HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- Virginia Releases Cardinal Care Medicaid Managed Care RFP

- California Medi-Cal Contracts Are Scheduled to Begin January 1

- PBMs Face Lawsuit from Los Angeles County Over Opioid Crisis

- Georgia Receives Approval of Waivers to Streamline Medicaid Unwinding Process

- Montana Medicaid Providers Face Further Delay in Receiving Increased Rates

- New York Managed Long-term Care Plan Is Closing Down

- Oregon to Step Up PBM Regulation After Audit Finds Lax Oversight

- Pennsylvania Senate Passes Bill to Raise Reimbursement Rate for Ambulance Services

- Tennessee Awards Findhelp Contract to Connect Medicaid Beneficiaries with Social Services

- West Virginia Receives CMS Approval for Medicaid Mobile Crisis State Plan Amendment

- CMS to Provide Funding to Help States Implement AHEAD Total Cost of Care Delivery System Model

- Molina Acquires My Choice Wisconsin

In Focus
Virginia Releases Cardinal Care Medicaid Managed Care RFP
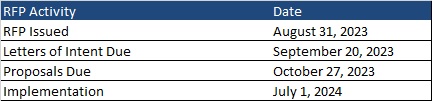
This week, our In Focus section reviews the request for proposals (RFP) for the Virginia Cardinal Care Medicaid managed care program, released by the Department of Medical Assistance Services (DMAS) on August 31, 2023. The RFP includes a new foster care specialty plan. Implementation is scheduled to begin July 1, 2024.
Cardinal Care
Cardinal Care launched in January 2023 as a rebranding of the state’s Medicaid program and Children’s Health Insurance Program—Family Access to Medical Insurance Security Plan (FAMIS). Cardinal Care Managed Care (CCMC) will combine the state’s existing Medallion 4.0 managed care program for traditional Medicaid and the Commonwealth Coordinated Care Plus (CCC Plus) managed long-term services and supports (MLTSS) program to serve 1.9 million Medicaid managed care members.
RFP
The state will award statewide fully capitated, risk-based contracts to a maximum of five health plans. A separate foster care specialty plan contract will also be awarded to one of the winners. If none of the plans win the separate foster care specialty program, all plans awarded a CCMC contract will be required to cover all services.
Selected plans will provide acute care, behavioral health, and MLTSS services to all Virginians who are eligible for Medicaid, including children, adults, and pregnant women in low-income households; children and adults with disabilities; low-income older adults; and individuals receiving LTSS, including dual-eligible populations. The foster care plan will cover children in foster care, individuals younger than 26 years old who were formerly in foster care, and children eligible for adoption assistance.
The RFP contains several targeted focus areas and changes to the managed care program. For example, it emphasizes improvements to the state’s behavioral health care system and improved health outcomes through a focus on health-related social needs such as housing stability and food insecurity for CCMC members.
Contracted plans will be required to operate a dual-eligible special needs plan (DSNP) in Virginia.
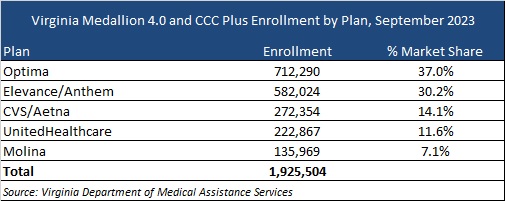
Market
CVS/Aetna, Elevance/Anthem, Sentara/Optima Health, Molina, and UnitedHealthcare are the current incumbents. Effective with the new RFP, DMAS intends to reassign most CCMC members as part of an enrollment process. At present, Optima holds the largest market share of enrollment at 37 percent, followed by Anthem at 30 percent.
Timeline
Letters of intent are due by September 20 and proposals are due on October 27. As previously mentioned, new contracts will begin July 1, 2024. Contracts will have a six-year initial term, with two two-year renewal options. Award dates have not been announced.
Evaluation
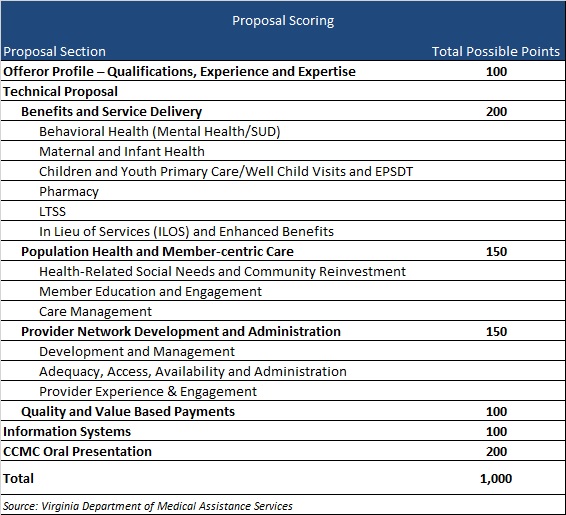
Plans will be awarded up to 1,000 points during the evaluation process based on the categories shown below.
HMA Roundup
Arizona
Arizona Includes Community Feedback in Parents as Paid Caregivers Final Proposal. The Arizona Health Care Cost Containment System (AHCCCS) announced on September 5, 2023, that it has incorporated community feedback into its waiver proposal to extend Medicaid payments to parents who provide caregiver services to children under age 18 with disabilities. The proposal, which will be submitted for federal approval, seeks to include the addition of habilitation services; ensuring timely access to care; extending additional home and community support services; and allowing parents to receive Medicaid reimbursements for providing caregiver services to their minor children. A public forum to review the final federal proposal will be held on September 6, 2023. Read More
Arizona Releases Updates to Medicaid Claims Payment System, Provider Enrollment Process. The Arizona Health Care Cost Containment System (AHCCCS) released on September 1, 2023, changes to its Medicaid claims payment system and provider/member enrollment processes. The changes, which are aimed at ending fraudulent behavioral health billing, include requiring behavioral health providers to submit additional documentation; ensuring providers under investigation help members transition to new providers; and ensuring Native American/Alaskan Native individuals are allowed to choose AHCCCS’ American Indian Health Program as their health plan. Read More
California
