
April 30, 2025
Preparing for Change: The TEAM Model and What Medicare’s 2026 Inpatient Proposed Rule Means for Hospitals
HMA Insights – including our new podcast – puts the vast depth of HMA’s expertise at your fingertips, helping you stay informed about the latest healthcare trends and topics. Below, you can easily search based on your topic of interest to find useful information from our podcast, blogs, webinars, case studies, reports and more.

Preparing for Change: The TEAM Model and What Medicare’s 2026 Inpatient Proposed Rule Means for Hospitals

Multi-sector consensus-based alliances, rooted in collaboration, are a critical tool for cutting through the divisive partisanship of our national discourse, providing a pathway to sustainable progress. Through the Leavitt Center for Alliances, an initiative of Health Management Associates, we have helped diverse stakeholders—public and private, government and industry, nonprofit and corporate—solve dozens of the most entrenched challenges in health care.
Consensus-based alliances can solve complex challenges faster and more creatively than any one organization alone. With the recent publication of several case studies on the Leavitt Center for Alliances website, the tools for collaboration are now more accessible than ever. The site offers a window into the Center’s proven alliance framework and showcases a range of successful collaborations that exemplify how shared purpose, a commitment to consensus, and structured governance can drive real-world impact.
The case studies bring this to life, illustrating the diversity of issues that alliances can address when built on trust, structure, and shared purpose:
In our own ongoing work, ranging from behavioral health integration to payment reform and data interoperability, we see firsthand how alliances are helping translate federal policy shifts into systems change. These examples reveal what’s possible when stakeholders move beyond silos and toward collective action

Hospitals that use specially designated new technologies in the inpatient setting may receive additional reimbursement through a program offered by the Centers for Medicare & Medicaid Services (CMS) known as the new technology add-on payment (NTAP) program. CMS offers a separate NTAP payment in addition to the regular Medicare Severity-Diagnosis Related Group (MS-DRG) payment, for use of specially designated new technologies that qualify. This payment is meant to remove some of the disincentives faced by hospitals under the bundled inpatient payment system, when the costs of new technologies are not incorporated into the payment rates until two to three years after market entry. At a recent webinar, HMA Principal Clare Mamerow discussed the NTAP program, what manufacturers must do to apply for and receive NTAP designation for their new technologies, and some of the changes coming in 2025. This blog shares some of the key issues raised.
While NTAP designation can offer manufacturers of new technologies a significant advantage, the NTAP application process can be intense, arcane, and difficult to navigate without proper guidance. Most products applying for NTAP need to meet three criteria: newness, cost, and substantial clinical improvement. Certain other products – breakthrough devices and certain antibiotic and antimicrobial drugs – are deemed to have already met the newness and substantial clinical improvement criteria and therefore, only need to show that the cost criterion is met. This alternative application pathway is significantly streamlined and makes gaining NTAP designation much easier for these special products because the majority of products that fail to meet the three criteria miss substantial clinical improvement.
The newness criterion has two facets. First, the product must be newly on the market (received FDA approval recently, but prior to May 1, 2026) and must not be “substantially similar” to other available products. CMS looks to whether the product has a different mechanism of action or whether the product treats a new or different disease or patient population in making a substantially similar determination.
The cost criterion involves an analysis of Medicare claims data, where claims from two years ago are identified as cases where the new product could have been used had it been available and then repriced to account for the cost of the new technology. The average charges on those claims are compared to a DRG specific thresholds that CMS calculates. If the claim charges exceed the threshold, the cost criterion is met.
Finally, the substantial clinical improvement criterion requires that applicants show that patient outcomes are better with treatment with the new technology. Outcomes such as reduced mortality, reduced complications, and reduced health care utilization are all examples of clinical improvement. CMS takes a totality of the circumstances view of substantial clinical improvement, so applicants are encouraged to provide as much data as possible to support their application.
While NTAP can provide supplemental payments in some circumstances, it’s important to understand the program’s limits. The NTAP payment that hospitals receive is calculated on a claim-by-claim basis, with the payment at the lesser of 65% of the cost of the product, or 65% of the cost above the regular DRG payment. This means that hospitals are only made aware of the payment amount after the claim has been submitted, and that the hospital can never be made whole for the use of the new technology. In addition, the payment can be any amount less than 65% of the cost of the product—it’s even possible that the hospital will receive no payment if the cost of the case isn’t high enough to trigger the payment. Certain antibiotics and gene therapies that treat sickle cell disease receive a high payment, up to 75% of the cost of the product. Additionally, the payments are only applicable to Medicare fee-for-service claims in IPPS hospitals. Medicare Advantage, Medicaid, and commercial hospital claims are not eligible for payments. Finally, NTAP eligibility only extends for 2-3 years after market entry.
Although the NTAP application deadline for FY 2027 has not yet been announced, manufacturers of new technologies with an interest in NTAP should begin preparing their applications soon.
HMA experts in Medicare and Life Sciences can partner with your organization navigate the challenges in the NTAP program. If you are interested in learning more, contact us.

