This week, our In Focus section reviews the North Carolina Department of Health and Human Services (DHHS) Medicaid Managed Care Proposed Policy Paper released on May 16, 2018, Prepaid Health Plans in North Carolina Medicaid Managed Care, ahead of a competitive procurement for the new Medicaid managed care program expected to be released in spring or summer 2018. North Carolina will be contracting with statewide Medicaid managed care organizations (Commercial Plans, CPs) as well as regional provider-led managed care entities (Provider-Led Entities, PLEs) to serve 1.9 million Medicaid beneficiaries beginning in 2019. All plans are considered by the state to be Prepaid Health Plans (PHPs). The policy paper provides additional detail on the characteristics and requirements that apply to CPs and PLEs. To read HMA’s previous analysis of “North Carolina’s Proposed Program Design for Medicaid Managed Care,” click here.
North Carolina DHHS will award three statewide capitated PHP contracts and up to 12 capitated PHP contracts with PLEs to provide coverage by region. DHHS will encourage PLEs to bid on more than one region. It will also encourage PLEs to participate in other North Carolina insurance markets, including the individual health insurance marketplace. The request for proposals (RFP) is expected to include an opportunity for PHPs to make a commitment to offer Qualified Health Plans (QHPs) on the Federally Facilitated Marketplace (FFM). DHHS will grant points to RFP respondents for their commitment to participate, for their current participation status, and for their expected footprint in North Carolina in 2021.
PHPs will not need prior experience serving as a health plan to bid on the PHP procurement and may therefore be a new organization. Additionally, they may be formed by joint ventures or other partnerships between managed care organizations, health care providers or other organizations.
There is a total of six regions in the state:
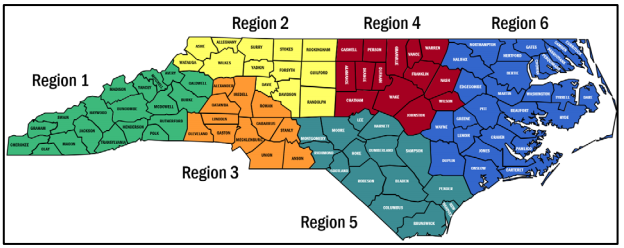
Selected plans in each region will have enrollment minimums and maximums for auto assignment. A region’s enrollment floor will be the greater of 10 percent market share or 20,000 lives and the enrollment ceiling will be 50 percent market share. The table below shows a breakdown per region.
Most Medicaid and NC Health Choice populations will be mandatorily enrolled in PHPs. However, mandatory enrollment for high-need populations will be phased in after the Medicaid managed care program is fully established. After full implementation of the managed care program, the following populations will be covered:
- AFDC and related MAGI populations
- Aged, Blind, and Disabled populations
- NC Health Choice and Medicaid-Expansion Children’s Health Insurance Program (MCHIP)
- Legal Aliens
- Long-term services and supports populations
- Foster Children, Adoption Children, and Former Foster children
- Dual eligibles (excluding partial duals and pending legislative change)
Meanwhile, the following populations will be excluded:
- PACE beneficiaries
- Medically needy beneficiaries
- Beneficiaries only eligible for emergency services
- Presumptively eligible beneficiaries, during the period of presumptive eligibility
- Beneficiaries eligible for Medicare, but not full Medicaid benefits
- Health Insurance Premium Payment (HIPP) beneficiaries
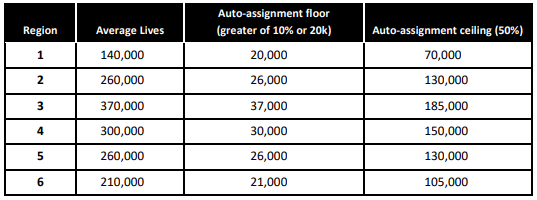
DHHS will set capitated rates for all PHPs. It will provide draft capitation rates as part of the PHP RFP. As a result, PHPs will not submit price bids to the RFP. The capitation rates will include an assumed underwriting gain of 1.75 percent of premium: 1.25 percent for the cost of capital and a risk margin of 0.5 percent. PHPs will be required to accept the rate setting and risk adjustment methodologies. The capitated rate-setting methodology will be based on the following elements:
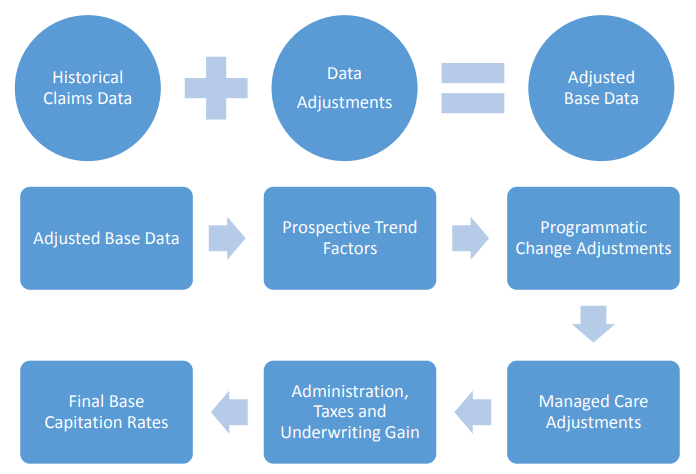
DHHS expects to set a remittance Medical Loss Ratio (MLR) threshold of approximately 88 percent and an overall minimum MLR threshold of approximately 90 percent. It will adjust the MLR thresholds by PHP based on the specific populations covered. To prevent PLEs from anti-competitive or self-dealing behaviors, such as paying its affiliated providers or subcontractors more than others, DHHS will include a clause in the RFP forbidding such actions.
PHPs will also be required to cover out-of-network services for enrollees. If the provider refuses to contract with the PHP or fails to meet quality standards, the PHP prohibited from reimbursing the provider more than 90 percent of the Medicaid fee-for-service rate for services.
Prepaid Health Plans in North Carolina Medicaid Managed Care Policy Paper