Medi-Cal Contracts Are Scheduled to Begin January 1. The Department of Health Care Services (DHCS) announced on September 2, 2023, that all Medi-Cal managed care plan (MCP) contracts awarded last year will go live as scheduled on January 1, 2024. After conducting “go-live” assessments, DHCS gave the green light to Kaiser Foundation Health Plan, Anthem Blue Cross, Partnership HealthPlan of California, Community Health Plan of Imperial Valley, and Molina Healthcare. Read More
PBMs Face Lawsuit from Los Angeles County Over Opioid Crisis. The Los Angeles Times reported on September 5, 2023, that Los Angeles County has filed a lawsuit in state superior court alleging that pharmacy benefit managers (PBMs) Express Scripts and UnitedHealth/OptumRx contributed to the opioid epidemic by promoting use of the drugs despite evidence of rising abuse. Similar suits have been filed against PBMs in Ohio, Texas, and Virginia. Read More
Georgia
Georgia Receives Approval of Waivers to Streamline Medicaid Unwinding Process. The Georgia Department of Community Health announced on September 6, 2023, that it has received federal approval to use seven waivers to help streamline the Medicaid Unwinding process. The approved waivers include Targeted SNAP Strategy; Targeted TANF Strategy; Beneficiaries with No Income Renewal; Streamlined Asset Verification; MCO Beneficiary Contact Updates; NCOA and/or USPS Contact Updates; and Fair Hearing Timeframe Extension. Georgia has already used the waivers to auto-renew coverage for more than 115,000 Georgians. Read More
Georgia Medicaid Plan Uses Mobile Clinics to Assist Members in Maintaining Coverage. The Georgia Recorder reported on August 30, 2023, that CareSource Georgia is partnering with providers in the state to use Wellness on Wheels mobile clinics to educate and assist beneficiaries with Medicaid eligibility redeterminations and renewals. Read More
Illinois
Illinois Halts Co-pays for Undocumented Residents. The Illinois Department of Healthcare and Family Services reported on September 6, 2023, that it will halt co-pays for undocumented individuals enrolled in a state Medicaid-like program. Co-pays already collected by providers must be returned. A public hearing will be held September 12. Read More
Organizations to Receive Federal Funding to Address Youth Substance Use. Health News Illinois reported on September 6, 2023, that six organizations in Illinois will each receive $125,000 in federal funding to tackle issues ranging from tobacco prevention to opioid misuse in an effort to address youth substance use in the state. Read More
Iowa
Iowa Cites 14 Home Health Agencies for Violations. The Iowa Capital Dispatch reported on September 4, 2023, Iowa has cited 14 home health agencies for care delivery violations, including four run by county health departments. The 14 agencies are out of 15 inspected by the state to date in 2023. Read More
Kentucky
Public Comment Period Begins for MPW HCBC Waiver. The Kentucky Department of Medicaid Services (DMS) announced on September 1, 2023, that it is taking public comments through October 1, 2023, on the renewal of the state’s Michele P. waiver (MPW), a 1915(c) home and community-based services (HCBS) waiver. MPW helps individuals with intellectual or developmental disabilities live independently with supportive services. Read More
Attorney General Calls for Medicaid Work Requirements. WKU Public Radio reported on August 31, 2023, that Kentucky Attorney General Daniel Cameron wants to establish work requirements for able-bodied Medicaid beneficiaries. Read More
Montana
Montana Medicaid Providers Face Further Delay in Receiving Increased Rates. The Billings Gazette reported on September 3, 2023, that Montana Medicaid providers will not actually receive increased payment rates until September 8; although, they will receive the difference retroactively for any claims for services after July 1. A delay in final approval of the state budget pushed back the timeline for the higher payments. Read More
New Mexico
New Mexico Medicaid Expansion Would Lower Uninsured Rate, Employer Costs, Study Finds. The Santa Fe New Mexican reported on September 5, 2023, that New Mexico’s proposed Medicaid Forward expansion program would lower the uninsured rate, insurance premiums, and employer insurance costs, according to a state-funded Urban Institute study. Read More
New York
New York Managed Long-term Care Plan Is Closing Down. Beckers Payer Issues reported on September 5, 2023, that Fallon Health Weinberg, based in Amherst, NY, will close down its managed long-term care (MLTC) plan by January 12, 2024. Fallon Health was unable to meet the January 1 deadline for the new state requirement mandating health plans to offer a D-SNP plan by 2024, prompting the closure. Read More
Oregon
Oregon to Step Up PBM Regulation After Audit Finds Lax Oversight. The Tillamook Headline Herald reported on September 4, 2023, that the Oregon Health Authority (OHA) will step up regulation of pharmacy benefit managers (PBMs) after a state audit found that oversight is lax and minimal. OHA said that by mid-2024 it will hire additional staff to improve transparency and access and by January 2025 will require audits of PBMs, following a recommendation made in the audit by the Oregon Secretary of State. Read More
Pennsylvania
Senate Passes Bill to Raise Reimbursement Rate for Ambulance Services. EMS 1 reported on August 31, 2023, that the Pennsylvania Senate has passed a bill that would provide $20.7 million in state funding to increase the mileage reimbursement rate for ambulance services and improve compensation for EMS employees. The bill, which has not yet passed the House, was originally introduced by Representative Thomas Mehaffie (R-Dauphin County) and several co-sponsors in the House Aging and Older Adult Services Committee. Read More
