognitive limitations
- Adults with disabilities who are homeless
Awards
EOHHS expects to award contracts to three plans but may award up to five. Plans can bid in as few as one or as many as all 14 counties, and in full or in partial counties. Subsequently, they can be awarded in all, some, or none of their proposed counties or partial counties. EOHHS also intends to enter into a two-way contract with each selected One Care Plan for additional services. Plans must include an Innovation Plan in their response.
Current Market
One Care serves approximately 22,500 individuals in nine counties. The current One Care contracts were extended though December 31, 2019. Enrollment is through a voluntary opt-out process. In 2017, Massachusetts spent an estimated $546.9 million on Medicaid and Medicare services for One Care enrollees.
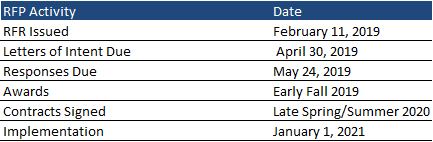
Timeline
The One Care RFR was issued February 11, 2019. Responses are due May 24, 2019, with awards announced in the early fall of 2019. Implementation will begin January 1, 2021, with contracts effective for five years through December 31, 2025, with five optional renewal years.