HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Medicare’s 2024 Proposed Payment Rules Offer a Mix of Opportunities and Policy Changes for Physicians and Hospitals

- Redeterminations News: Arkansas, Connecticut, Georgia, Iowa, Kentucky, North Carolina, North Dakota, Texas, Wyoming

- California Health Plan to Provide $46 Million in Grants for Housing, Other Services

- Colorado Medicaid, CHIP Are Among Payers Most Likely to Reimburse for Unnecessary Health Services, Study Finds

- Florida Is Ordered to Amend Medicaid Program to Prevent Institutionalization of Children with Complex Needs

- Hawaii to Seek Medicaid Services for Justice-involved Populations Prior to Release

- Illinois Provides $75 Million in Funding to Address Health Disparities, Housing

- Medicaid Disenrollments Top 3 Million Following Redeterminations

- MTM Acquires Medical Transportation Brokerage of Arizona

In Focus
Medicare’s 2024 Proposed Payment Rules Offer a Mix of Opportunities and Policy Changes for Physicians and Hospitals
This week’s In Focus section is the first in a summer series of analysis and insights from Health Management Associates (HMA) on recent Medicare payment and policy developments. Our series kicks off with a big-picture take on the slew of regulations the Centers for Medicare & Medicaid Services (CMS) has released over the past two weeks. In future posts, we will dig deeper into several of the planned changes to highlight their potential impact on financial and operational decisions across the healthcare industry.
In July, CMS published three significant proposed Medicare rules for calendar year (CY) 2024: the Physician Fee Schedule (PFS) Proposed Rule, which includes proposed changes to the Medicare Shared Savings Program (MSSP); a proposed remedy to 340B-acquired drug payment policy for CY 2018−2022; and the Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System (OPPS-ASC) Proposed Rule. Comments on these proposals are due to CMS in early September.
HMA’s experts note several trends across these three Medicare payment regulations:
- Health equity remains a significant focus of CMS and the Biden Administration.
- The agency is expanding its coverage of behavioral health services under Medicare and enhancing payment and access for these services.
- The long-term focus of CMS continues to be the transition toward value-based care.
- Medicare is incrementally moving toward supporting care that is delivered where and how Medicare beneficiaries prefer, for example moving away from reimbursing largely for face-to-face services and supporting reimbursement for telehealth services in more situations.
- CMS is creating pathways for reimbursement for a broader range of clinicians and caregivers who are addressing Medicare beneficiaries’ care needs.
- CMS continues its efforts to improve hospital price transparency with policies aimed at encouraging providers to publicly report data.
Medicare policy experts at HMA and is affiliate, The Moran Company, summarize details on these regulations below. These colleagues work collaboratively to monitor legislative and regulatory developments in the physician, 340B, and outpatient and ASC policy arenas and to assess the impact of changes in these reimbursement systems. HMA’s Medicare experts interpret and model policy proposals and use these analyses to assist clients in developing their strategic plans and comment on proposed regulations. Moran annually replicates the methodologies CMS uses to set payments and recommends alternative payment policies to help support its clients’ comments on various rules and to help clients understand the impact of specific policies. In addition, HMA’s other partner companies, including Wakely and Leavitt Partners, are monitoring these issues from their unique perspectives.
For more information or questions about the policies described below, please contact Amy Bassano ([email protected]), Zach Gaumer ([email protected]), Andrea Maresca ([email protected]), Kevin Kirby ([email protected]), or Rachel Kramer ([email protected]).
Medicare Physician Fee Schedule Proposed Rule (CY 2024)
The Medicare PFS establishes payments and policies for physicians and other healthcare professionals. By statute, PFS payment rates will decline by 1.25 percent from CY 2023 to 2024. However, when coupled with budget neutrality adjustments for other policy changes, the proposed PFS conversion factor will decline by 3.34 percent. The impact of this reduction will vary by physician specialty.