Late 2024, HMA convened a panel of experts, including individuals with lived experience and state leaders, to spotlight the critical need for cross-system transformation. The discussion underscored the importance of centering youth and family voices, aligning placement and community-based services, and leveraging opportunities like the Family First Prevention Services Act, Medicaid waivers, and specialty managed care models. As states grapple with a behavioral health workforce crisis and insufficient foster care placements, the path forward requires bold, coordinated strategies grounded in flexibility, equity, and evidence. This brief includes key takeaways from the 2024 panel and outlines actionable insights to guide the transformation of the children’s behavioral health system.

Section 1115(a) demonstrations, informally known as 1115 waivers, are experimental, pilot, or demonstration projects that give states flexibility to design, test, and evaluate state-specific approaches to improve their healthcare programs and better serve eligible populations.
Approved by the Centers for Medicare & Medicaid Services (CMS), 1115 demonstrations provide alternative options to provide access, coverage, financing, and delivery of services under the joint federal-state funded programs Medicaid and the Children’s Health Insurance Program (CHIP). Across multiple administrations, HMA has helped states write, design, implement and evaluate their 1115 demonstrations aimed at improving program and population health outcomes. Stakeholders need to optimize their role in shaping and implementing 1115 initiatives with practical solutions and effective engagement strategies with states.
Medicaid and CHIP 1115 demonstrations allow states—and their stakeholders—to test new innovations to improve the health of enrollees and advance program efficiencies. These demonstrations require careful planning, political savvy, policy knowledge, and ongoing support through the application, approval, and implementation phases. In today’s environment, 1115 programs must be responsive to the policy priorities at the federal level and grounded in solutions that work in the state. Stakeholders need aligned engagement strategies and communications plans to achieve shared goals, including monitoring that drives continuous improvements after implementation.
HMA consultants bring extensive real-world and leadership expertise from decades of working with states and federal agencies prior to joining HMA. We offer the range of services and support needed to advance 1115 programs, including:
Strengthening healthcare safety net sustainability through financial and operational supports
Developing solutions for complex patient populations such as individuals who are justice-involved or have extensive behavioral needs including substance use disorder
Designing coverage strategies for critical social needs, such as community reintegration of vulnerable populations such as the justice involved, including when these require collaboration with agencies and programs beyond Medicaid
Supporting states in meaningful stakeholder engagement efforts, provider training and guidance, and other activities necessary for successful program implementation
Working with managed care organizations, health plans, providers, and other stakeholders to apply our expertise in implementing 1115 demonstrations
HOW HMA CAN HELP
Providing strategic and operational support to design demonstration programs
With several former state Medicaid directors and former CMS officials on staff, HMA helps states design successful new interventions to address the unique needs of their populations and ensures proposals meet CMS’ approval requirements and expectations, including aligning 1115 interventions with evolving federal priorities and objectives for the program. With HMA, states and stakeholders gain valuable insights on strategic engagement and partnerships.
Developing applications for 1115 demonstration proposals
HMA has supported a variety of 1115 initiatives in several states, including developing proposals for new, continuing, and amended 1115 demonstration programs. HMA consultants bring decades of experience in 1115 program design that covers all of the components critical to developing and operating 1115 programs – policy, actuarial and budgeting, operations, communications, project management, and IT.
Supporting federal negotiations for approval of state 1115 demonstration proposals
HMA helps states navigate the federal processes to secure approval for their 1115 initiatives. In many cases, HMA joins in active negotiations with the state agency to support federal negotiations. HMA has unique insight into federal approval parameters with former CMS officials.
Operational Support
We help stakeholders—including state agencies and their partners—manage the challenges of implementing new Medicaid or CHIP initiatives, with a focus on ensuring efficient integration and improvements in outcomes.
Evaluation and Assessment of section 1115 demonstrations
