HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- CMS Takes Next Major Step in Medicare Drug Price Negotiation Program

- Medicaid Eligibility Redeterminations News: Alaska, Illinois, Maine, Massachusetts

- Georgia Looks to Increase Oversight of Medicaid Plans

- Idaho Gears Up for Transition to Single Behavioral Health Plan Covering Inpatient, Outpatient Services

- Indiana Medicaid Beneficiaries Struggle to Access Dental Care

- Iowa Increases Medicaid Reimbursements for Substance Abuse, Mental Health Counseling

- Michigan Governor to Call for Legislation Locking in ACA Protections

- Nevada Awards Magellan Contract for Complex Behavioral Care Management for Youths

- North Carolina Medicaid Expansion Will No Longer Launch on October 1

- Oklahoma Proposes 12 Months of Continuous Eligibility for Children on Medicaid, CHIP

- CMS Takes Additional Action to Halt Wrongful Medicaid Disenrollments

- Centene to Sell Circle Health Group to PureHealth

In Focus
CMS Takes Next Major Step in Medicare Drug Price Negotiation Program
This week’s In Focus centers on the U.S. Department of Health and Human Services (HHS) August 29, 2023, announcement of the first 10 prescription medications that will be subject to price negotiation for Medicare coverage. This week, Health Management Association (HMA) experts offer their perspective on what this change means and what to expect next.
Background
Medicare was granted the authority to negotiate prescription drug prices through the Inflation Reduction Act (IRA), which the president signed into law on August 16, 2022. HHS, acting through the Centers for Medicare & Medicaid Services (CMS), will lead negotiations and enter into agreements with manufacturers for these products, negotiating a maximum fair price (MFP) for each selected drug in the Medicare program. HHS is required to negotiate on a certain number of drugs each year: 10 drugs in 2026, 15 drugs in 2027 and 2028, and 20 drugs in 2029 and subsequent years. Up to 60 drugs could be negotiated by 2029. Manufacturers that are noncompliant will face an excise tax that could far exceed the cost of drugs sold over time and civil monetary penalties.
Medicare Drug Negotiations: The Latest Development
Since passage of the IRA, CMS has been working to establish the regulatory infrastructure and policies to support implementation of Medicare’s new drug price negotiation authority on an expedited timeline. Guidance on the approach the agency will take in negotiating MFPs, along with other provisions of the act, has been issued.
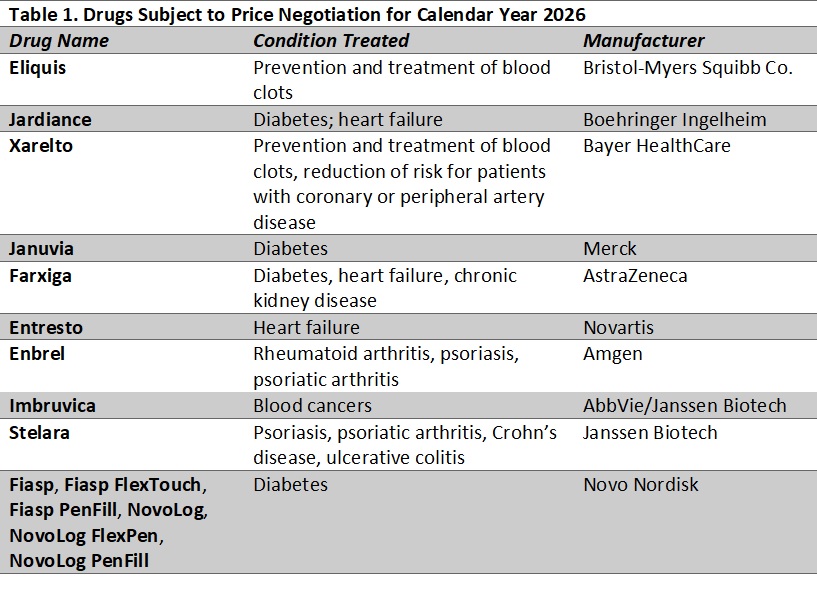
With this week’s action, CMS will begin the first round of negotiations. Table 1 lists the drugs CMS has identified for the first round of negotiations. Products selected for negotiation (with prices effective in 2026) are medications that represent the highest spending in the Part D drug benefit, excluding products with generic or biosimilar competition as well as certain orphan drugs and other products that qualify for a small biotechnology exemption.
Alongside CMS’s announcement, HHS’s Office of the Assistant Secretary for Planning and Evaluation (ASPE) released its analysis of prescription drug use and out-of-pocket spending for each of the 10 drugs for all Part D enrollees and separately by whether an enrollee receives the low-income subsidy (LIS). The report also examines demographic information about enrollees who use the selected products.
Takeaways
The products selected were largely in line with initial modeling that Moran Company analysts and others performed, but with some surprises. Variation from earlier projections could be expected for a number of reasons, including:
- The June 2022−May 2023 data CMS used were not generally available to outside analysts, and it is clear that several products had spending increases (whether because of volume or price increases) relative to prior years that moved them up the list.
- Some higher spending products have seen generic or biosimilar competitors launch, making them ineligible for selection for negotiation.
- For the top 30 products identified in previous dashboard data, at least 10 have evidence of generic or biosimilar competition.
- CMS’s decision to treat multiple products together for purposes of negotiations also affected the products included on the list.
- For a few other products, it is still unclear how CMS decisions were made.
What to Expect Next
The drug negotiation policy is highly controversial and is the subject of litigation that could delay the process. If litigation does not affect the timeline for implementation, manufacturers of selected drugs have until October 1 to agree to negotiate and provide initial information to CMS. If a manufacturer opts out of the negotiations, the company must pay either an excise tax or withdraw all its products from the Medicare and Medicaid programs. CMS and participating companies will then meet to discuss manufacturer submissions, and CMS will receive information from other stakeholders. Several listening sessions will take place.