Tennessee
Tennessee Awards Findhelp Contract to Connect Medicaid Beneficiaries with Social Services. Findhelp announced on August 31, 2023, that it has been awarded a contract with the Tennessee Medicaid agency TennCare to aid beneficiaries in finding non-medical social care services. The system will connect individuals with community-based organizations and track resulting outcomes. Read More
Texas
Texas to Request Federal Funding to Implement Medicaid Postpartum Coverage Extension. The Austin Chronicle reported on August 31, 2023, that Texas plans to submit a state plan amendment to the Centers for Medicare & Medicaid Services (CMS) to secure funding for implementation of House Bill 12, which grants Medicaid postpartum coverage for one year. If CMS approves the state plan amendment, implementation is projected to begin on March 1, 2024. Read More
Virginia
Virginia Proposed Budget to Renew Individual Market Reinsurance Program. The Richmond Times Dispatch reported on September 2, 2023, that a proposed Virginia budget bill would continue the state’s individual reinsurance program. The proposed budget also includes funds to increase behavioral crisis services, supportive housing, higher pay personal care providers, and 500 more slots for community services under the state’s Medicaid developmental disability waiver. Read More
Virginia Receives More Than 60,000 Responses to Medicaid Eligibility Notification Program. The Virginia Mercury reported on August 31, 2023, that the Virginia Department of Medical Assistance Services (DMAS) received more than 63,982 requests for information about Medicaid eligibility during the first year of the state’s facilitated enrollment program in 2022. The program lets individuals find out if they are eligible for Medicaid by checking a box on their state tax return. Read More
West Virginia
West Virginia Receives CMS Approval for Medicaid Mobile Crisis State Plan Amendment. The Centers for Medicare & Medicaid Services (CMS) approved on September 5, 2023, a Medicaid state plan amendment that will allow West Virginia to develop mobile crisis intervention teams to connect eligible individuals to behavioral health providers 24 hours a day. The program is effective July 1, 2023. Read More
National
CMS to Provide Funding to Help States Implement AHEAD Total Cost of Care Delivery System Model. The Centers for Medicare & Medicaid Services (CMS) announced on September 5, 2023, that it will provide up to $12 million each to eight states to help implement a total cost of care delivery system initiative with an emphasis on primary care called States Advancing All-Payer Health Equity Approaches and Development (AHEAD). The first of two notices of funding opportunities will be released in late fall 2023, with applications due in 90 days. The program will run from summer 2024 through December 2034. AHEAD is based on existing state all-payer initiatives in Maryland, Vermont, and Pennsylvania. Read More
CMS Releases Proposed Minimum Staffing Standards for Long-Term Care Facilities. The Centers for Medicare & Medicaid Services (CMS) released on September 1, 2023, minimum staffing standards for long-term care (LTC) facilities participating in Medicare and Medicaid, including national minimum nurse staffing standards. The proposal would set per resident per day minimums of 0.55 hours from a registered nurse (RN) and 2.45 hours from a nurse aide. It would also require an RN onsite 24 hours a day. CMS is seeking comments through November 6, 2023. Read More
Flat Medicare Spending Results in Reduced Federal Deficit. The New York Times reported on September 4, 2023, that Medicare spending has been flat for over 10 years, a trend partially attributable to the Affordable Care Act. More broadly, the drivers have been unclear. Read More
Medicaid, CHIP Enrollment Falls in May 2023, CMS Reports. The Centers for Medicare & Medicaid Services (CMS) announced on August 31, 2023, that enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) was nearly 94 million in May 2023, a decrease of 321,060 from April 2023. Medicare enrollment topped 65.9 million, up 118,238 from April 2023, including 32 million in Medicare Advantage plans. More than 12 million Medicare-Medicaid dual eligibles are counted in both programs. Read More
Humana Files Federal Lawsuit Over Medicare Advantage Clawback Rule. Health Payer Specialist reported on September 1, 2023, that Humana Benefit Plan of Texas filed a federal lawsuit over a plan that would allow the U.S. Department of Health and Human Services to claw back overpayments to Medicare Advantage plans. Clawbacks are expected to total $4.7 billion over 10 years. Read More
Medicaid Enrollees With HIV May Not Be Receiving Critical Services, OIG HHS Finds. The Department of Health and Human Services (HHS) Office of Inspector General (OIG) reported on August 31, 2023, that more than a quarter of Medicaid enrollees with HIV may not have received one or more critical services in 2021, including medical visits, viral load tests, and antiretroviral therapy prescriptions. The finding is based on claims data for Medicaid and dual-eligible enrollees. Read More
Industry News
Molina Acquires My Choice Wisconsin. Molina Healthcare announced on September 5, 2023, that it completed its acquisition of My Choice Wisconsin, which serves more than 44,000 managed long-term services and supports and other Medicaid members. Read More
RFP Calendar

