This week, our In Focus section reviews the Nevada Medicaid and Child Health Insurance Program (CHIP) managed care request for proposals (RFP) released by the Nevada Department of Health and Human Services, Division of Health Care Financing and Policy (DHCFP) on March 17, 2021. The RFP is for the current service area covering two urban counties of the state, Clark and Washoe; however, the state may extend the geographic service area under the contract. Through this RFP, Nevada seeks to advance the state’s goals of “improved clarity and oversight of requirements; increased focus on care management, member engagement, and access; and continued progress towards integration of services and efficiency.”
Contracts are worth approximately over $2 billion annually. DHCFP’s actuary will hold a public meeting on April 2, 2021, to present an overview of the calendar year 2022 rate development to potential bidders.
Selected managed care organization (MCOs) must also participate in the state-based Affordable Care Act (ACA) Exchange, providing at least one Silver and one Gold Qualified Health Plan (QHP) by 2024. This is to ensure continuity of care for individuals and families who may have a change in Medicaid or CHIP eligibility status. The offerings must also meet the requirements of an MCO Transition QHP.
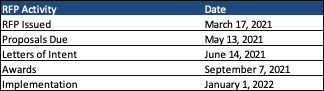
RFP Timeline
Contracts will run from January 1, 2022, to December 31, 2025, with a possible two-year extension. Proposals are due May 13, 2021, and awards are expected to be announced September 7, 2021.
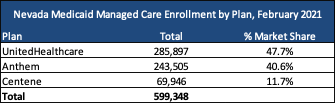
Current Market
Current incumbents are Anthem/Amerigroup, UnitedHealthcare/Health Plan of Nevada, and Centene/SilverSummit Health Plan, who collectively serve nearly 600,000 individuals. The last procurement was in 2016. MCOs cover benefits including physical health, behavioral health, and prescription drugs, and serve approximately 72 percent of the state’s Medicaid and CHIP population. The rest receive benefits through a fee-for-service delivery model.
Enrollment in managed care is mandatory for recipients under the family medical categories, the Nevada Check Up program (the state’s CHIP program), and the aged out of foster care coverage group when there is more than one MCO option in the geographic service area. Eligible Native American populations and children with Special Health Care Needs (CSHCN) or Severe Emotional Disturbance (SED) can choose to opt out of managed care. Excluded populations from managed care include: individuals in foster care/child welfare, individuals in an intermediate care facility with intellectual disabilities, individuals receiving services in a Nursing Facility (NF) for over 180 days, individuals receiving hospice services, individuals enrolled in a 1915(c) Home and Community Based Services waiver program, and individuals admitted to a swing bed stay in an acute care hospital for over 45 days.
Evaluation
The proposal evaluation process will consist of three phases:
- Phase I: Review of Mandatory Requirements
- Phase II: Review of Responses to Technical Questions
- Phase III: Oral Presentations (at state’s option)
The technical proposal will be scored out of a possible 1,500 points. MCO responses to each topic area will receive a numerical score of zero through five, correlating to a percentage of points earned, with zero being no points earned through five being 100 percent of points earned.
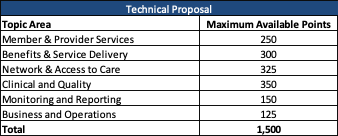
The state may also invite individual MCOs for an oral presentation but reserves the right to forego oral presentations and select winning MCOs based on the written proposal.