Behavioral Health Services: CMS implements provisions in the Consolidated Appropriations Act (CAA), 2023, which would allow Medicare coverage and payment for the services of marriage and family therapists (MFTs) and mental health counselors (MHCs). CMS proposes to classify addiction counselors who meet certain requirements as MHCs. The rule outlines how these practitioners can enroll in Medicare and bill for services starting January 1, 2024. CMS is establishing new codes and payment for psychotherapy for crisis services and proposed refinements to Health and Behavior Assessment/Intervention codes to allow additional practitioners to bill for these services and to increase the valuations of timed behavioral health services. CMS seeks comment on ways to expand access to behavioral health services. CMS specifically is looking for information on digital therapies, remote physiologic monitoring, and remote therapeutic monitoring services.
Evaluation and Management (E/M) Office Visit Services: CMS proposed to implement separate payment for an add-on billing code to account for the additional resources associated with primary care or ongoing care related to a patient’s single serious or complex chronic condition. This complexity-based add-on code may be reported with all office and outpatient (O/O) and evaluation and management (E/M) visit level codes, and CMS estimates it will be reported for 38 percent of all O/O E/M visits initially. This estimate contributes to a significant portion of the relative value unit (RVU) budget-neutrality adjustment applied to the conversion factor. CMS also requests comments on evaluating E/M services more regularly and comprehensively including ways to improve data collection and methodologies to establish more timely improvements and accurate payments for E/M and other services.
Telehealth: CMS proposes several additions to the list of covered telehealth services and implements the various telehealth provisions included in CAA 2023, such as allowing the patient’s home to serve as an originating site. This provision would expand the scope of permitted telehealth providers and allow rural health clinics and federally qualified health centers (FQHCs) to provide telehealth services until December 31, 2024. In addition, CMS proposes opportunities for teaching physicians and medical residents to continue to use telehealth services to meet the supervision requirements via telehealth.
Caregiver Training Services: CMS proposed a new payment for practitioners who train caregivers to implement a treatment plan and support patients with diseases like dementia.
Payment for Community Health Integration, Social Determinants of Health (SDOH) Risk Assessment, and Principal Illness Navigation Provided by Social Workers, Community Health Workers, Care Navigators, and Peer Support Specialists: CMS is establishing opportunities for these services to be paid separately and account for the specific resources necessary to provide these services.
Dental Services: Although Medicare generally is prohibited from paying for dental services, CMS proposed to pay for certain dental services related to the treatment of head and neck cancers and when linked to other covered services used to treat cancer.
Discarded Drugs: The proposed rule continues the implementation process for a statutory requirement that drug and biological manufacturers refund amounts paid for discarded single-use prescription drug vials. CMS provides the list of products for which refunds would have been due in 2021, and the number of products included is expected to increase over time.
340B and Outpatient Offset Proposed Rule
In the 340B proposed rule, CMS proposed retrospective payments to 340B hospitals for incorrect payments made in CYs 2018−2022. After extensive litigation and a Supreme Court ruling, CMS will return to paying 340B hospitals for drugs using the formula of the average sales price (ASP) +6 percent, rather than the formula of the ASP −22.5 percent. In this proposed rule, CMS proposes to correct past underpayments to 340B hospitals by making lump sum payments to affected 340B hospitals. These retrospective payments are estimated to amount to $9 billion, and we anticipate payments will be made to hospitals at the beginning of CY 2024.
In addition, CMS proposed a corresponding prospectively budget neutrality offset to the 340B spending increase that will reduce hospital outpatient payments for non-drug outpatient services by 0.5 percent each year beginning in 2025. Specifically, CMS proposes to maintain this reduction until $7.8 billion in spending has been offset, which it estimates will take 16 years. The impact of this policy on the hospital industry will be significant and will create groups of winners and losers. Winners will include 340B hospitals, despite the fact that the outpatient offset will also affect their payment rates. Losers will include non-340B hospitals, particularly if their service mix is heavily focused on outpatient surgical services. Overall, the industry will observe a reduction in outpatient spending of roughly $300 million to $600 million per year for each of the 16 years the policy is in place.