CMS will make initial price offers by February 1, 2024. After a counteroffer process, negotiations may continue into the summer of 2024, but final determinations will be made by August 1, 2024. CMS plans to publish any agreed-upon negotiated prices for the selected drugs by September 1, 2024. Those prices take effect starting January 1, 2026.
In addition to the short-term impact on prices for specific drugs, several questions about the potential effects of the policy are worth monitoring over the long-term:
- How will research and development of new products and trends in the type of products prioritized change as a result of these policies?
- How will the policies affect pricing for competitor products and the launch prices of products in the future?
- Beyond the Medicare population, for whom the prices are directly applicable, how will MFPs affect negotiations on costs and supplemental rebates for other payers. including state Medicaid programs, state employee programs, drug purchasing pools, and commercial insurers?
- Will negotiations affect the design of standalone Prescription Drug Plans (PDPs) and Medicare Advantage PDPs.
The IRA included several other changes to the Medicare program, which we discussed in a previous In Focus.
HMA Roundup
Alaska
Alaska Medicaid Enrollment Is Down 14,398 Since April. Anchorage Daily News reported on August 23, 2023, that Alaska Medicaid enrollment is down 14,398 from 264,649 when eligibility redeterminations resumed in April to 250,251 in July. About a third of coverage losses from redeterminations were for procedural reasons, a rate that federal regulars say may indicate people are not getting notices, understanding them, or submitting forms. Read More
Arkansas
Arkansas Redirects Additional Funds to Crisis Stabilization Units. The Arkansas Department of Human Services (DHS) announced on August 29, 2023, that the state will redirect $1 million in Substance Abuse and Mental Health Services Administration (SAMHSA) grant money to support the state’s four crisis stabilization units (CSUs). CSUs must submit a plan to DHS showing they will be able to sustain operations once grant funding ends on June 30, 2024. Read More
Assisted Living Facilities Receive Majority of Federal COVID Relief Funds. The Arkansas Advocate reported on August 28, 2023, that the Arkansas Department of Human Services (DHS) distributed most of the $2 million it received in federal COVID-19 relief funds to assisted living facilities participating in the state’s Medicaid program through the Living Choices Assisted Living Waiver. The waiver targets seniors and adults at risk of nursing home admission. Funds were allocated based on the average number of Medicaid beds used in each between fiscal 2019 and 2023. Read More
Colorado
Colorado Selects Safety Net Connect to Implement Medicaid eConsult Platform. Safety Net Connect announced on August 29, 2023, that it has been selected by the Colorado Department of Health Care Policy & Financing for its eConsult platform, aimed at facilitating electronic communication between Medicaid primary care providers and specialists. Read More
California
California Grants Zero-Interest Loans To 17 Community Hospitals. Modern Healthcare reported on August 25, 2023, that the California Distressed Hospital Loan Program is offering about $300 million in interest-free loans to 17 hospitals in the state. Madera Community Hospital, which filed for Chapter 11 bankruptcy protection, located in rural California, has been offered up to $52 million. Adventist Health has agreed to manage Madera if it reopens. Read More
Georgia
Georgia Looks to Increase Oversight of Medicaid Plans. Capitol Beat News Service reported on August 24, 2023, that the Georgia Department of Community Health (DCH) is seeking $7.2 million in its fiscal 2024 mid-year budget request to improve oversight of Medicaid managed care plans in the state. The majority of funds would go toward adding 49 staffers, including individuals to help with the state’s upcoming Medicaid managed care procurement. Governor Brian Kemp will present budget recommendations to the General Assembly in January. Read More
Idaho
Idaho Gears Up for Transition to Single Behavioral Health Plan Covering Inpatient, Outpatient Services. Big Country News reported on August 28, 2023, that Idaho is gearing up for the March 2024 transition to a single, comprehensive behavioral health plan covering both inpatient and outpatient services, a contract the state awarded to Magellan Health. Prior behavioral plan Optum, covering outpatient behavioral health services, has filed a lawsuit disputing the contract award.
Illinois
Illinois Works to Improve Productivity of Medicaid Redeterminations Call Centers. Health News Illinois reported on August 28, 2023, that Illinois state officials are working to increase the productivity of call centers aiding individuals going through the Medicaid eligibility redetermination process. Efforts by the Department of Healthcare and Family Services and the Department of Human Services include making one phone number the primary source of redeterminations information. Read More
