This week, our In Focus summarizes the findings of an HMA Information Services (HMAIS) analysis of Medicaid managed care rates in 2018 versus 2017. The analysis represents HMAIS’ first attempt at what will be an annual tracking of Medicaid managed care rate increases, which we will expand upon and refine over time with input from our readers and the Medicaid community. Complete results, including spreadsheets showing underlying analysis, will be made available to HMAIS subscribers. For information on how to subscribe, contact Carl Mercurio.
Rate Analysis
HMA Information Services, a division of Health Management Associates, calculated per member per month (PMPM) capitated rates paid to Medicaid managed care plans in 25 states. HMAIS was able to obtain comparable year-over-year data for 2018 versus 2017 in 19 of these states. The analysis provides a look at the level of rates paid for various key eligibility categories as well as the annual rate of increase.
It is important to note that any attempt to compare capitated rates across states is problematic because the cost of care, the way care is delivered, the member mix, benefit levels, and eligibility criteria vary from state to state. Even in a single state, annual changes in program parameters, benefits, and eligibility can make year-to-year rate comparisons difficult if not impossible.
Traditional Medicaid
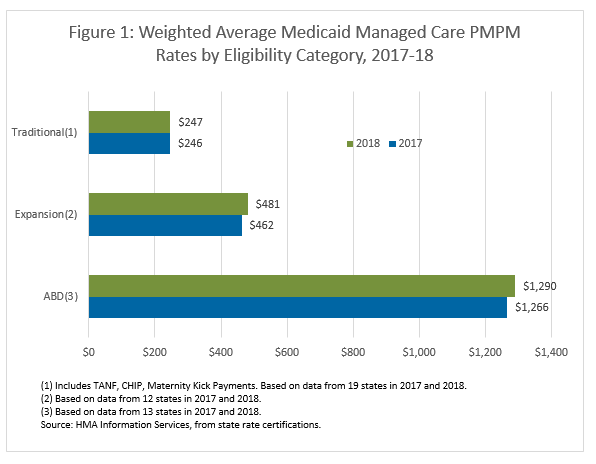
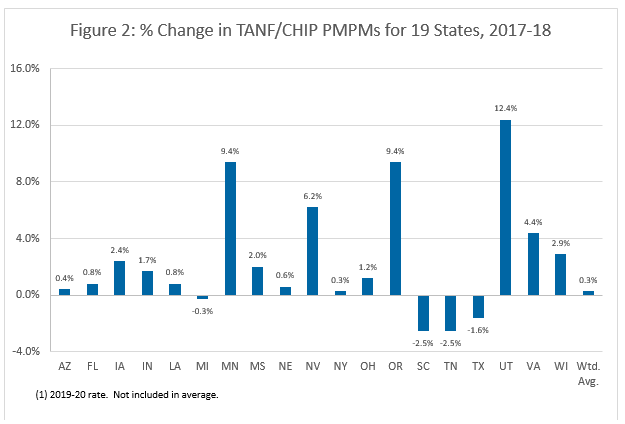
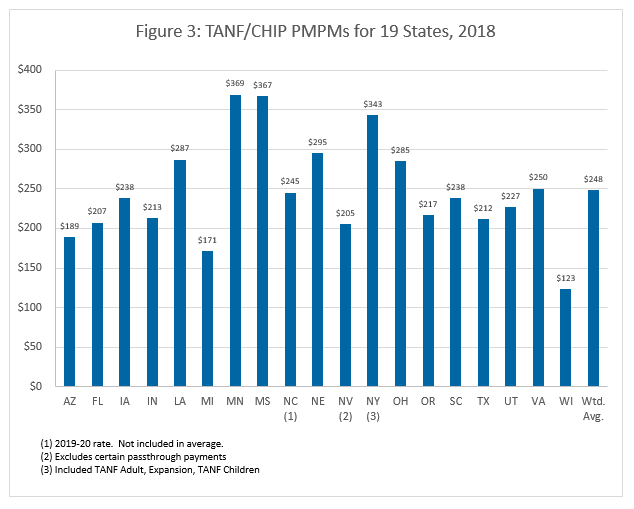
For traditional Medicaid (aka Temporary Assistance for Needy Families (TANF) and Children’s Health Insurance Program (CHIP) populations), the weighted average PMPM rate paid by 19 states to Medicaid managed care plans for the rating period ending in 2018 was $247, up 0.3 percent from $246 in 2017. The figures include TANF, CHIP, and maternity kick payments.