Hospital Outpatient Proposed Rule (CY 2024)
Under the OPPS proposed rule, CMS would update payments for outpatient and ASC services by 2.8 percent in CY 2024 from CY 2023. This change will increase payments for hospital outpatient services by $1.9 billion and for ASC services by $170 million. In addition, if the 340B proposal is finalized, the 0.5 percent payment offset would not reduce CY 2024 OPPS payment rates but would begin reducing outpatient payments in CY 2025.
Behavioral Health: CMS proposes to establish the Intensive Outpatient Program (IOP) for behavioral health services provided to Medicare beneficiaries. The IOP proposal addresses one of the main gaps in behavioral health coverage in Medicare and promotes access to related services. CMS will define IOP as a distinct outpatient program of psychiatric services provided to individuals with acute mental illness or substance use disorder. Services could be provided at hospital outpatient departments, community mental health centers, FQHCs, and RHCs. Further, the agency proposed to establish two IOP service codes for each provider type—one for days with three services per day and another with four or more services per day.
Price Transparency: CMS proposes to increase the rigidity of its price transparency reporting program in an effort to improve hospital industry compliance with the reporting of hospital charge data to the public.
The HMA Medicare team and Moran Company reimbursement experts will continue to analyze these proposal alongside other policy and reimbursement changes that affect Medicare providers. We have the depth and breadth of expertise to assist with tailored analysis, to model policy impacts, and to support clients that intend to draft comment letters on this proposed rule.
HMA Roundup
Arkansas
Arkansas Disenrolls More Than 77,000 Medicaid Beneficiaries During June Redeterminations. The Arkansas Department of Human Services announced on July 10, 2023, the disenrollment of more than 77,000 Medicaid beneficiaries during June redeterminations. The state renewed coverage for approximately 50,000 beneficiaries. Read More
California
California Health Plan to Provide $46 Million in Grants for Housing, Other Services. MedCity News reported on July 14, 2023, that Centene/Health Net will provide $46 million in grants to help California Medi-Cal beneficiaries find housing and other services. The funding will largely help continuum of care programs in 26 counties better connect Medicaid beneficiaries with housing and redetermination services. Read More
Colorado
Medicaid, CHIP Are Among Payers Most Likely to Reimburse for Unnecessary Health Services, Study Finds. Health Payer Intelligence reported on July 18, 2023, that the Colorado Medicaid and Children’s Health Insurance Program (CHIP) were among the payers most likely to reimburse for unnecessary or low-value healthcare services, according to an analysis from the Center for Improving Value in Health Care. The study, based on claims data from 2017 to 2021, also examined spending in the state by Medicare and commercial insurers. Among the top categories for spending on low-value services were opioid prescriptions, Vitamin D deficiency screening, prostate cancer screening, imaging tests for eye disease, and coronary angiographies. Read More
Connecticut
Connecticut Disenrolls 15,500 Medicaid Beneficiaries During June Redeterminations. The Connecticut Department of Social Services announced on July 10, 2023, the disenrollment of more than 15,500 Medicaid beneficiaries during June redeterminations. The state renewed coverage for more than 65,300 beneficiaries.
