This week, our In Focus is the second in a series written by HMA Medicaid Market Solutions (MMS), which has worked with a number of states to design and implement Section 1115 Demonstration Waivers that support individual state goals for member engagement and personal responsibility while complying with new Centers for Medicare and Medicaid Services (CMS) guidance.
A joint letter from then-Health and Human Services (HHS) Secretary Tom Price and CMS Administrator Seema Verma released March 2017[1] promoted state flexibility for Medicaid program design and implementation. This announcement prompted states to submit 1115 demonstration requests to allow new policies and requirements for targeted Medicaid beneficiaries. Many of these demonstrations have proposed aspects of “personal responsibility,” including benefit packages and cost structures that align more with commercial insurance, member accounts that act more like health savings or flexible spending accounts, premium assistance to help beneficiaries access commercial health insurance, and requirements to participate in work or work-equivalent activities as a condition of eligibility.
One of the most considered and controversial state requests for 1115 demonstration waiver authority is to require targeted Medicaid populations to complete work or “work-equivalent” activities as a condition of eligibility. On January 11, 2018, the CMS issued policy guidance[2] for states that wanted to require work, training, and other similar activities for their Medicaid populations. CMS called these activities “community engagement,” citing the agency’s longstanding support for work and other forms of community involvement as a component of sustained health and independence. The guidance laid out policy and operational guidelines for states, including restrictions on who could be required to participate and recommending alignment with existing program policies and processes.
To date, three states—Kentucky,[3] Indiana,[4] and Arkansas[5] — have been granted approval to implement community engagement requirements as a condition of eligibility for certain Medicaid beneficiaries. While each state program goal and design aligns with the CMS guidance, there are key differences that highlight the many decision points states and stakeholders face when designing and implementing a community engagement requirement.
Populations that Qualify for Community Engagement
Flexibility exists for the specific populations states might require to participate in community engagement activities as a condition of eligibility; however, CMS guidance excludes certain individuals from community engagement requirements. The guidance restricts states from applying penalties for non-compliance with community engagement to pregnant women, children under age 19, and individuals who are elderly, medically frail, or eligible for Medicaid due to disability. The guidance also indicates that individuals enrolled in the Supplemental Nutrition Assistance Program (SNAP) and/or Temporary Assistance for Needy Families (TANF) program are subject to the work requirements and exemptions for those programs; and regardless of the state’s requirements, individuals on SNAP and TANF meeting work requirements would automatically be considered meeting their state’s Medicaid community engagement requirements. Medicaid populations outside of these exclusions are described by CMS as “working-age, non-pregnant adult Medicaid beneficiaries who qualify for Medicaid on a basis other than a disability.”
The Medicaid beneficiaries subject to community engagement requirements vary based on which Medicaid beneficiaries are included in the state’s demonstration request. Kentucky, Indiana, and Arkansas are all Medicaid expansion states, and the community engagement requirements for all three states apply to the expansion adult, or newly eligible adult group. Kentucky’s and Indiana’s approved demonstrations also include targeted individuals outside of the Medicaid expansion population, including individuals eligible as very low-income parents and caretakers, and those that move from this group to transitional medical assistance coverage when they gain employment.
Some states have also chosen to limit their community engagement requirement with age restrictions. All three state demonstrations provide medical benefits for individuals age 19-64; but Kentucky is the only state where community engagement requirements align with this eligibility criteria. Indiana’s community engagement requirements will apply to individuals age 19-59 aligning with the state’s TANF requirements; and Arkansas’ community engagement requirements will apply to individuals age 19-49, aligning with SNAP requirements.
CMS guidance also recognized that many individuals that fail to meet the Medicaid definition of “disabled” still face significant challenges getting and holding jobs, and acknowledged the need for exemptions from the community engagement requirements. Aligning with CMS guidance, all three states exempt medically frail individuals,[6] but each state has flexibility in how it defines and identifies this population. States may choose to take a broader view of the medically frail designation; or may develop a narrower definition for medically frail while providing exemptions under other categories, if the definition meets federal requirements. For example, both Kentucky and Indiana exempt homeless individuals from community engagement requirements; but Kentucky does so as a part of its medically frail definition whereas Indiana offers a separate exemption for homeless individuals and reserves its medically frail definition for more complex chronic diseases.
