HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: The Role of Specialized Managed Care in Addressing the Intersection of Child Welfare Reform and Behavioral Health Transformation

- Early Bird Registration Now Available for HMA’s Spring Workshop on Implementing Value Based Care

- Medicaid Redetermination Update: Arizona, Iowa, Utah

- Arkansas Assisted Living Facilities Face Financial Crisis, Possibility of Closures

- California Los Angeles County Implements Free Behavioral Health Programs for K-12 Students

- Florida Senate President Proposes Initiative to Increase Healthcare Access, Workforce

- Idaho Moves Forward with Magellan Health’s Behavioral Health Plan Contract

- Kansas Rural Hospitals at Risk of Closing, Report Finds

- Massachusetts Medicaid to Cover Doula Services by Spring 2024

- Michigan Expands Medicaid Coverage to Include Community Health Worker Services

- New Hampshire Releases Technical Scoring for Contract Bids on Medicaid Procurement

- New Hampshire Experiences Strong Demand in Adult Medicaid Dental Program

- North Carolina Provides 12-Month Continuous Medicaid, CHIP Coverage for Children

- Oregon Medicaid Committee Recommends Against SCAN Acquisition of CareOregon

- West Virginia Medicaid Program Faces $114 Million Budget Deficit in Fiscal 2025

- CMS Guidance Promotes Tool to Improve Medicaid Access to HCBS Direct Support Workers

- Medicare Advantage Market Grows More Competitive

- House Passes Bill Requiring Greater PBM Transparency, Hospital Site Neutrality Policies

- Federal Government to Crack Down on Anticompetitive Health Insurer Transactions