Florida
Florida Is Ordered to Amend Medicaid Program to Prevent Institutionalization of Children with Complex Needs. Health News Florida reported on July 18, 2023, that a federal judge ordered Florida to amend its Medicaid program to prevent children with complex needs from unnecessary institutionalization in nursing homes and to expand care in home and community based settings. The ruling stems from a lawsuit filed in 2013 by the U.S. Justice Department, alleging that Florida was institutionalizing children with complex needs unnecessarily. The ruling stated that approximately 140 children on Medicaid reside in nursing homes and more than 1,800 are at risk of institutionalization. Read More
Special Needs Medicare Advantage Market Gets New Entry. Becker’s Payer Issues reported on July 12, 2023, that insurer Gold Kidney Health Plan will offer nine chronic special needs Medicare Advantage plans in Florida beginning in 2024 pending regulatory approval. Gold Kidney Health Plans also offers plans in Arizona in 2023. Read More
Georgia
Georgia Disenrolls 95,000 Medicaid Beneficiaries During June Redeterminations. The Associated Press reported on July 12, 2023, that Georgia Disenrolled approximately 95,000 Medicaid beneficiaries during June redeterminations. The state renewed coverage for about 64,000 beneficiaries. Read More
Hawaii
Hawaii to Seek Medicaid Services for Justice-involved Populations Prior to Release. State of Reform reported on July 14, 2023, that Hawaii will seek approval for Medicaid services like case management and medication-assisted treatment for justice-involved populations prior to release. The state is expected to add the initiative to its Med-QUEST Section 1115 waiver renewal request, along with respite care coverage for recuperative care, short-term stays, post-hospitalization, and housing services. The current waiver expires July 31, 2024. Read More
Illinois
Health Benefits for Immigrant Seniors and Adults Program Is Projected to Run Over Budget in November. Health News Illinois reported on July 19, 2023, that the Illinois Health Benefits for Immigrant Seniors and Adults program could run over its $550 million budget as soon as November, according to the state Department of Healthcare and Family Services. In June, the state paused enrollment for adults in the program due to rising costs. Read More
Illinois Extends Hospital-at-home Program through 2024. Health News Illinois reported on July 18, 2023, that the Illinois Department of Public Health will extend its hospital-at-home program through the end of 2024. The program, which received federal approval during the COVID-19 pandemic, allows certain hospitals to provide limited inpatient services in a patient’s home. Read More
Illinois Provides $75 Million in Funding to Address Health Disparities, Housing. Health News Illinois reported on July 17, 2023, that the Illinois Housing Development Authority will provide $75 million in state and federal funding to address health disparities and housing for individuals with disabilities and those suffering chronic homelessness. The state will provide $15 million to support partnerships between affordable housing and healthcare groups and $60 million to support the acquisition, new construction, rehabilitation, or adaptive reuse of supportive housing units. Read More
Indiana
Indiana Hospital Association Calls on State Legislators to Raise Medicaid Rates. The Hamilton County Reporter Newspaper reported on July 14, 2023, that the Indiana Hospital Association released a statement urging state legislators to use surplus state funds to increase Medicaid rates and help address a $2.7 billion shortfall in unpaid Medicaid costs. Read More
Iowa
Iowa Disenrolls 8,000 Medicaid Beneficiaries During June Redeterminations. The Iowa Department of Health and Human Services announced on July 12, 2023, the disenrollment of more than 8,000 Medicaid beneficiaries during June redeterminations. The state renewed coverage for nearly 32,300 beneficiaries.
Kentucky
Kentucky Disenrolls 37,500 Medicaid Beneficiaries During June Redeterminations. The Kentucky Cabinet for Health and Family Services announced on July 4, 2023, the disenrollment of nearly 37,500 Medicaid beneficiaries during June redeterminations. The state renewed coverage for almost 40,000 beneficiaries.
