HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- Florida Disenrolls Some Children with Complex Medical Needs During Redeterminations

- Idaho Faces Lawsuits Over Medicaid Behavioral Plan Award

- Iowa Medicaid Managed Care Contracts Begin July 1

- UCare Names Former Kansas Medicaid Director Jon Hamdorf Market President

- Louisiana Governor Vetoes Part of Legislature’s Proposed Budget, Reinstates Health Spending Increase

- Maryland Extends Pregnancy, Postpartum Medicaid Benefits to Undocumented Individuals

- Massachusetts Made $85 Million in Capitation Payments on Beneficiaries Living Out of State, Audit Finds

- Minnesota Releases Medicaid, MinnesotaCare IHP RFP

- Minnesota Provides One Month Grace Period to Reenroll in Medicaid Following June Redeterminations

- Nevada Allows Medicaid to Cover Behavioral Health Services in Schools

- New Hampshire Medicaid Beneficiaries Struggle to Find Dental Care

- North Carolina Governor Urges Lawmakers to Separate Medicaid Expansion from Budget

- Oklahoma Disenrolls 54,000 Medicaid Enrollees During May Redeterminations

- South Dakota Implements Medicaid Expansion on July 1

- Washington Receives Federal Renewal of Medicaid Transformation Project Section 1115 Waiver

- Washington Disenrolls 116,000 Medicaid Beneficiaries During May Redeterminations

- Home Health Providers Face Proposed 2.2 Percent Medicare Rate Cut in Fiscal 2024