- Cigna, Humana Scrap Merger Discussions

In Focus
The Role of Specialized Managed Care in Addressing the Intersection of Child Welfare Reform and Behavioral Health Transformation
This week, our In Focus section highlights the efforts of Health Management Associates (HMA) and partner organizations to better coordinate services for children in foster care and for children with behavioral health needs.
First, HMA released an issue brief on November 6, 2023, as part of a partnership between HMA and the National Association of State Mental Health Program Directors (NASMHPD) Technical Assistance Coalition. Together HMA and NASMHPD experts wrote a series of five briefs on children’s behavioral health.
The brief released last month, “The Role of Specialized Managed Care,” written by HMA experts Heidi Arthur and Angela Bergefurd, with input from Caitlin Thomas-Henkel and Uma Ahluwalia, centered on the intersection of child welfare reform and behavioral health transformation. More specifically, it described how specialized Medicaid managed care plans can ensure better alignment between child welfare and behavioral healthcare services.
The paper emphasizes the role of state-level special needs plans (SNPs) in the delivery of coordinated care and examines the opportunities afforded to states seeking to leverage specialty managed care plans.
Specialized managed care plans can help fill the void by incentivizing the provision of services for children in foster care and specialty services for children with behavioral health needs. Plans in three states — Washington, Arizona, and Ohio — are highlighted, and can serve as examples of how state Medicaid SNPs can be implemented.
This paper is part of a larger effort that HMA and several partner organizations are supporting. Stakeholders include:
- NASMHPD
- The Annie E. Casey Foundation
- Casey Family Programs
- MITRE
- National Association of Medicaid Directors (NAMD)
- Child Welfare League of America (CWLA)
- Administration for Children and Families
- Substance Abuse and Mental Health Services Administration
The goal of these collaborations is to foster dialog between state agencies and stakeholders working to improve the well-being of children and youth with complex needs.
Most recently, HMA hosted a webinar December 12, 2023, featuring speakers from the partner organizations to discuss insights from a federal meeting that took place in November. Webinar speakers also informed participants about plans for a multistate policy lab scheduled for February 2024, where representatives of up to eight state child welfare agencies will participate in a two-day workshop on improving the children’s behavioral health continuum of care in their states. The webinar focused on the overall effort and provided a forum for states to hear from this partnership on the importance of collaborating to strengthen the children’s behavioral health system. Watch the webinar here.
For questions about the brief, please contact Heidi Arthur or Angela Bergefurd. For questions about the webinar or the larger effort, please contact Caitlin Thomas-Henkel or Uma Ahluwalia.
Early Bird Registration Now Available for HMA’s Spring Workshop on Implementing Value Based Care
The HMA Spring Workshop: Getting Real About Transforming Healthcare Quality and Value
Kickoff Dinner & Networking: March 5, 2023, 5pm
Workshop: March 6
Fairmont Chicago Millennium Park
As we prepare for the new year, “change” is top of mind. HMA’s Spring Workshop will offer a unique opportunity to collaborate on change-oriented strategies and actions that advance value-based care.
Provocative speakers and facilitators will challenge you and your team to deepen your understanding of the complexities and real issues within the current value-based care landscape.
Working sessions will support action-oriented and solutions-focused conversations among peers. You will leave with multi-sector insights and ideas for taking your organization to the next phase of your value journey, as well as opportunities for continued engagement with peers.
Who Should Attend?
Executives and leaders from provider organizations, management services organizations and other physician enablers, federal, state and local government entities, payers, vendors, and community-based organizations will benefit from attending this event. Organizational leaders responsible for payment and risk management, policy and strategy, metrics and outcomes, and data and technology should attend.
Space is limited for this event.
Early Bird Registration ends January 26.
Register Now.
HMA Roundup
Arizona
Arizona Disenrolls 436,037 Medicaid Beneficiaries During Redeterminations, Adds Heat Map Feature to Redetermination Dashboard. The Arizona Health Care Cost Containment System (AHCCCS) announced on December 11, 2023, that it has disenrolled 436,037 Medicaid beneficiaries during redeterminations from April through November. The state has renewed coverage for more than 1.2 million beneficiaries. AHCCCS has also released a new “heat map” that provides zip code level information about the likelihood of losing coverage due to procedural reasons. Read More
Arkansas