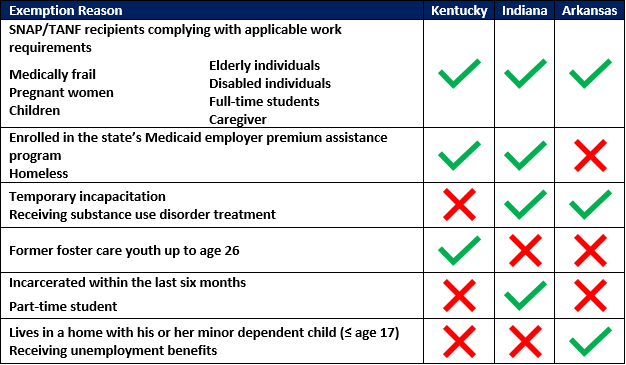
In addition to the exemptions defined by CMS (medically frail, pregnant women, children, elderly individuals, SNAP/TANF recipients complying with applicable work requirements, and disabled individuals), each state has been approved to include additional exemptions in its 1115 demonstration, detailed in Table 1.
Table 1. Community engagement exemptions, by state
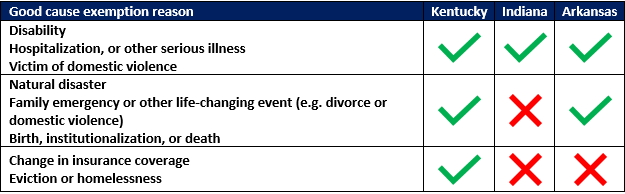
In addition to longer-term exemptions, Kentucky, Indiana, and Arkansas have also aligned with the SNAP/TANF policy of offering good cause exemptions to individuals who may have failed to meet requirements due to some unexpected circumstances beyond their control, such as disability,[7] hospitalization, and other serious illnesses for the beneficiary or a member of the beneficiary’s household. In addition to these common good cause exemption reasons, the approved demonstrations also vary on some of the good cause exemptions they currently anticipate approving. Some examples of different good cause exemptions are highlighted in Table 2, but all three states with approved community engagement waivers have authority to add good cause exemptions as appropriate.
Table 2. Good cause exemption reasons, by state
Participation Requirements, Eligible Activities, and Consequences for Non-Compliance
The level of participation required, the types of activities that will meet the requirement, and the consequences for failing to comply with the requirements vary between the demonstrations approved to date. Currently, all approved community engagement demonstrations will require beneficiaries to complete at least 80 hours of qualified activities per month.
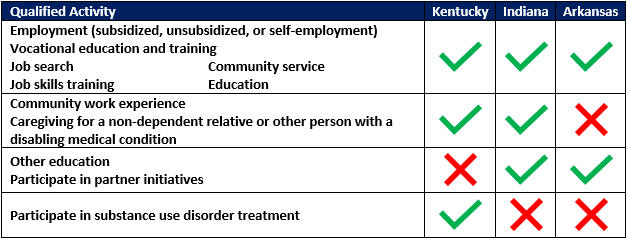
The types of activities beneficiaries can complete to meet their community engagement requirement are generally similar from state to state, including employment (subsidized, unsubsidized, or self-employment), job search, job skills training, vocational education and training, community service, and education (such as high school, GED, college or graduate education, or English as a second language, or other education related to employment). Qualified activities are detailed in Table 3. Non-exempt beneficiaries may complete a combination of these activities to meet their community engagement requirements.
Table 3. Qualified activities, by state
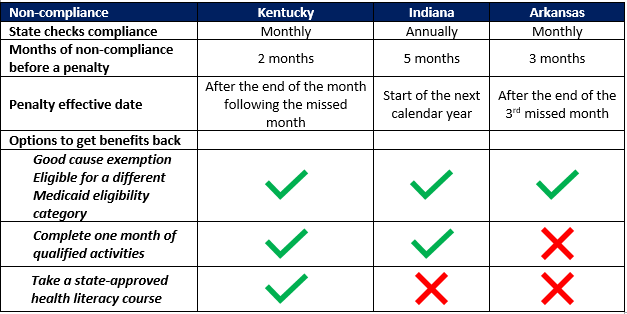
States will need to consider the consequences for beneficiaries who do not meet the community engagement requirement. Kentucky, Indiana, and Arkansas were all approved to withhold benefits for non-exempt beneficiaries who do not meet the state’s community engagement requirement. However, the frequency with which the states check compliance, the number of months non-exempt beneficiaries must meet the requirements, opportunities to avoid the penalty, the length of time these beneficiaries could be without coverage and beneficiary options to regain access to their benefits vary significantly across the states. This variation is detailed in Table 4.