- Molina to Acquire Bright Health Medicare Advantage Subsidiaries

In Focus
The CMS Managed Care Proposed Rule: Three Implications for Local and Regional MCOs
This week, our In Focus section revisits three specific aspects and implications for regional and local managed care organizations of the proposed Medicaid and Children’s Health Insurance Program (CHIP) managed care access, finance, and quality rule published by the Centers for Medicare & Medicaid Services (CMS). HMA previously reviewed the provisions of the rule, which CMS published on April 28, 2023. If finalized as put forward, the rule will have a significant impact across Medicaid stakeholders including enrollees, managed care organizations (MCOs), providers, and state Medicaid agencies.
Medical Loss Ratio (MLR) Standards
In the proposed rule, CMS outlines three areas for revisions to its existing MLR standards which require MCOs to annually submit MLR reports to states and require states, in turn, to annually provide a summary of those reports to CMS. An MLR is calculated by adding the expenditures for incurred claims to the expenditures for activities that improve health care quality and fraud prevention activities (the numerator) and dividing this by adjusted premium revenue (the denominator). The three areas where CMS proposes revisions include: (1) requirements for clinical or quality improvement standards for provider incentive arrangements, (2) prohibited administrative costs in quality improvement activity (QIA) reporting, and (3) additional requirements for expense allocation methodology reporting.
Related to provider incentive arrangements (which are considered part of incurred claims), CMS proposes to require that contracts between MCOs and providers: (1) have a defined performance period that can be tied to the applicable MLR reporting period(s), (2) include well-defined quality improvement or performance metrics that the provider must meet to receive the incentive payment, and (3) specify a dollar amount that can be clearly linked to successful completion of these metrics as well as a date of payment. Furthermore, MCOs would be required to maintain documentation to support these arrangements and cannot rely upon attestations as documentation of compliance.
Related to QIA reporting, CMS proposes to explicitly prohibit MCOs from including indirect or overhead expenses when reporting QIA costs in the MLR. CMS notes that today, for example, expenditures for facility maintenance, marketing, or utilities may be included in the MLR even though such expenses do not directly improve health care quality. From the perspective of CMS, the inclusion of such expenditures in the MLR numerator may be resulting an inflated MLRs that then provide a distorted view of MCO performance.
Related to expense allocating reporting, CMS proposes to add requirements regarding how MCOs can allocate expenses for the purpose of calculating the MLR. Specifically, MCOs would need to describe in their methodology a detailed description of the methods used to allocate expenses, including incurred claims, quality improvement expenses, federal and state taxes and licensing or regulatory fees, and other non-claims costs. The goal of requiring this additional detail is to give state Medicaid agencies the ability to assess whether MLRs are accurately represented as a result of the methodology employed by an MCO to allocate expenses across lines of business (e.g., Marketplace, Medicaid, and Medicare).
For local and regional MCOs, the changes to MLR standards proposed by CMS will require meaningful efforts to ensure compliance. Provider incentive arrangements, most expansively, may need to be renegotiated to conform to the requirements and, at a minimum, may need to be documented in a more robust fashion to ensure evidence of compliance can be furnished upon request. The impact of QIA expenditures that are no longer able to be included in the MLR numerator will need to be modeled to ensure that a resulting failure to meet any minimum MLR requirements does not occur and, if this is projected to occur, a strategy will need to be developed and executed to ensure it does not. Expense allocation methodologies will need to be documented more extensively and evaluated for reasonability to ensure that they can withstand regulatory scrutiny when additional detail is provided to state Medicaid agencies.
Medicaid and CHIP Quality Rating System (MAC QRS)
In the proposed rule, CMS outlines a MAC QRS framework that includes: (1) mandatory quality measures, (2) a quality rating methodology, and (3) a mandatory website display format. State Medicaid agencies and MCOs will be required to adopt and implement the MAC QRS framework developed by CMS or adopt and implement an alternative managed care quality rating system. CMS will update the mandatory measure set at least every other year. Measures will have public notice through a call letter (or similar guidance) on any planned modifications with measures being based on: (1) value in choosing an MCO, (2) alignment with other CMS programs, (3) the relationship to enrollee experience, access, health outcomes, quality of care, MCO administration, or health equity, (4) MCO performance, (5) data availability, and (6) scientific acceptability.