Arkansas Assisted Living Facilities Face Financial Crisis, Possibility of Closures. The Malvern Daily Record reported on December 8, 2023, that six Arkansas assisted living facilities are facing the possibility of closure within 60 days, and several more providers are financially stressed and at risk of closing. The facilities attribute the strain to Arkansas Governor Sarah Huckabee Sanders delaying approval of Medicaid reimbursement increases that were slated to take effect January 1, 2023, for the state’s 55 Medicaid assisted living communities. Read More
California
Los Angeles County Implements Free Behavioral Health Programs for K-12 Students through MCOs. KFF Health News reported on December 12, 2023, that Los Angeles County’s Medi-Cal plans are currently implementing four projects to offer free mental health services to K-12 students. California’s Student Behavioral Health Incentive Program will invest up to $83 million in these projects, which include teletherapy services that allow students to see clinicians virtually. Hazel Health, a company offering teletherapy, is slated to receive $20 million from the county to provide services through 2024, with the potential for renewal if the program proves effective. Read More
Florida
Florida Senate President Proposes Initiative to Increase Healthcare Access, Workforce. Health News Florida reported on December 8, 2023, that Florida Senate President Kathleen Passidomo (R-Naples) released a proposed legislative package aimed at increasing healthcare access and technological innovation by expanding the health care workforce with new programs for education, training, and retention. The Senator’s “Live Healthy” plan, which seeks nearly $900 million in state and federal funding, would also expand access to free and charitable clinics, enhance coverage for mobile response teams, and require the state to seek federal approval of a program allowing Medicaid beneficiaries to receive hospital care at home. Read More
Idaho
Idaho Moves Forward with Magellan Health’s Behavioral Health Plan Contract After Judges Dismiss Opposing Lawsuits. The Idaho Capital Sun reported on December 13, 2023, that Magellan Health will begin administering the Idaho Behavioral Health Plan beginning July 1, 2024, according to an announcement from the Idaho state department of health. The start date decision comes after two state district court judges dismissed lawsuits from the other bidders, Beacon Health and Optum Health. The four-year, $1.2 billion contract will provide inpatient mental health care along with outpatient services to approximately 331,549 Medicaid beneficiaries. Optum Health, the current contract holder, disagreed with the court rulings and has appealed to the Idaho Supreme Court. Read More
Iowa
Iowa Disenrolls 2,737 Medicaid Beneficiaries During November Redeterminations. The Iowa Department of Health and Human Services on December 8, 2023, reported that it has disenrolled 2,737 Medicaid beneficiaries during November redeterminations, of which 610 were due to procedural reasons. The state has renewed coverage for 35,468 beneficiaries in November. The state has 26,976 pending eligibility cases for individuals whose renewal was due in November.
Kansas
Kansas Transitional Medicaid Program Made $16 Million in Overpayments, State Audit Finds. WIBW reported on December 11, 2023, that the Kansas Transitional Medicaid Program, TransMed, made $16 million worth of overpayments to 2,322 beneficiaries who received 13 months or more of continuous coverage before the March 2020 COVID-19 Public Health Emergency, according to an audit from the Office of Medicaid Inspector General. In total, 9,322 beneficiaries were found to have 13 months or more of continuous TransMed coverage over a three-year period from 2019 and 2021, and about 580 beneficiaries may still be receiving payments. Recommendations include strengthening overpayment process provisions and holding managed care organizations accountable when tracking a TransMed beneficiary’s continuous eligibility. Read More
Rural Hospitals At Risk of Closing, Report Finds. The Kansas Reflector reported on December 12, 2023, that 59 rural Kansas hospitals are in jeopardy of closing and 28 are at immediate risk of collapse as of October 2023, according to a report by the Center for Healthcare Quality and Payment Reform. Additionally, 84 of the state’s 102 rural hospitals recorded financial losses on patient services, prompting Kansas Governor Laura Kelly to reiterate her support to expand Medicaid. Read More
Massachusetts
Massachusetts Medicaid to Cover Doula Services by Spring 2024. MassLive reported on December 8, 2023, that Massachusetts’ Medicaid program, MassHealth, will cover doula services for pregnant, birthing, and postpartum individuals beginning in spring 2024, as a part of efforts to improve maternal and infant health outcomes. MassHealth’s doula coverage will include labor and delivery support and visits during pregnancy and the postpartum period. Doulas who enroll as a MassHealth provider will be eligible to earn payment for serving MassHealth members. Read More
Michigan
Michigan Expands Medicaid Coverage to Include Community Health Worker Services. The Michigan Department of Health and Human Services (MDHHS) announced on December 7, 2023, that it has expanded Medicaid coverage to include community health worker (CHW) services, effective January 1, 2024. Medicaid CHW coverage includes health system navigation and resource coordination; health promotion and education; and screening and assessment. MDHHS selected Michigan Community Health Worker Alliance through a competitive bid process to support provider qualification assessment, certification, and the development of a registry of certified providers. Read More