Illinois to Expand Mental Telehealth Pilot Program to Rural Farmers Statewide. Health News Illinois reported on August 30, 2023, that a pilot program providing mental telehealth services to rural farmers will now be available statewide, offering six free telehealth sessions. The pilot was initially available in six counties. Illinois Governor JB Pritzker announced grant funding of up to $1,000 to chapters of the Illinois FFA Foundation to increase mental health awareness and services in schools and communities. Read More
Illinois Hospital to Receive $800,000 in Federal Funds for Neonatal Intensive Care Unit. Health News Illinois reported on August 30, 2023, that Illinois’s Cook County Health/John H. Stroger, Jr. Hospital will receive more than $800,000 in federal grants funds for the neonatal intensive care unit. Funds will go toward the purchase of incubators, infant warmers and critical care equipment. Read More
Indiana
Indiana Medicaid Beneficiaries Struggle to Access Dental Care. The Indianapolis Star reported on August 24, 2023, that Indiana Medicaid beneficiaries struggle to access dental care, driven by a shortage of dentists willing to accept the state Medicaid program’s reimbursement rates. Read More
Iowa
Iowa Increases Medicaid Reimbursements for Substance Abuse, Mental Health Counseling. Radio Iowa reported on August 24, 2023, that the Iowa legislature approved a $13 million increase in Medicaid reimbursement rates for substance abuse counseling and mental health services. The increase in rates for mental health counseling is 18 percent. Read More
Maine
Maine Disenrolls 1,642 Medicaid Beneficiaries During July Redeterminations. The Maine Department of Health and Human Services (DHHS) announced on August 25, 2023, the disenrollment of 1,642 Medicaid beneficiaries during July redeterminations. Of the 33,196 MaineCare members up for renewal during that period, coverage was renewed for 11,210 individuals. The remaining renewals were not yet completed. Read More
Massachusetts
Massachusetts Disenrolls More Than 60,000 Medicaid Beneficiaries During July Redeterminations. WBUR reported on August 24, 2023, that Massachusetts has disenrolled more than 60,000 Medicaid beneficiaries during July redeterminations. Cumulative disenrollment since April is 127,000. All told, enrollment in the state’s Medicaid and Children’s Health Insurance Program was 2.39 million in July, down 0.6 percent from 2.4 million on April 1 when redeterminations began in Massachusetts. Read More
Michigan
Michigan Governor to Call for Legislation Locking in ACA Protections. The Associated Press reported on August 28, 2023, that Michigan Governor Gretchen Whitmer is expected to ask lawmakers to approve legislation locking in certain Affordable Care Act protections, including no-cost preventive care, essential benefits, and ensuring coverage despite an individual’s preexisting conditions. Read More
FQHCs Receive $500,000 in Grants from UnitedHealthcare. UnitedHealthcare Community Plan of Michigan announced on August 23, 2023, that it has awarded $500,000 in grants of $100,000 each to five federally qualified health centers (FQHCs) to expand access to behavioral health services. FQHC awards went to Cherry Health, Family Health Center, Great Lakes Bay Health Centers, InterCare Community Health Network and MidMichigan Community Health Services. Read More
Nevada
Nevada Awards Magellan Healthcare Contract to Administer Complex Behavioral Care Management for Youths. Magellan Health announced on August 29, 2023, that it was awarded the capitated contract to administer care management for individuals in Nevada aged three to 20 with complex behavioral health needs. The program will focus on individuals who are at risk for placement outside of their homes or communities. Read More
New York
New York Announces Additional Initiatives to Improve Maternal, Newborn Health. The New York State Department of Health announced on August 24, 2023, various initiatives targeted at improving maternal and newborn health, including doula coverage, midwifery services, updated perinatal care standards, remote patient monitoring, prenatal and postnatal community health worker coverage, nutrition and lactation counseling, and prenatal testing. The initiatives were exacted as part of the state’s 2024 budget. Read More
Lawmakers, Advocates Raise Concerns over Proposed Medicaid Reimbursement Rates for Doulas. Crain’s New York Business reported on August 24, 2023, that New York lawmakers and advocates question whether the state’s proposed Medicaid reimbursement rates for doulas are high enough to encourage participation in the program. Proposed 2024 doula rates of $1,350 per pregnancy upstate and $1,500 downstate await approval from the Centers for Medicare & Medicaid Services. Read More
North Carolina
Medicaid Expansion Will No Longer Launch on October 1. The North Carolina Department of Health and Human Services (DHHS) announced on August 28, 2023, that Medicaid expansion will not launch as planned on October 1, due to continued budget negotiations in the state legislature. A new launch date has not been determined. Read More
Oklahoma
Oklahoma Forms Medicaid Delivery System Quality Advisory Committee. The Oklahoma Health Care Authority (OHCA) announced on August 28, 2023, that it has formed a Medicaid Delivery System Quality Advisory Committee to address oversight, evaluate performance, and make recommendations for SoonerSelect Medicaid managed care plans. The 19 committee members include providers, community members, academics. Read More