State Medicaid agencies will be required to collect from MCOs the data necessary to calculate ratings for each measure and ensure that all data collected are validated. Additionally, state Medicaid agencies must calculate each measure and issue ratings to each MCO for each measure. Finally, the mandatory state website will be required to contain the following elements: (1) clear information that is understandable and usable for navigating the website itself, (2) interactive features that allow users to tailor specific information, such as formulary, provider directory, and ratings based on their entered data, (3) standardized information so that users can compare MCOs, (4) information that promotes beneficiary understanding of and trust in the displayed ratings, such as data collection timeframes and validation confirmation, and (5) access to Medicaid and CHIP enrollment and eligibility information, either directly on the website or through external resources.
For local and regional MCOs, the MAC QRS framework proposed by CMS will require assessing their capability to produce the mandated data upon request by state Medicaid agencies. It will also then require ensuring that all mandated data is available to be provided on an annual basis. To the extent possible, at the appropriate time, assessing baseline performance on measures and proactively developing and implementing strategies to improve performance will be prudent. Assessing the impact of the greater transparency around quality performance that the proposed MAC QRS will bring in order to understand the potential impact on competitive position will also be important.
Network Adequacy Requirements
In the proposed rule, CMS outlines important network adequacy requirements meant to further timely access to care for Medicaid and CHIP managed care enrollees. Two of these are focused upon here: (1) appointment wait time standards and (2) secret shopper surveys. Other policies to enhance access are also included in the proposed rule including, for example, a requirement that state Medicaid agencies conduct an annual enrollee experience for each MCO.
For appointment wait time standards, CMS proposes that state Medicaid agencies develop and enforce wait time standards for routine appointments for four types of services: (1) outpatient mental health and substance use disorder (SUD) for adults and children, (2) primary care for adults and children, (3) obstetrics and gynecology (OB/GYN), and (4) an additional service type determined by the state Medicaid agencies in an evidence-based manner (in addition to the previous three noted). The maximum wait times must be no longer than 10 business days for routine outpatient mental health and SUD appointments and no longer than 15 business days for routine primary care and OB/GYN appointments. State Medicaid agencies could impose stricter wait time standards but not more lax ones. The wait time standard for the fourth service type selected by state Medicaid agencies will be determined at the state level.
For secret shopper surveys, state Medicaid agencies will be required to utilize an independent entity to conduct annual secret shopper surveys to validate MCO compliance with appointment wait time standards and the accuracy of provider directories to identify errors as well as providers that do not offer appointments. For an MCO to be compliant with the wait time standards, as assessed through the secret shopper surveys, it would need to demonstrate a rate of appointment availability that meets the wait time standards at least 90% of the time. State Medicaid agencies would be required to develop remedy plans when MCO compliance issues are identified which designate the party responsible for taking action, outline the appropriate steps to be taken to address the issue, and document the intended implementation timeline.
For local and regional MCOs, the wait time standards and secret shopper surveys present opportunities to prepare to ensure compliance and to collaborate with state Medicaid agencies. For preparation, undertaking secret shopper surveys ahead of implementation to determine the current performance relative to maximum wait times may be advisable. Additionally, there is an opportunity to collaborate with state Medicaid agencies regarding the selection of the fourth service type for which wait time standards will be established.
For More Information
If you have questions about how HMA can support your efforts related to the proposed rule’s implications for local and regional MCOs, please contact Michael Engelhard, managing director, Patrick Tigue, managing director, or Sarah Owens, principal.
HMA Roundup
Florida
Florida Disenrolls Some Children with Complex Medical Needs During Redeterminations. Becker’s Payer Issues reported on June 28, 2023, that Florida has disenrolled some children with complex medical needs during Medicaid eligibility redeterminations. The Florida Department of Children and Families previously stated that it would postpone redeterminations for these individuals until 2024. Read More
Idaho
Idaho Faces Lawsuits Over Medicaid Behavioral Plan Award. The Idaho Capital Sun reported on July 5, 2023, that Idaho faces two lawsuits filed by UnitedHealth Group and Elevance Health over the decision to award the state’s $1.2 billion Medicaid behavioral health plan contract to Centene/Magellan Healthcare. United is the incumbent. The lawsuit alleges that Magellan did not meet minimum qualifications for the contract. Read More