Mississippi
Mississippi Medical Care Advisory Committee Delays Recommendation on Prenatal Presumptive Medicaid Eligibility. Mississippi Today reported on December 11, 2023, that the Mississippi Medical Care Advisory Committee held a hearing to discuss establishing prenatal presumptive Medicaid eligibility that would make it easier for pregnant Medicaid beneficiaries to access timely prenatal care. Mississippi Medicaid Director Drew Snyder urged the committee to delay recommending presumptive Medicaid eligibility for expectant mothers, while Senators Kevin Blackwell (R-Southaven) and Nicole Boyd (R-Oxford) plan to co-author a bill during the upcoming legislative session to allow presumptive eligibility for pregnant women. Read More
New Hampshire
New Hampshire Releases Technical Scoring for Contract Bids on Medicaid Procurement. Health Payer Specialist reported on December 11, 2023, that New Hampshire released technical scores for Centene, AmeriHealth Caritas, and Boston Medical Center/WellSense, all of which submitted bids for the state’s Medicaid procurement and are current contract holders. The state has previously reported that it expects to award three contracts. Contract execution is expected December 11. Read More
New Hampshire Experiences Strong Demand in Adult Medicaid Dental Program, Seeks More Providers. New Hampshire Bulletin reported on December 8, 2023, that more than 8,000 people have seen a dentist, oral surgeon, or hygienist in the 8 months since New Hampshire Medicaid began covering basic dental services for adults. Currently, about 145 of the state’s 850 dentists are participating, although the state Department of Health and Human Services, Northeast Delta Dental, and DentaQuest are working to recruit more dental providers, specifically those that will treat people with disabilities. DentaQuest is offering transportation to and from appointments, and Northeast Delta Dental is offering student loan repayments for new dentists who sign-on to the program. Read More
New Jersey
New Jersey State Assembly to Vote on Bill to Implement Medicaid Community-based Palliative Care Services. NJ Spotlight News reported on December 7, 2023, that the New Jersey State Assembly will take a final vote on a bill (AB 5225) that would provide Medicaid beneficiaries with community-based palliative care services. Governor Phil Murphy previously signed the bill with the condition that the New Jersey Department of Human Services have two years to implement the new benefit, which lawmakers incorporated into the final version of the bill. The bill is sponsored by assemblywomen Angela McKnight (D-Hudson), Shanique Speight (D-Essex), and Carol Murphy (D-Burlington). Read More
New York
New York Officials Find Inaccurate Health Plan Directories with Mental Health Providers. Crain’s New York reported on December 8, 2023, that among mental health providers listed in New York health plan directories, 86 percent did not take in-network patients, according to a report by New York Attorney General (AG) Letitia James’ office. The AG’s office conducted a secret shopper survey of 13 public program and commercial health plans, including Aetna, CDPHP, Cigna, Emblem, Empire BlueCross BlueShield, Excellus, Fidelis, Healthfirst, Independent Health, MetroPlus, Molina, MVP, and UnitedHealthcare. The attorney general recommended state regulators, such as the Department of Health, the Office of Mental Health, and the Department of Financial Services, issue new network adequacy regulations and enhance oversight and enforcement of health plans. Read More
North Carolina
North Carolina Provides 12-Month Continuous Medicaid, CHIP Coverage for Children. North Carolina Health News reported on December 13, 2023, that North Carolina will provide children with 12-months of continuous Medicaid and Children’s Health Insurance Program (CHIP) coverage, aiming to insulate them from procedural disenrollments as the state continues Medicaid redeterminations. Through November, the number of children covered by North Carolina Medicaid has dropped by about 53,000. Separately, North Carolina requested federal approval to allow younger kids to remain continuously enrolled in the program through age 5 and older children to remain enrolled for two years before needing to renew their eligibility. Read More
Oregon
Oregon Medicaid Committee Recommends Against SCAN Acquisition of CareOregon. The Lund Report reported on December 6, 2023, that the Oregon Medicaid Advisory Committee has recommended that Oregon Health Authority reject SCAN’s acquisition of CareOregon, unless SCAN provides sufficient responses to a series of questions laid out in the Committee’s memo. The 15 questions seek clarification on how the acquisition would improve services to Oregon Health Plan members, how SCAN anticipates addressing health care inequities, and the impact of diverting financial resources to the new entity. Read More
West Virginia