Federal regulations require evaluation of CMS-approved 1115 programs. HMA designs and conducts evaluation reports that meet federal requirements, such as hypotheses, data sources, and comparison strategies. HMA’s work on evaluation designs and evaluation reports has been held out by CMS as best practice models to other states for evaluating new policy interventions as well as for ongoing monitoring activities.
Developing materials for and supporting stakeholder engagement from design to implementation.
HMA works closely with states and their partners to engage stakeholders early in the 1115 process to ensure that communities and local organizations are involved in the planning and implementation of 1115 programs.
HMA has supported approved section 1115 demonstration programs testing new strategies for addressing substance use disorder (SUD), serious mental illness (SMI), and/or serious emotional disturbance (SED) through new flexibilities around the federal institution for mental disease (IMD) exclusion in seven states (Alabama, Colorado, Delaware, Indiana, Missouri, Ohio, and Oklahoma). In addition to initial and extension application support, HMA teams also support the evaluation and financial modeling components of 1115 demonstration development. In the last four years, we have delivered six evaluation designs, two midpoint progress assessments, two interim evaluations, and two summative evaluations approved by CMS. In general, HMA’s approved evaluation design plans use multiple evaluation methods, including a mixed-methods approach, drawing from various data sources, measures, and analytics, including quasi-experimental methods, to produce relevant and actionable study findings to conduct analyses. Additional 1115 demonstration program development activities include completing budget neutrality estimates and rate setting for new interventions proposed under demonstrations.
California is the first state in the nation to receive approval from CMS to provide detained and sentenced individuals with 90-day pre-release healthcare services and behavioral health linkages. HMA helps clients build administrative capacity, information technology, pre-release services, care management models, and Medicaid claiming infrastructure to meet their unique needs and leverage this significant state-federal demonstration opportunity. Our planning and implementation support spans the breadth of the CalAIM Justice-Involved Initiative including: the pre-release Medicaid application process, 90-day pre-release services, behavioral health links, Enhanced Care Management (ECM), and Community Supports services. In addition to California, HMA supported other states, such as Illinois and Maryland, with the design, approval, and/or implementation of justice-involved demonstrations approved by CMS. Learn more about CalAIM Justice-Involved Reentry Initiative Planning and Implementation Services.
HMA has supported multiple states in developing alternate approaches to Medicaid eligibility and enrollment tailored to their unique policy goals. For example, our consultants have worked with the Indiana Family and Social Services Administration on the program design, approval, and implementation of the Healthy Indiana Plan (HIP), Indiana’s alternative Medicaid expansion demonstration program. We also supported the Iowa Department of Health and Human services in developing the Iowa Health and Wellness Plan (IHAWP) 1115 demonstration which provides an alternative benefit design to traditional Medicaid expansion. HMA also supported the Kentucky Cabinet for Health & Family Services (CHFS) with a variety of services related to its section 1115 demonstration, Kentucky HEALTH, the first community engagement program in the nation approved by CMS.

Health Management Associates (HMA) is pleased to congratulate Caprice Knapp, PhD, as she departs our organization to serve as Medicaid Counselor to U.S. Health and Human Services (HHS) Secretary Robert F. Kennedy, Jr. At HMA, Knapp served as managing director of the Quality and Accreditation practice group.
As Medicaid Counselor, Knapp will work closely with the White House and the Centers for Medicare and Medicaid Services to coordinate Medicaid strategy and policy. She begins her new role on April 28.
“This is an incredible opportunity to improve the health and well-being of Americans and ensure Medicaid recipients are always at the center of those efforts. While I have loved my time at HMA, I feel called to return to public service in this impactful role,” Knapp said.
A former member of the Congressional Budget Office’s Panel of Health Advisers, Knapp is a health economist with more than 20 years’ experience working on Medicaid and the Children’s Health Insurance Program (CHIP). She previously served as North Dakota’s Medicaid director and as a Robert Wood Johnson health policy fellow on the Energy and Commerce Committee of the U.S. House of Representatives.
“Caprice has been a tremendous leader at HMA, and like our diverse team of experts, a trusted advisor for clients tackling tough challenges to improve the health and wellness of individuals and communities alike,” said HMA CEO Chuck Milligan. “The Medicaid Counselor will play a vital role in moving the program and health of our country forward – something Caprice is uniquely equipped to do. We are grateful for her many contributions and wish her the best.”