Oklahoma Proposes 12 Months of Continuous Eligibility for Children on Medicaid, CHIP. The Oklahoma Health Care Authority proposed on August 22, 2023, a 12-month period of continuous eligibility for children on Medicaid and CHIP, effective January 1, 2024. The public comment period will be open until September 8, 2023. Read More
National
CMS Issues Final Rule for Medicaid, CHIP Quality Measures Reporting. The Centers for Medicare & Medicaid Services (CMS) released on August 28, 2023, a final rule to require reporting of standardized quality measures in Medicaid and the Children’s Health Insurance Program (CHIP). The rule requires mandatory annual state reporting on three different quality measure sets, including child and adult core sets, health home core sets, and behavioral health core sets. The rule will begin in fiscal 2024. Read More
CMS Takes Additional Action to Halt Wrongful Medicaid Disenrollments. The Centers for Medicaid & Medicare Services (CMS) urged states on August 30, 2023, to identify eligibility redetermination systems issues that may be causing beneficiaries to be wrongfully disenrolled from Medicaid and the Children’s Health Insurance Program (CHIP). CMS said that “eligibility systems in a number of states are programmed incorrectly and are conducting automatic renewals at the family-level and not the individual-level.” States that CMS identified to need immediate action must pause procedural disenrollments and reinstate coverage for affected individuals, implement one or more CMS-approved mitigation strategies, and fix state systems and processes to ensure renewals are conducted appropriately. Read More
Medicare Shared Savings Program Saves $1.8 Billion in 2022, CMS Says. The Centers for Medicare & Medicaid Services (CMS) announced on August 24, 2023, that the Medicare Shared Savings Program saved $1.8 billion in 2022, compared to spending targets. This is the sixth consecutive year that the program has generated overall Medicare savings, according to CMS. Read More
HHS OIG Releases Medicare, Medicaid Managed Care Oversight Plan. The Department of Health and Human Services (HHS) Office of Inspector General (OIG) released on August 28, 2023, a strategic plan aimed at improving oversight of Medicaid managed care and Medicare Advantage plans. The initiative would include audits, evaluations, investigation, financial oversight, and efforts to broaden access and encourage data accuracy and use. Read More
Medicaid Unwinding Could Double Uninsured Rate Among Children. CNN reported on August 26, 2023, that 6.7 million children are at risk of losing Medicaid coverage during the unwinding process, according to Georgetown University’s Center for Children and Families. Among the 15 states that release coverage losses by age, at least 1.1 million kids have been disenrolled between April and the end of July, according to KFF. Read More
CMS Study Undermines Rationale for Nursing Home Staffing Mandate. KFF Health News reported on August 29, 2023, that the Centers for Medicare & Medicaid Services (CMS) commissioned a study that undermines a Biden administration plan to require minimum staffing levels at nursing homes. The study maintains that no single staffing level guarantees high quality care. Read More
Industry News
Centene to Sell Circle Health Group to PureHealth. Centene Corporation announced on August 28, 2023, that it signed a definitive agreement to sell U.K. independent hospital operator Circle Health Group to PureHealth for about $1.2 billion, including assumption of debt. PureHealth is an integrated healthcare network in the Middle East. The transaction is expected to close in the first quarter of 2024. Read More
New Story Acquires Virginia Assets of Center for Autism & Related Disorder. Special education and client provider New Story announced on August 25, 2023, the acquisition of the Virginia assets of the Center for Autism & Related Disorder, including three school campuses and nine Applied Behavior Analysis (ABA) therapy clinics. The campuses will transition to Rivermont Schools, and clinics will transition to Your Life ABA clinics. New Story now operates in seven states and serves 3,800 students. Read More
Cigna Exits Kansas, Missouri Insurance Exchanges for 2024. Fierce Healthcare reported on August 28, 2023, that Cigna will no longer offer Exchange coverage in Kansas and Missouri for 2024. Cigna will also exit two counties in Arizona and two in Utah. Cigna is expanding into 15 additional counties in North Carolina. Cigna intends to offer plans in 350 counties for 2024, compared to 363 in 2023. Read More
Humana Subsidiary CenterWell to Introduce Home Health Care in Georgia, Louisiana. Health Payer Specialist reported on August 30, 2023, that Humana subsidiary CenterWell Senior Primary Care will introduce in-home, primary care for Medicare Advantage and traditional Medicare members in Louisiana and Georgia. The launch leverages the company’s 2023 acquisition of Heal and will allow patients to receive routine care such as blood draws, vaccinations, and prescription management at home. Read More
RFP Calendar