Minnesota
Minnesota to Provide $36 Million to Bolster Medicaid Coverage Renewals. The Minnesota Department of Human Services announced on July 14, 2023, $36 million in funding for counties and the White Earth Nation, the only tribe in the state to process public health care program renewals, to help beneficiaries with Medical Assistance and MinnesotaCare renew their coverage. The funds will be used to hire and train staff, pay overtime, and reach out to enrollees. Read More
Mississippi
Mississippi Democratic Gubernatorial Candidate Announces Support for Medicaid Expansion. Magnolia Tribune reported on July 12, 2023, that Mississippi Democratic gubernatorial candidate Brandon Presley announced his support for Medicaid expansion. Approximately 220,000 Mississippians would be eligible for expanded coverage. Read More
New York
Medicaid Spending to Rise 13 Percent to More Than $87 Billion by Fiscal 2027. The New York State Comptroller published on July 18, 2023, a report noting that based on the current budget, Medicaid spending will increase from $77.4 billion to $87.3 billion, or 13 percent, between now to fiscal 2027. The state’s share of Medicaid spending will increase by about six percent per year. Read More
North Carolina
North Carolina Disenrolls 35,000 Medicaid Beneficiaries During June Redeterminations. North Carolina Health News reported on July 19, 2023, that North Carolina disenrolled more than 35,000 Medicaid beneficiaries during June redeterminations. The state renewed coverage for nearly 138,000 beneficiaries. Read More
North Dakota
North Dakota Disenrolls 6,800 Medicaid Beneficiaries During June Redeterminations. The North Dakota Department of Health and Human Services announced on July 6, 2023, the disenrollment of more than 6,800 Medicaid beneficiaries during June redeterminations. The state renewed coverage for nearly 5,300 beneficiaries.
Oklahoma
Oklahoma Panel Approves Plan to Distribute $200 Million to Financially Struggling Hospitals. The Oklahoma Health Care Authority Board approved on July 17, 2023, a plan to distribute $200 million appropriated by the state legislature to financially struggling Oklahoma hospitals. The state will direct $150 million to hospitals proportionally based on total Medicaid payments, $25 million to the most vulnerable hospitals, and $25 million to accelerate the implementation of a new Medicaid hospital payment program. Read More
South Dakota
South Dakota to Expand Prescription Drug Stockpiles to Address Shortages. The Associated Press reported on July 17, 2023, that South Dakota governor Kristi Noem has announced that the state will expand stockpiles of prescription medications to help offset shortages and called on the federal government to decrease reliance on foreign suppliers. The state stores antibiotics in two pharmaceutical warehouses and plans to add five more sites in partnership with pharmacies and include the drugs albuterol, epinephrine, insulin, prednisone and pediatric amoxicillin. Read More
South Dakota Enrolls 1,800 Medicaid Beneficiaries Following Medicaid Expansion. Keloland News reported on July 12, 2023, that South Dakota has enrolled about 1,800 Medicaid beneficiaries since Medicaid expansion began in July. Read More
Texas
Texas Disenrolls More Than 500,000 Medicaid Beneficiaries Following Redeterminations. The Fort Worth Star-Telegram reported on July 14, 2023, that Texas has disenrolled more than 500,000 Medicaid beneficiaries since redeterminations began in April. Approximately 405,000 lost coverage due to procedural reasons and 96,000 were found ineligible; another 173,000 are pending review. Read More
Virginia
Virginia to Permanently Allow Direct State Payment of Family Caregivers. The Virginia Mercury reported on July 19, 2023, that the Virginia Department of Medical Assistance Services released a modified proposal that would permanently allow certain family caregivers to be paid directly by the state. The option, initially made available during the COVID-19 pandemic, is otherwise set to end in the fall. Read More