Iowa
Iowa Medicaid Managed Care Contracts Begin July 1. The Des Moines Register reported on June 29, 2023, that the new contracts for Iowa Health Link, the state’s Medicaid managed care program consisting of traditional Medicaid, Iowa Health and Wellness Plan, and Children’s Health Insurance Program (known as Healthy and Well Kids in Iowa (Hawki)), will begin on July 1 with Molina Healthcare of Iowa and Elevance/Amerigroup Iowa. Centene/Iowa Total Care also serves the Medicaid population and holds a current contract through 2025. The Iowa Medicaid program serves more than 754,000 beneficiaries. Read More
Kansas
UCare Names Former Kansas Medicaid Director Jon Hamdorf Market President. Kansas City Business Journal reported on June 29, 2023, that UCare named Jon Hamdorf, the former Kansas Medicaid director, as its market president. UCare is a nonprofit health plan that will bid on the upcoming KanCare procurement. A request for proposals is expected to be released in 2023. Read More
Louisiana
Louisiana Governor Vetoes Part of Legislature’s Proposed Budget, Reinstates Health Spending Increase. The Associated Press reported on June 29, 2023, that Louisiana governor, John Bel Edwards, vetoed elements of the legislature’s proposed budget and restored a $100 million increase in funding for the Department of Health, which oversees the state’s Medicaid program. According to Edwards, this will prevent program cuts and a loss of up to $700 million in federal matching funds. Lawmakers can still override the vetoes. Read More
Maryland
Maryland Extends Pregnancy, Postpartum Medicaid Benefits to Undocumented Individuals. Maryland Governor Wes Moore announced on July 3, 2023, the availability of both pregnancy and four months of postpartum Medicaid coverage to undocumented individuals. The state also received approval to use Medicaid funds to pay for eligible community violence prevention services and to reimburse Certified Peer Recovery Specialists for substance use treatment services provided at Federally Qualified Health Centers. Read More
Maryland Obtains CMS Approval of 1332 Waiver Extension for Exchange Plan Reinsurance Program. The Centers for Medicaid & Medicare Services (CMS) announced on June 28, 2023, approval of a State Innovation 1332 Waiver Extension Request for Maryland’s reinsurance program for Exchange plans from January 1, 2024, through December 31, 2028. Read More
Massachusetts
Massachusetts Made $85 Million in Capitation Payments on Beneficiaries Living Out of State, Audit Finds. The Massachusetts Office of the State Auditor published on June 28, 2023, an audit that found MassHealth made nearly $85 million in capitation payments to Medicaid managed care organizations on behalf of beneficiaries living outside the state. The audit recommends MassHealth revise its policies and procedures regarding data matches for eligibility, investigate instances where data matches indicate a beneficiary is enrolled in another state’s Medicaid program, and provide beneficiaries with instructions for unenrolling if they move out of state. The audit covered January 1, 2018 through September 30, 2021. Read More
Minnesota
Minnesota Releases Medicaid, MinnesotaCare IHP RFP. The Minnesota Department of Human Services released on July 3, 2023, a request for proposals (RFP) for providers interested in participating in the state’s Integrated Health Partnerships (IHP) Demonstration, an accountable care model that serves Medicaid and MinnesotaCare. The program, which currently has 28 IHPs serving more than 520,000 beneficiaries, offers two tracks: Track 1 (non-risk) and Track 2 (upside and downside risk). Letters of intent are due August 28, and proposals are due September 8. The contract is anticipated to begin on January 1, 2024, and run through December 31, 2026, with a five-year extension option. Read More
Minnesota Provides One Month Grace Period to Reenroll in Medicaid Following June Redeterminations. The Minnesota Department of Human Services announced on June 29, 2023, that the state will give Medicaid enrollees a one-month grace period until August 1 to re-enroll in the program following June redeterminations. The additional time will benefit nearly 35,500 beneficiaries who had a July 1 deadline. Read More
Nevada
Nevada Allows Medicaid to Cover Behavioral Health Services in Schools. News 4 reported on June 29, 2023, that Nevada school districts will be able to bill Medicaid for services outside the Individualized Education Plan through a state plan amendment. The focus will be on early intervention, including mental, behavioral, social, emotional, and physical health. Read More
New Hampshire
Medicaid Beneficiaries Struggle to Find Dental Care. The New Hampshire Bulletin reported on July 5, 2023, that New Hampshire Medicaid beneficiaries are struggling to get dental appointments, with less than 15 percent of dentists and oral surgeons enrolling to accept Medicaid since the state began covering basic dental services for adults in April. About half of participating providers have set limits on patient volume. The state has seen an increase in dental claims from 1,000 in April to 2,000 in June. Read More
