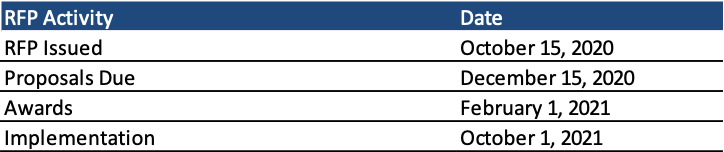
This week, our In Focus section reviews the statewide Oklahoma Medicaid managed care request for proposals (RFP) released by the Oklahoma Health Care Authority on October 15, 2020, and the North Dakota Medicaid expansion managed care RFP released by the North Dakota Department of Human Services, Medical Services Division on October 20, 2020.
Oklahoma
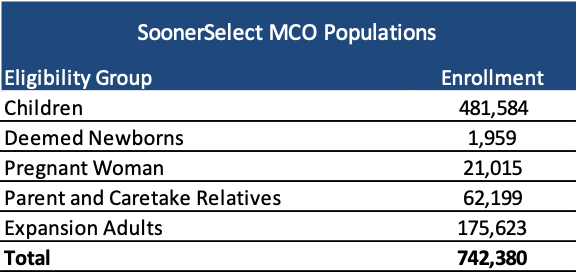
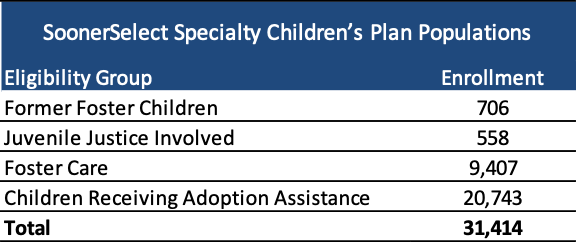
Oklahoma is procuring contracts, worth over $2 billion, for a new statewide Medicaid managed care program called SoonerSelect Plan, which would cover physical health, behavioral health, and pharmacy benefits for more than 742,000 Medicaid beneficiaries. The state will also contract with one of the selected Medicaid managed care plans for a statewide program called SoonerSelect Specialty Children’s Plan, which would cover 31,000 former foster children, juvenile justice-involved individuals, and children either in foster care or receiving adoption assistance.
CareSource already announced that it intends to submit a bid through CareSource Oklahoma, a new joint venture between the health plan and Texas-based administrative services provider Healthcare Highways.
Background
Oklahoma currently does not have a fully capitated, risk-based Medicaid managed care program. There are more than 900,000 Medicaid members. The majority are in SoonerCare Choice, a Primary Care Case Management (PCCM) program in which each member has a medical home. Other programs include SoonerCare Traditional (Medicaid fee-for-service), SoonerPlan (a limited benefit family planning program), and Insure Oklahoma (a premium assistance program for low-income people whose employers offer health insurance).
A previous attempt for managed care was canceled in June 2017 for SoonerHealth+, a planned Medicaid managed care program for the aged, blind, and disabled (ABD) population. The RFP was canceled due to a lack of funding. Start-up costs for SoonerCare+ were projected at more than $100 million over the first several years of the program, and a request for $52 million in near-term funding needed to move ahead with the RFP was denied by legislators.
The new Medicaid managed care contracts will provide benefits to SoonerCare children, deemed newborns, pregnant women, parent and caretaker relatives, and expansion adults. Medicaid expansion in the state is slated to go into effect on July 1, 2021. The SoonerSelect Specialty Children’s Plan will cover former foster children, juvenile justice involved population, foster care population, and children receiving adoption assistance.
The state also released a SoonerSelect Dental RFP for the procurement of statewide prepaid ambulatory health plans (PAHPs) to deliver risk-based dental benefits to nearly 774,000 Medicaid beneficiaries.
Timeline
Proposals are due December 15, 2020, and awards will be announced on February 1, 2021. The contracts will run for one year, with up to five optional one-year renewals. Implementation begins on October 1, 2021.
Evaluation
The evaluation process will consist of several steps. Under the administrative step, proposals will be evaluated on a pass/fail basis for timely submission, completeness, and compliance with general submission guidelines. The technical proposal will consist of 1,650 points. If the bidder submitted a proposal for the SoonerSelect Specialty Children’s Plan, the proposal will be scored out of 400 points. Only bidders awarded a SoonerSelect managed care organization (MCO) contract will be eligible to be awarded the SoonerSelect Specialty Children’s Plan contract. Oklahoma may negotiate with one, some, all, or none of the bidders after the scoring.