Wyoming
Wyoming Medicaid Waiver Beneficiaries Fail to Submit Renewal Forms, Risk Disruptions. The Wyoming Department of Health announced on July 18, 2023, that some Medicaid beneficiaries receiving services through waiver programs have not submitted proper Medicaid renewal forms and may be at risk of losing coverage following eligibility redeterminations. Waivers include the Community Choices Waiver, which serves individuals 65 and older or those aged 19 to 64 with a disability; the Supports Waiver, which serves individuals with intellectual or developmental disabilities (IDD) or brain injuries; and the Comprehensive Waiver, which provides comprehensive services individuals with IDD. Read More
National
Medicaid Disenrollments Top 3 Million Following Redeterminations. KFF reported on July 19, 2023, that more than three million people have been disenrolled from Medicaid following eligibility redeterminations. Seventy-four percent lost coverage due to procedural reasons. Read More
CMS Works to Connect Individuals Disenrolled from Medicaid With Exchange Coverage. Becker’s Payer Issues reported on July 19, 2023, that the Centers for Medicare & Medicaid Services (CMS) is increasing outreach efforts and informing disenrolled Medicaid beneficiaries of other insurance options, including Exchange coverage. As of July 18, 2023, at least 2.9 million people have lost Medicaid coverage nationwide as a result of eligibility redeterminations, according to KFF. Read More
House Committee Holds Hearing on Biden Plan to Extend Medicaid to DACA Recipients. The Iowa Capital Dispatch reported on July 18, 2023, that the House Oversight and Accountability Committee held a hearing on the Biden administration’s plan to allow Deferred Action for Childhood Arrivals (DACA) recipients to enroll in Medicaid or Exchange plans. The proposal would take effect November 1, 2023, if finalized. Read More
CMS Proposes Updating Hospital Outpatient Prospective Payment System, Ambulatory Surgical Center Rates by 2.8 Percent. The Centers for Medicare & Medicaid Services (CMS) published on July 13, 2023, a proposed rule to update the payment rates for the Hospital Outpatient Prospective Payment System and for Ambulatory Surgical Centers by 2.8 percent for providers that meet applicable quality reporting requirements. CMS is also proposing a new benefit category for Intensive Outpatient Program services, which is aimed at expanding access to behavioral health services. Additionally, CMS is proposing actions to promote health equity for tribal communities. Read More
CMS Announces 2024 Physician Payment Rule Aimed at Advancing Health Equity, Expanding Access. The Centers for Medicaid & Medicare Services announced on July 13, 2023, the proposed 2024 Medicare Physician Fee Schedule, which includes a 1.25 percent reduction in overall payments for clinicians compared to 2023. The proposal also includes coding and payment for new services, such as caregiver training and community health integration for underrepresented populations in order to advance health equity. In addition, the proposal calls for payment for Principal Illness Navigation services to help patients navigate cancer treatments and allows various behavioral professionals to enroll in Medicare and bill for services. Read More
House Committee Advances Bills on PBM Drug Cost, Pricing Transparency. Modern Healthcare reported on July 13, 2023, that the House Committee on Education and the Workforce has advanced bills aimed at improving drug costs and pricing transparency among pharmacy benefit managers (PBMs). The bills would also require PBMs to provide certain data to health plans as well as requiring new disclosures from health plans and hospitals about healthcare costs. Read More