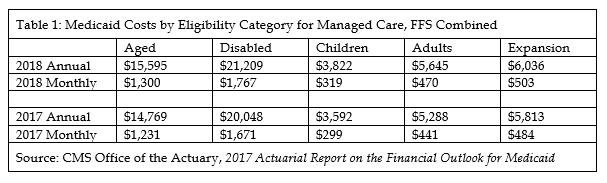
The rates are lower than Medicaid costs presented by the U.S. Office of the Actuary in its 2017 Actuarial Report on the Financial Outlook for Medicaid, which estimates that annual Medicaid costs per child were $3,822 in 2018, or about $319 per month; however, it is important to note that the actuarial report includes costs for both Medicaid managed care, Medicaid fee-for-service, and other programs.
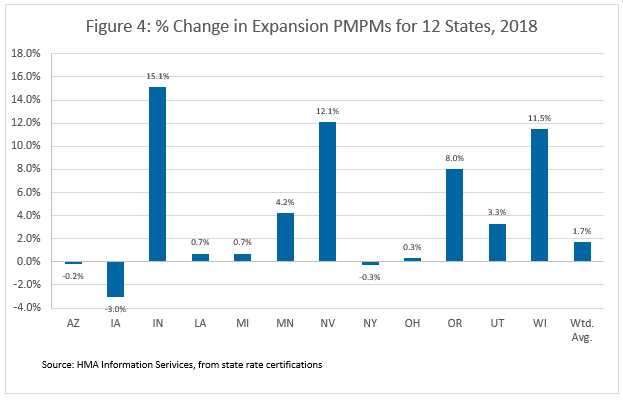
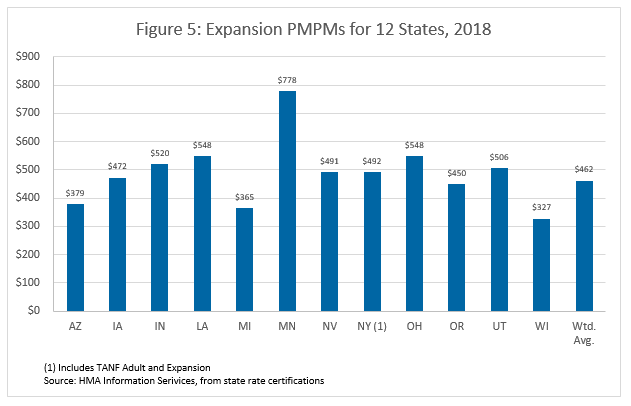
Medicaid Expansion
For Medicaid expansion populations, the weighted average PMPM rate paid by 12 states to Medicaid managed care plans for the rating period ending in 2018 was $481, up 4 percent from $462 in 2017.
The rates are lower than Medicaid costs presented by the U.S. Office of the Actuary in its 2017 Actuarial Report on the Financial Outlook for Medicaid, which estimates that annual Medicaid costs per expansion adult were $6,036 in 2018, or about $503 per month. Again, the actuarial report includes costs for both Medicaid managed care and Medicaid fee-for-service.
Aged, Blind, and Disabled
For aged, blind, and disabled (ABD), the weighted average PMPM rate paid by 13 states to Medicaid managed care plans for the rating period ending in 2018 was $1,290, up 1.9 percent from $1,266 in 2017. The figures include states with Medicaid managed care ABD programs that variously cover some or all the following: acute care, short-term nursing home stays, home and community-based services, long-term services and supports, the Medicaid portion of duals, and in a few cases long-term nursing home stays.
Unlike for TANF and expansion, this report does not provide a state-by-state chart comparing ABD rates and percentage changes because the programmatic variation is too great.
Overall, the weighted average rate is lower than Medicaid costs presented by the U.S. Office of the Actuary in its 2017 Actuarial Report on the Financial Outlook for Medicaid, which estimates that annual Medicaid costs per disabled member were $21,209 or $1,767 per month in 2018, and costs per aged member were $15,595 annually or $1,300 per month. Again, it is important to note that the actuarial report includes costs for both Medicaid managed care, Medicaid fee-for-service, and other programs.
For questions, please contact Carl Mercurio.