New HMA Report Provides Insights on Strengthening State Medicaid NEMT Contracts

Amy Bassano is a Managing Director at Health Management Associates and a nationally recognized Medicare policy expert. In this episode of Vital Viewpoints on Healthcare, we unpack the complexities of Medicare innovation and examine where the program is headed next. Drawing on decades of experience—including her leadership at the Center for Medicare and Medicaid Innovation—Amy breaks down what makes value-based care so complex, why scaling successful models is harder than it sounds, and how Medicare Advantage continues to reshape the healthcare landscape. She also discusses how financial incentives, regulatory constraints, and the urgent need for system-wide efficiency are shaping the next chapter of Medicare policy. This conversation offers practical insights for policymakers, providers, and advocates navigating the future of one of the nation’s most essential programs.

Federal statute requires states to provide non-emergency medical transportation (NEMT) to Medicaid beneficiaries who have no other means of getting to medically necessary healthcare facilities. Though NEMT programs must meet certain federal requirements, states have considerable flexibility in the design and operation of their NEMT program. As a result, states vary widely in their NEMT procurement and contract standards, metrics, reporting, and enforcement of requirements for NEMT brokers, MCOs, and transportation providers. Health Management Associates, Inc. (HMA), examined NEMT-related requests for proposals (RFPs) and contracts for five states and interviewed state Medicaid officials, transportation brokers and providers, MCOs, advocates, and subject matter experts (SMEs). The goal was to synthesize the information gathered to help inform states and other stakeholders about key NEMT standards, challenges and successes, and considerations for developing RFPs and contracts.

This week, our second In Focus article addresses the transition to end the Medicare Advantage Value-Based Insurance Design (VBID) model, which launched in 2017 and subsequently has been expanded with bipartisan support. This model was designed to promote flexible benefit design, reduce cost barriers, and enhance care for targeted populations, especially dual eligibles and individuals with chronic conditions. In December 2024, however, the Centers for Medicare & Medicaid Services (CMS) announced that the model would be terminated by the end of 2025, citing unmitigable costs to the Medicare Trust Funds, totaling more than $4.5 billion across 2021 and 2022 alone.
Despite its popularity and effectiveness in improving medication adherence and addressing social determinants of health, CMS concluded that the cost trajectory was unsustainable within the parameters of the Innovation Center’s mandate.
The end of the VBID model is not the end of innovation in Medicare Advantage (MA); rather, it is a strategic inflection point. Plans that approach this transition with a proactive, data-driven lens will be best positioned to maintain competitive advantage, compliance, and member trust. This article reviews critical steps VBID plans should be taking and how Medicare Advantage Organizations (MAOs) and their partners can best prepare for future opportunities.
Pain Points and Key Strategic Decisions for MAOs
As plans prepare for a post-VBID world, they face a series of complex trade-offs—especially those with Dual Eligible Special Needs Plans (D-SNPs) that had $0 drug cost sharing under VBID. With the end of CMS’s drug cost offset in the initial coverage phase, MAOs will need to determine whether and how to absorb those costs through alternative mechanisms. In addition, plans will need to make important decisions regarding their other VBID benefits, namely, whether to discontinue or transition them to the special supplemental benefits for the chronically ill (SSBCI) program. MAOs should consider the following key strategic decisions:
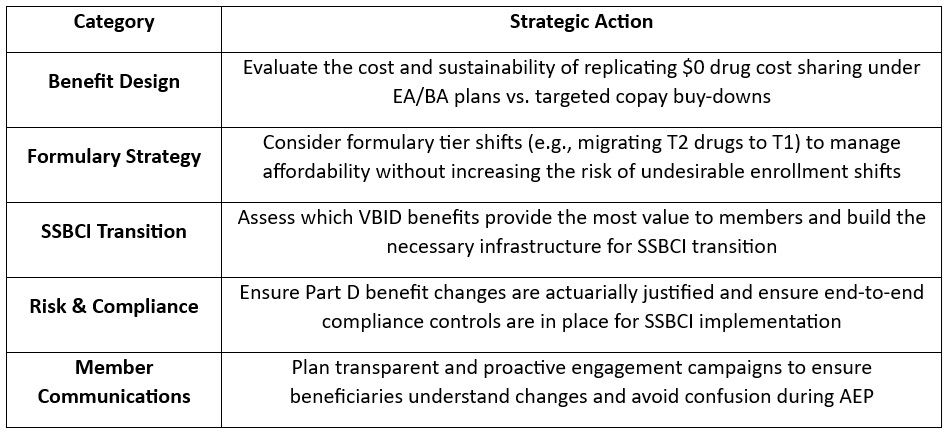
Action Plan: What MAOs Should Be Doing Now
To navigate this transition successfully, teams of experts at Wakely, a Health Management Associates, Inc. (HMA) Company, are already working with VBID stakeholders to evaluate multiple transition scenarios. Our experts recommend that MAOs take the following actions:
What to Watch: Future Innovation in Medicare Advantage
Though VBID is ending, the innovation landscape is far from static. With the new Trump Administration and the return of Abe Sutton—a VBID expansion advocate—appointed as Director of the CMS Innovation Center, our experts are closely monitoring the potential for a revised version of VBID or similar models. Stakeholder advocacy could influence how CMS prioritizes the next wave of innovation. Plans should consider engaging in dialogue now to shape what happens next.
Connect with Us
Wakely is embedded in MA strategy and policy. Wakely and HMA teams are working with clients to evaluate multiple transition scenarios, helping them optimize value, protect Star Ratings, and preserve member satisfaction during this pivotal shift, while also supporting targeted policy engagement efforts to ensure their perspectives are reflected in future CMS and Innovation Center decision making.
Our joint capabilities bring together:
To connect on additional questions contact our featured experts below.