The state did not specify how many plans SoonerSelect Plan will contract with.
| Step | Possible Points |
| Administrative Review | Pass/Fail |
| Technical Proposal | 1,650 |
| Executive Summary | 25 |
| Staffing and Organizational Structure | 75 |
| References and Past Performance Information | 50 |
| Corporate Information and Experience in Improving Outcomes including:Oklahoma ExperienceMedicaid ExperienceProposed Oklahoma Economic Impact | 100 |
| Implementation Plan | 50 |
| Provider Network | 75 |
| Covered Benefits | 100 |
| Rural Health Strategy | 75 |
| American Indian/Alaska Native Health Understanding and Strategy | 50 |
| Care Management and Population Health | 150 |
| Medical Management | 100 |
| Quality Improvement | 100 |
| Health Plan Enrollee Services including:Health Plan Enrollee Grievance and AppealsCall Center | 75 |
| Provider Services including:Claims Payment ProcessingCall Center | 75 |
| Program Integrity | 75 |
| Information Technology Including:General Requirements ResponseEncounter ProcessingInteroperability Rule ReadinessHIE ResponseSystem Security and PrivacyBusiness Continuity and Disaster Recovery Plan | 100 |
| Financial Standards and Third Party Liability | 75 |
| Reporting | 50 |
| Behavioral Health Integration | 100 |
| Value-Based Payment Strategy | 50 |
| Case Studies | 75 |
| Contractor Performance/Compliance Strategy | 25 |
| SoonerSelect Specialty Children’s Plan Evaluation | 400 |
| Technical Approach and Experience with Specialty Populations | 70 |
| Staffing | 30 |
| Covered Benefits | 40 |
| Medical Management | 30 |
| Care Management and Transition of Care | 75 |
| Health Plan Enrollee Services | 35 |
| Provider Network | 30 |
| Case Studies | 30 |
| Quality Improvement | 20 |
| Inter-Agency Coordination and Data Sharing | 40 |
North Dakota
The North Dakota Department of Human Services, Medical Services Division, released an RFP for up to two Medicaid MCOs to serve the Medicaid expansion population. As of March 2020, current incumbent Sanford Health Plan serves approximately 19,800 expansion members.
The state implemented Medicaid expansion in 2014 to adults without dependent children with incomes at or below 138 percent of the federal poverty level. The state found that the population experiences a significant amount of churning, based on eligibility data collected from 2017-18. Over the two-year period, an estimated 13 percent of enrollees had gaps in coverage, with the average duration of eligibility being 13 months during the two-year period. However, since the COVID-19 pandemic, Medicaid expansion members have not been disenrolled.
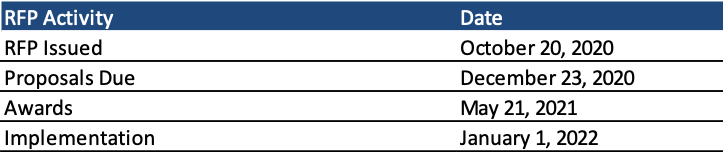
Timeline
Proposals are due December 23, 2020, with awards to be announced on May 21, 2021. Contracts run from January 1, 2022, through December 31, 2025. The state can extend the contract for up to 12 additional months.
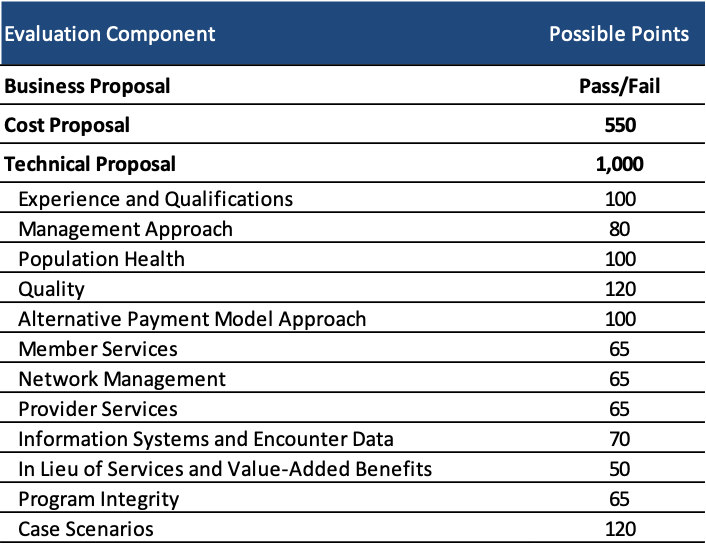
Evaluation
Technical proposals will be scored out of 1,000 points. A bidder must obtain at least 660 points on the technical proposal to have its cost proposal to be evaluated. Cost proposals will be assigned up to 550 points.