HMA News & Events
Upcoming HMA Webinar:
Medicare Policy Changes Impacting Behavioral Health Services Workforce and Population Health. With recent rule changes proposed by the Centers for Medicare and Medicaid Services (CMS) addressing expanding access to behavioral health services, this webinar will focus on how those changes will impact the already strained workforce, and corresponding impacts on population health. HMA Experts will dive deeper into approaches to handle workforce shortages while expanding access. Tuesday, September 12, 12pm ET. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Illinois Medicaid Managed Care Enrollment is Up 2.5%, Jul-23 Data
- Illinois Dual Demo Enrollment is Down 1.4%, Jul-23 Data
- Indiana Medicaid Managed Care Enrollment Is Up 3.2%, May-23 Data
- West Virginia Medicaid Managed Care Enrollment is Down 6.6%, Jun-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Virginia Cardinal Care Managed Care RFP, 2023
Medicaid Program Reports, Data, and Updates:
- Colorado Medicaid Dental Annual Report, SFY 2022
- Georgia Medical Care Advisory Committee Meetings, 2021-22
- Hawaii Department of Human Services Annual Reports, 2013-22
- Hawaii QUEST Integration Section 1115 CMS Quarterly Reports, 3Q22
- Illinois Medical Programs External Quality Review Annual Reports, FY 2012-22
- Maryland Health Benefit Exchange Annual Reports, 2018-22
- Maryland HealthChoice Consumer MCO Report Cards, 2019-23
- Ohio Reports on Pregnant Women, Infants, and Children, 2020-21
- TennCare Survey of Recipients, 2019-22
- Texas Quarterly Reports from the HHS Ombudsman Managed Care Assistance Team, FY 2019-23
- Vermont Blueprint for Health Annual Reports, 2015-22
- Washington Value-Based Payment Quality Report Cards, 2021-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