West Virginia Medicaid Program Faces $114 Million Budget Deficit in Fiscal 2025. West Virginia Watch reported on December 13, 2023, that West Virginia’s Commissioner for the Bureau of Medical Services, Cindy Beane, informed lawmakers on the Joint Committee on Government and Finance that the state’s Medicaid program will experience a $114 million budget deficit in fiscal 2025, which begins July 1, 2024. Beane reported on drivers of the deficit, including the loss of the COVID-19 related enhanced federal funding, higher enrollment compared to pre-COVID, and drug prices, among other factors. She also discussed potential solutions, including increasing the tax on Medicaid managed care organizations to six percent, reducing provider reimbursement rates, and delaying the implementation of the Certified Community Behavioral Health Center program and mobile crisis intervention services. Read More
National
CMS Guidance Promotes Tool to Improve Medicaid Access to HCBS Direct Support Workers. The Centers for Medicare & Medicaid Services (CMS) released on December 12, 2023, new guidance advising states on the use of worker management platforms, also referred to as registries, to connect Medicaid beneficiaries receiving home and community-based services (HCBS) with qualified direct support workers who can provide such services. Specifically, the guidance emphasizes the use of worker registries to enable beneficiaries to choose care settings and highlights federal funding made available through the American Rescue Plan that can be used to build the registries. Read More
Medicare Advantage Market Grows More Competitive, Report Finds. Modern Healthcare reported on December 12, 2023, that among 381 metropolitan statistical areas surveyed in 2022, 71 percent were considered highly concentrated for Medicare Advantage, down from 87 percent in 2017, according to the American Medical Association’s annual report on health insurers. A single carrier held at least half of the Medicare Advantage market share in 31 percent of metropolitan areas, and one carrier held at least half the Marketplace program market share in 67 percent of areas. UnitedHealth Group was the largest commercial and Medicare Advantage insurer nationally while Centene was the largest Marketplace insurer. Read More
House Passes Bill Requiring Greater PBM Transparency, Hospital Site Neutrality Policies. Modern Healthcare reported on December 11, 2023, that the U.S. House of Representatives passed The Lower Costs More Transparency Act of 2023, which requires hospitals, insurers, imaging services, diagnostic laboratories, and pharmacy benefit managers (PBMs) to disclose prices and costs. It also bans PBMs from Medicaid spread pricing. Additionally, the bill delays for each of the next two years $8 billion in cuts to the Disproportionate Share Hospital program. The bill includes a four-year phase in of site-neutral payment policies beginning in 2025, and extends the National Health Service Corps through 2025, the Teaching Health Center Graduate Medical Education program through 2030, and funding for community health centers. The bill was sponsored by Representative Cathy Rodgers (R-WA). Read More
Federal Government to Crack Down on Anticompetitive Health Insurer Transactions. Health Payer Specialist reported on December 8, 2023, that the Biden administration has ordered federal antitrust regulators to investigate smaller mergers and acquisitions among major health insurance payers. The U.S. Department of Justice, Federal Trade Commission and U.S. Department of Health and Human Services will participate in a data-sharing initiative to help antitrust enforcers identify potentially anticompetitive transactions, according to the administration’s fact sheet. Read More
CMS Releases New Medicaid, CHIP Health Equity Data Briefs. The Centers for Medicare & Medicare Services (CMS) released on December 7, 2023, a second set of health equity data briefs which provide demographic information about the composition of the Medicaid and Children’s Health Insurance Program (CHIP) based on 2020 data. The briefs describe data about mental health/substance use disorder services, the Section 1915(c) waiver program, and well-child visits. Key data findings include 93 percent of children under age 1 received a well-child visit, nearly a quarter of enrollees, ages 21 to 64, received a behavioral health service, and Asian/Pacific Islander and Hispanic enrollees receive behavioral health services at lower rates than other racial and ethnic groups. Read More
MedPAC Recommends 1.3 Percent Increase to Medicare Physician Pay Levels in 2025. MedPage Today reported on December 7, 2023, that the Medicare Payment Advisory Commission (MedPAC) is considering a recommendation that Medicare increase reimbursement for physicians by about 1.3 percent in 2025, half of the projected increase in the Medicare Economic Index. MedPAC’s analysis finds that while rates are currently sustainable, without the increase in 2025, clinicians may not be able to absorb projected increases in input costs. The Commission is also considering reiterating its previous recommendation that no-budget neutral add-on payments for fee schedule services to low-income Medicare beneficiaries be established, including 15 percent for primary care clinicians and 5 percent for non-primary care clinicians. Read More