HMA News & Events
Upcoming HMA Webinar:
Medicare Policy Changes Impacting Behavioral Health Services Workforce and Population Health. With recent rule changes proposed by the Centers for Medicare and Medicaid Services (CMS) addressing expanding access to behavioral health services, this webinar will focus on how those changes will impact the already strained workforce, and corresponding impacts on population health. HMA Experts will dive deeper into approaches to handle workforce shortages while expanding access. Tuesday, September 12, 12pm ET. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Indiana Medicaid Managed Care Enrollment Is Up 3.3%, Apr-23 Data
- Michigan Medicaid Managed Care Enrollment is Up 1.4%, May-23 Data
- Michigan Dual Demo Enrollment is Down 0.8%, May-23 Data
- Pennsylvania Medicaid LTSS Enrollment is Up 2.7%, Jun-23 Data
- West Virginia Medicaid Managed Care Enrollment is Down 2.1%, May-23 Data
- West Virginia Medicaid Managed Care Enrollment is Up 2.1%, Apr-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Arizona Long Term Care System RFP and Q&A, Aug-23
- Michigan State Medicaid Agency Contract (SMAC) D-SNP Contracts, 2024
- Pennsylvania HealthChoices Physical Health Model Contract, 2020-23
Medicaid Program Reports, Data, and Updates:
- Alaska Medicaid Enrollment Dashboard, Jul-23
- Connecticut Medical Assistance Program Oversight Council Meeting Materials, Jul-23
- District of Columbia Medicaid Managed Care Annual Technical Reports, 2014-22
- District of Columbia Medical Care Advisory Committee Meeting Materials, 2021-23
- District of Columbia Mental Health and Substance Abuse Expenditures and Service Utilization Reports, 2017-22
- Idaho Medicaid Procurement Schedule, Aug-23
- Maine PHE Medicaid Redeterminations Monthly Report to CMS, Jul-23
- Massachusetts Medicaid Care Management Quality Performance Report, 2018-22
- MassHealth Medical Care Advisory Council Meeting Materials, Mar-23
- Pennsylvania HealthChoices Behavioral Health Enrollment Map by County and BH MCO, Jun-23
- Pennsylvania Behavioral Health External Quality Review Reports, 2022
- Pennsylvania HealthChoices HEDIS Performance Measures Rate Charts, 2015-21
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