This week, our In Focus section reviews the policy changes that the Centers for Medicare & Medicaid Services (CMS) proposes to make in the Fiscal Year (FY) 2026 Medicare Hospital Inpatient Prospective Payment System (IPPS) and Long-Term Acute Care Hospital (LTCH) Proposed Rule (CMS-1833-P). The IPPS proposed rule, released April 11, 2025, includes several important policy changes that will alter hospital margins and change administrative procedures, beginning as soon as October 1, 2025.
Key Provisions of the FY 2026 Hospital IPPS and LTCH Proposed Rule
For FY 2026, CMS proposes to modify several hospital inpatient payment policies. We highlight and interpret six of these proposed policies that may be among the most impactful for Medicare beneficiaries, hospitals and health systems, payers, and manufacturers, as follows:
Annual Inpatient Market Basket Update
Proposed Rule: CMS’s FY 2026 Medicare IPPS Proposed Rule will increase payments to acute care hospitals overall by 2.4 percent from FY 2025, amounting to an estimated $4 billion increase in reimbursement. This update is based on a hospital market basket increase of 3.2 percent and a 0.8 percent reduction for total factor productivity.
HMA Analysis: CMS’s 2.4 percent increase results from the estimated rate of increase in the cost of a standard basket of hospital goods—the hospital market basket. For beneficiaries, this payment increase will lead to a slightly higher standard Medicare inpatient deductible and an increase in out-of-pocket costs. For hospitals and health systems, payers, and manufacturers, the proposed payment increase (2.4 percent) is consistent with economy-wide inflation over the past year (2.4 percent) and below the amount that MA plans will receive for 2026 (5 percent).[1], [2] Although the published payment update for FY 2026 is 2.4 percent, other policy changes result in the average change in inpatient payments totaling slightly more than 3 percent. We anticipate the proposed 2.4 percent increase will increase somewhat by the time CMS finalizes these rates later in the year.
Labor Share Reduction
Proposed Rule: CMS proposes to modify the hospital labor share used to reimburse hospitals for inpatient services. Using 2023 hospital cost report data CMS proposed a national labor‑related share of 66.0 percent, a decrease from the labor share of 67.6 percent.
HMA Analysis: Every five years, CMS recalculates the hospital market basket and the hospital labor share using updated cost data from the hospital cost reports. For FY 2026, CMS conducted its routine rebasing calculation using 2023 cost report data, replacing the 2018 cost data currently used. As a result, CMS calculated that the cost of labor accounts for a slightly smaller share of total hospital costs in 2023 than in 2018. The labor share is used within the IPPS to identify the proportion of payments that are affected by the hospital wage index in an effort to adjust payments for geographic variation in labor costs. The consequence of a lower hospital labor share is that a slightly smaller share of hospital inpatient payments will be adjusted by the hospital wage index. The subtle impact of this change is that hospitals with higher wage index values may experience reductions in payment. Further, this downward revision of the labor share signals that hospital wages, salaries, and employee benefits account for a smaller share of total costs in the post-pandemic environment. This change may come to a surprise to some, as hospital labor costs have been a subject of concern since the COVID-19 public health emergency.
Medicare Advantage Data Integration in Measuring Hospital Readmissions
Proposed Rule: CMS proposed to make several modifications to the Hospital Readmissions Reduction Program (HRRP), including:
CMS also proposed to include MA data in other measures included in the Hospital Value-Based Purchasing (VBP) program and the Inpatient Quality Reporting (IQR) program.