Table 4. Non-compliance policies, by state
Implementation and Roll-Out
Just as there is a great deal of variation in policy, the three states with approved community engagement demonstrations have each planned very different roll-outs for their demonstrations. Each of the states differs in its roll-out date and the populations and geographic areas to which the requirements will apply. The states are also considering their options and existing resources for stakeholder outreach and education, as well as necessary systems and contract updates to ensure necessary information is captured and evaluated, in compliance with federal requirements and the terms of their demonstrations.
Implementation dates for the three approved demonstrations will be spread out, and the non-exempt populations will be affected differently over time. Arkansas will be the first state to implement the community engagement aspects of its program, starting June 1, 2018. Kentucky will follow Arkansas with a go-live date of July 1, 2018; and Indiana is scheduled to be the last to implement community engagement, starting January 1, 2019.
None of these states will have a statewide implementation for their entire non-exempt population on those implementation dates. Arkansas anticipates a statewide implementation, starting with its 30-49-year-old non-exempt beneficiaries, and is planning to add the 19-29 year old non-exempt beneficiaries later. Kentucky will require its full age range to participate, but will roll out the initiative by region. Indiana’s requirements will apply to the entire non-exempt population statewide, but will implement community engagement with an initial hour requirement of zero, and gradually increase the hour requirements over time.
The three states are also in the process of evaluating how they will gather and process all the new data related to community engagement. They will all need to be able to:
- Capture data to help them evaluate whether their community engagement initiative met its goals
- Assess which demonstration participants are eligible for exemptions
- Track which beneficiaries are meeting the requirements and which are not
Kentucky, Indiana, and Arkansas have also considered how non-exempt beneficiaries will track their hours and how those hours will be verified. This could result in necessary systems changes for their Medicaid eligibility systems and the systems of their vendors and partners, such as managed care organizations (MCOs). These states have also been looking at whether the necessary functionality exists in their current systems or if they will need to build or procure new systems. The three states are all still preparing to implement their community engagement initiatives, so there are still many operational unknowns; but both Kentucky and Arkansas have opted to leverage their existing SNAP work requirement tracking systems as a way for beneficiaries to report their time. It is also likely that Indiana will leverage one of its existing systems.
As community engagement will have an impact on beneficiary eligibility, the states and their partners are also developing or adapting member notices and appeals processes to address participation requirements, exemptions (including good cause exemptions), and non-compliance. The new notices could also draw more beneficiary questions, which could in turn increase call volume for Medicaid call centers and foot traffic for local Medicaid offices. To make sure call centers and local office workers are prepared to answer beneficiary questions, the states and/or their vendors are developing internal trainings and communications.
Kentucky, Indiana, and Arkansas may develop relationships with other state agencies and community-based organizations to garner their buy-in to the initiative and leverage their resources and expertise to help the states meet their goals around community engagement. All three states appear to look to their departments of workforce development as key resources to help connect beneficiaries to activities that would meet the community engagement requirements. Kentucky has also started holding stakeholder forums to educate possible community partners about the program.
If you are interested in learning more about this topic, please contact Lora Saunders at [email protected].
[1] Released March 14, 2017. Source: https://www.hhs.gov/sites/default/files/sec-price-admin-verma-ltr.pdf
[2] Released January 11, 2018. Source: https://www.medicaid.gov/federal-policy-guidance/downloads/smd18002.pdf
[3] Approved January 12, 2018. Source: https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ky/ky-health-ca.pdf
[4] Approved February 1, 2018. Source: https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-ca.pdf
[5] Approved March 5, 2018. Source: https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ar/ar-works-ca.pdf
[6] Medically frail individuals are described at 42 CFR 440.315(f) as individuals with: disabling mental disorders (including adults with serious mental illness); chronic substance use disorders; serious and complex medical conditions; a physical, intellectual, or developmental disability that significantly impairs their ability to perform one or more activities of daily living; or a disability determination based on Social Security criteria or State pan criteria (if more restrictive). Source: https://ecfr.io/Title-42/pt42.4.440#se42.4.440_1315
[7] Someone with a disability as defined by the ADA, section 504 of the Rehabilitation Act, or section 1557 of the Patient Protection and Affordable Care Act may not qualify as disabled under other federal definitions that would exempt the person from community engagement requirements in the three waivers approved to date.