Medicaid Expansion Is Associated with Increase in Palliative Care Use, Study Finds. Health Affairs published on July 13, 2023, a study that found that Medicaid expansion was associated with larger increases in palliative care use for people with advanced cancers. Researchers utilized data from people aged 18 to 64 who had recently been diagnosed with stage IV cancer between 2010 and 2019. Those receiving palliative care increased from 17 percent pre-expansion to 18.9 percent post-expansion in Medicaid expansion states and from 15.7 percent to 16.7 percent in non-expansion states. Read More
MACPAC Issue Brief Outlines Managed Care External Quality Review Process, CMS Policy Recommendations. The Medicaid and CHIP Payment and Access Commission (MACPAC) released in July 2023, an issue brief outlining the external quality review (EQR) process, including EQR protocols, federal funding, and state requirements. The report also outlines proposed policy changes from the Centers for Medicare & Medicaid Services (CMS), including a proposed rule released in May to alter the EQR process to reduce state burden and enhance quality improvement. Read More
Industry News
MTM Acquires Medical Transportation Brokerage of Arizona. MTM announced on July 11, 2023, the acquisition of the Medical Transportation Brokerage of Arizona, a non-emergency medical transportation (NEMT) provider and taxi operator. The acquisition closed on July 1. Read More
VersiCare Group Acquires Kentucky Y IDD Provider Open Doors. Seven Hills Capital announced on July 19, 2023, that partner company VersiCare Group has acquired Open Doors, a provider of residential and family home provider services to individuals with developmental disabilities within Kentucky’s Supports for Community Living Waiver program. This is VersiCare’s fourth acquisition in the state. Read More
Centene/Denova to Add Behavioral Health Clinics in Arizona, Expand Through Acquisitions in Other States. The Phoenix Business Journal reported on July 17, 2023, that Centene’s Denova Collaborative Health (formerly Bayless Integrated Health) will open behavioral health clinics in Tuscon and Flagstaff, AZ, and plans to expand in other states through acquisitions, according to chief executive Graham Johnson. The rebranding signals Denova’s intent to focus more on behavioral health. Read More
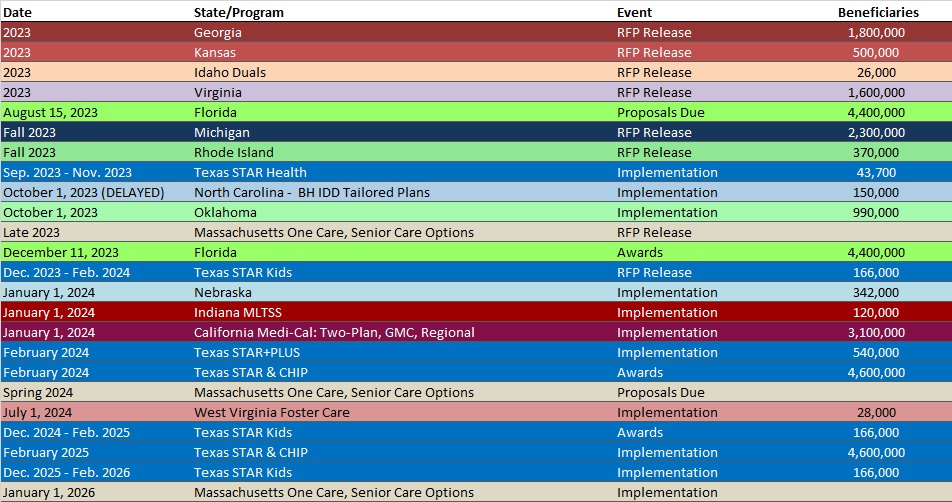
RFP Calendar
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Alaska Medicaid Fee for Service vs. Managed Care Penetration, 2014-22
- California Medicaid Fee for Service vs. Managed Care Penetration, 2014-22
- Georgia Medicaid Fee for Service vs. Managed Care Penetration, 2014-22
- Illinois Medicaid Fee for Service vs. Managed Care Penetration, 2014-22
- Indiana Medicaid Managed Care Enrollment Is Up 1.1%, Jan-23 Data
- Massachusetts Medicaid Managed Care Enrollment is Up 6.9%, 2022 Data
- Missouri Medicaid Managed Care Enrollment is Up 7%, May-23 Data
- Nevada Medicaid Managed Care Enrollment is Down 1.3%, May-23 Data
- New Mexico Medicaid Managed Care Enrollment is Down 1%, May-23 Data
- Oklahoma SNP Membership at 51,856, Mar-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- District of Columbia Medicaid Managed Care Contracts, 2022
- Utah Medicaid ACO Contracts, 2017-23
Medicaid Program Reports, Data, and Updates:
- Arizona AHCCCS External Quality Review Annual Reports, 2022
- Connecticut PHE Medicaid Redeterminations Monthly Report to CMS, Jun-23
- Georgia PHE Medicaid Redeterminations Monthly Report to CMS, Jun-23
- Iowa PHE Medicaid Redeterminations Monthly Report to CMS, Jun-23
- Kentucky Medicaid MCO External Quality Review Technical Reports, 2018-22
- Kentucky PHE Medicaid Redeterminations Monthly Report to CMS, Jun-23
- Maine Prescription Drug Affordability Board Meeting Materials, Mar-23
- North Carolina PHE Medicaid Redetermination Monthly Reports to CMS, Jun-23
- North Dakota PHE Medicaid Redeterminations Monthly Report to CMS, Jun-23
- Texas PHE Medicaid Redeterminations Monthly Report to CMS, Jun-23
- Washington PHE Medicaid Redeterminations Monthly Report to CMS, May-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio at [email protected].