HMA Analysis: The inclusion of MA data in the HRRP may have significant payment implications for many hospitals because it will alter their readmission rates in unanticipated ways, particularly if hospitals’ MA patients differ substantially from traditional Medicare beneficiaries. Importantly, the inclusion of MA data in the HRRP measures, and also within the VBP program and the IQR program, signals that CMS is moving toward broader integration of MA data into Medicare fee-for-service reimbursement systems.
New Technology Add-on Payment Program Growth
Proposed Rule: CMS proposed to continue NTAP status for 26 products because they continue to meet the newness criteria required under this program. In addition, within the proposed rule CMS discusses new NTAP applications for 43 additional products. Among these applications, 29 were submitted under the alternative pathways for breakthrough devices and qualified infectious disease products (QIDP).
HMA Analysis: The overall number of products with NTAPs is on par with other recent years, but the number of NTAP applications has blossomed in FY 2026 as the result of the alternative breakthrough application pathway. This alternative pathway allows breakthrough devices and certain antibiotic and antimicrobial drugs to apply for NTAP using an abbreviated application process.
Transforming Episode Accountability Model Modifications
Proposed Rule: CMS proposed several modifications to the forthcoming CMS Innovation Center TEAM framework. Among the various methodological modifications proposed to this mandatory payment model beginning January 1, 2026, CMS proposed to take the following actions:
HMA Analysis: The critical aspect of CMS’s TEAM provision is that the agency proposes to follow through with this Innovation Center model while cancelling other Innovation Center payment models in recent months. It also is noteworthy that the agency has proposed to remove the health equity data reporting requirements for TEAM in line with actions taken with many other CMS programs. Another proposal of note is the plan to expand the use of the waiver to circumvent the SNF three-day inpatient stay rule, which will allow hospitals to discharge patients more quickly to SNFs.
Uncompensated Care Payment Increase for Disproportionate Share Hospitals
Proposed Rule: CMS proposes to increase uncompensated care payments to DSHs by $1.5 billion in FY 2026.
HMA Analysis: CMS’s proposal will increase uncompensated care payments to hospitals by 26 percent. This increase is driven by CMS’s assumption that the rate of uninsured people will increase to 8.7 percent of the population in 2026 from 7.7 percent in 2025.
Stakeholder comments on the IPPS proposed rule are due no later than June 10, 2025.
Connect With Us
The Health Management Associates, Inc. (HMA), Medicare Practice Group monitors federal regulatory and legislative developments in the inpatient setting and assesses the impact on hospitals, life science companies, and other stakeholders. Our experts interpret and model hospital payment policies and assist clients in developing CMS comment letters and long-term strategic plans. Our team replicates CMS payment methodologies and model alternative policies using the most current Medicare fee-for-service and Medicare Advantage (100%) claims data. We also support clients with DRG reassignment requests, NTAP applications, and analyses of Innovation Center alternative payment models.
For more information about the proposed policies, please contact our expert below.
[1] U.S. Bureau of Labor Statistics. Table 1. Consumer Price Index for All Urban Consumers (CPI-U): U.S. City Average, by Expenditure Category. Modified April 10, 2025. Available at: https://www.bls.gov/news.release/cpi.t01.htm.
[2] Centers for Medicare & Medicaid Services. 2026 Medicare Advantage and Part D Rate Announcement. April 7, 2025. Available at: https://www.cms.gov/newsroom/fact-sheets/2026-medicare-advantage-and-part-d-rate-announcement.

FY 2026 Medicare Hospital Inpatient Proposed Regulation Signals Several Changes Lie Ahead for the Hospital Industry and Beneficiaries