Commerce Department Seeks Input on Policy for Addressing Drug Prices. NPR reported on December 7, 2023, that the Department of Commerce (DOC) has released a request for information (RFI) on a proposed framework describing when a federal agency may decide to take over patents for medicines developed with significant government funding if it believes the prices are set too high. The 60-day public comment period for the proposal will begin after the date of publication to the federal register. Read More
Nearly 7.3 Million Have Selected ACA Marketplace Plans Since Enrollment Period Began. The U.S. Department of Health and Human Services announced on December 6, 2023, that nearly 7.3 million people have selected an Affordable Care Act (ACA) Health Insurance Marketplace plan since the opening of the 2024 Marketplace Open Enrollment Period on November 1. Approximately 1.6 million people (23 percent) are new Marketplace consumers for 2024, and approximately 5.7 million (77 percent) are returning consumers. Read More
MACPAC Announces Agenda for December 14-15 Meeting. The Medicaid and CHIP Payment and Access Commission (MACPAC) announced on December 8, 2023, that its next meeting will be held on December 14-15. Topics for discussion include Medicaid continuous coverage unwinding, Medicaid demographic data collection, proposed rulemaking in Medicare Advantage, and barriers to improving the transparency of Medicaid financing. Read More
Industry News
Cigna, Humana Scrap Merger Discussions. Modern Healthcare reported on December 10, 2023, that Cigna and Humana have ended conversations around a stock-and-cash transaction deal. Cigna announced plans to buy back $10 billion worth of stock, bringing its total planned repurchases to $11.3 billion. The insurer is also considering smaller, “bolt-on” acquisitions in the near term. Read More
AHIP Names Mike Tuffin as Chief Executive. POLITICO Pro reported on December 11, 2023, that AHIP has named Mike Tuffin as president and chief executive, effective January 8, 2024. Tuffin returns to AHIP after serving as senior vice president for external affairs at UnitedHealth Group since 2015. Read More
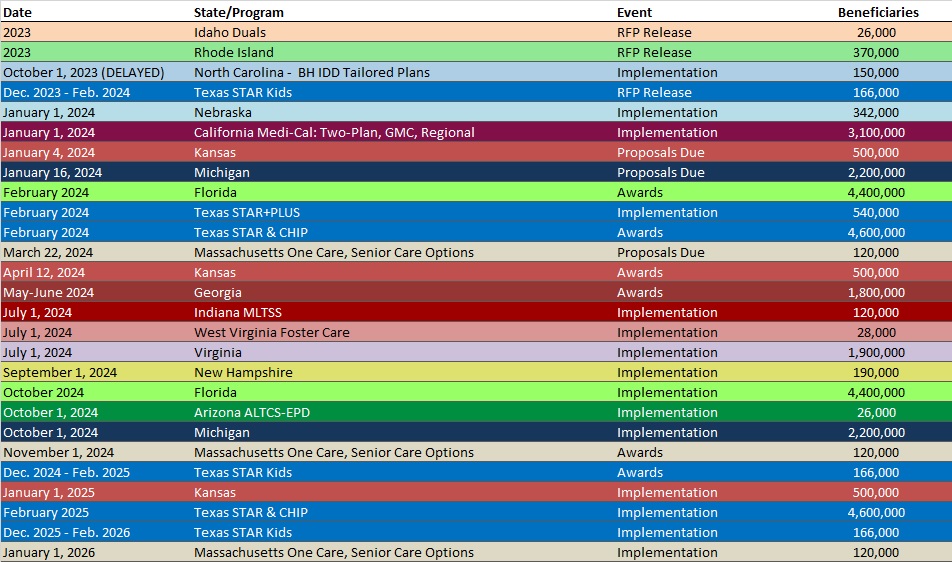
RFP Calendar
HMA News & Events
Wakely, an HMA Company, White Paper:
Considerations for Benefit Vendors and Providers in Demonstrating Their Value Proposition to Health Plans. In recent years, health insurers find themselves facing increasing pressures –from a competitive outlook and also from a financial standpoint – to create tangible improvements in health outcomes within the United States. It’s within this dynamic backdrop that a myriad of provider and benefit vendors are stepping forward to unveil innovative and previously unexplored solutions to the complex challenges in the healthcare sector. A key challenge that these companies frequently face is in demonstrating their value proposition to health plans so that their services can be included as covered benefits or as care management programs. Often, the providers and benefit vendors offer a compelling solution but are unable to support the effectiveness of their programs due to the newness of the solution. This whitepaper will explore the value proposition that these solutions can bring to the healthcare market, analyses that can be conducted to support the value proposition claims, and strategies to get data in order to conduct a retrospective study on the solutions. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Arizona Medicaid Managed Care Enrollment is Down 12%, Oct-23 Data
- Colorado RAE Enrollment is Down 9.5%, Sep-23 Data
- Colorado RAE Enrollment is Down 6.3%, Aug-23 Data
- MLRs Average 82.3% at Florida MMA MCOs, 2022 Data
- Maryland Medicaid Managed Care Enrollment Is Down 1.3%, Sep-23 Data
- Maryland Medicaid Managed Care Enrollment Is Down 1.2%, Aug-23 Data
- Michigan Medicaid Managed Care Enrollment is Down 5.9%, Oct-23 Data
- Michigan Dual Demo Enrollment is Down 13%, Oct-23 Data
- New Jersey Medicaid Managed Care Enrollment is Down 4.5%, Nov-23 Data
- North Dakota Medicaid Expansion Enrollment is Down 13.1%, Oct-23 Data
- Sole North Dakota Medicaid MCO’s MLR Is 74.6%, 2022 Data
- Puerto Rico Medicaid Managed Care Enrollment is Up 1.6%, Nov-23 Data
- Tennessee Medicaid Managed Care Enrollment is Down 1.5%, Oct-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Arizona Pharmacy Benefits Management (PBM) Services RFP and Q&A, 2023
- Louisiana Medicaid Consulting and Technical Assistance RFI, Dec-23
- Minnesota Projects for Assistance in Transition from Homelessness (PATH), Housing with Supports for Adults with Serious Mental Illness Grant Program (HSASMI) RFP, Dec-23
- New Hampshire Medicaid Care Management RFP and Scoring, 2023
- Utah Medicaid Managed Care Quality Consultant RFP, Dec-23
Medicaid Program Reports, Data, and Updates:
- Florida Governor’s Proposed Budget, FY 2025
- Iowa PHE Medicaid Redeterminations Monthly Report to CMS, Nov-23
- Kansas OMIG Transitional Medical Program Audit Report, Dec-23
- Louisiana Adjusted Medical Loss Ratio Rebate Calculation Reports, CY 2021
- Louisiana EQR Technical Reports, SFY 2022
- Texas Actuarial Analysis of Medicaid Managed Care Rates, FY 2024
- Texas HHS Quality Measures and Value-Based Payments Annual Reports, 2018-23
- Texas HHS Ombudsman Annual Report, 2023
- West Virginia Medicaid Managed Care Capitation Rate Development, SFY 2024
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Andrea Maresca at [email protected]