North Carolina
North Carolina Governor Urges Lawmakers to Separate Medicaid Expansion from Budget. North Carolina Governor Roy Cooper released on July 3, 2023, a statement urging lawmakers to separate implementation of Medicaid expansion from the state’s fiscal 2024 budget bill. The Medicaid expansion bill that was signed in March has a provision delaying implementation until the budget is adopted. Read More
Oklahoma
Oklahoma Disenrolls 54,000 Medicaid Enrollees During May Redeterminations. Ponca City Now reported on June 30, 2023, that Oklahoma has disenrolled approximately 54,000 Medicaid enrollees during the state’s May redeterminations and expects to disenroll an estimated additional 35,000 members on July 1. The state predicts that a total of over 270,000 beneficiaries will lose coverage over the course of the nine month redetermination period that began in May. Read More
South Dakota
South Dakota Implements Medicaid Expansion on July 1. The Centers for Medicare & Medicaid Services (CMS) announced on June 30, 2023, that South Dakota implemented Medicaid expansion coverage effective July 1, with more than 52,000 adults aged 19 to 64 eligible for coverage. Federal matching funds will cover 90 percent of the cost. Read More
U.S. Virgin Islands
U.S. Virgin Islands Extends Postpartum Medicaid Coverage. The Centers for Medicare & Medicaid Services announced on June 30, 2023, that the U.S. Virgin Islands received approval to extend postpartum Medicaid coverage to one year through a state plan amendment. Read More
Washington
Washington Receives Federal Renewal of Medicaid Transformation Project Section 1115 Waiver. The Washington State Health Care Authority announced on June 30, 2023, that federal regulators renewed the state’s Medicaid Transformation Project Section 1115 demonstration waiver, a delivery system transformation initiative, from July 1, 2023, through through June 30, 2028. Regulators approved new programs offering additional care for children, elderly, and those leaving correctional facilities; however, the state did not receive approval to use waiver funds to cover postpartum care for non-citizens. Read More
Washington Disenrolls 116,000 Medicaid Beneficiaries During May Redeterminations. The Washington State Healthcare Authority announced on June 30, 2023, that approximately 116,000 Medicaid beneficiaries were disenrolled during May redeterminations. Coverage was renewed for approximately 114,000 beneficiaries. May was the state’s first month of renewals. Read More
National
CMS Releases Revised Guidance for Medicare Drug Price Negotiation Program. The Centers for Medicare & Medicaid Services (CMS) released on June 30, 2023, revised guidance for the new Medicare Drug Price Negotiation Program, which includes additional opportunities for drug companies and members of the public to engage with CMS during the negotiation process. The first round of negotiations will occur during 2023 and 2024, with prices effective in 2026. Read More
Home Health Providers Face Proposed 2.2 Percent Medicare Rate Cut in Fiscal 2024. Modern Healthcare reported on June 30, 2023, that the Centers for Medicare & Medicaid Services (CMS) has proposed a 2.2 percent decrease in Medicare reimbursement rates for home health providers in fiscal 2024. CMS will accept comments on the proposal through August 29. Read More
Comments on CMS’s 2024 Hospital Inpatient Regulation Ask for Consideration of Rising Hospital Cost Trends. Modern Healthcare reported on June 30, 2023, that public comments submitted on the proposed fiscal 2024 Hospital Inpatient Prospective Payment System (IPPS) rule urge the Centers for Medicare & Medicaid Services (CMS) to consider rising cost trends, including inflation, labor shortages, and other pressures when finalizing the rule. The draft rule was published in April, with the final rule expected next month. Read More
MACPAC Voices Support of CMS Medicaid Managed Care Directed Payments, Medicaid Access Proposed Rules. The Medicaid and CHIP Payment and Access Commission (MACPAC) released two comment letters on June 30, 2023, supporting CMS’ Medicaid and Children’s Health Insurance Program (CHIP) Managed Care Access, Finance, and Quality proposed rule and the Ensuring Access to Medicaid Services proposed rule. MACPAC expressed support for broadening access monitoring and improving oversight of managed care directed payments, while suggesting that CMS clarify directed payment goals and develop a process to make approval documents and rate certifications publicly available. The commission also supports ensuring that Medicaid provides access to services by increasing payment rate transparency, standardizing reporting, and promoting beneficiary engagement. However, it recommends CMS consult with states about a realistic timeline for the proposed changes given the ongoing Medicaid unwinding activities.
CMS Rejects GAO Recommendation to Examine Cost Effectiveness of Medicaid Managed Care. Health Payer Specialist reported on June 29, 2023, that the Centers for Medicare & Medicaid Services (CMS) rejected Medicaid recommendations from a Government Accountability Office (GAO) report, including adding managed care plans to the Medicaid Recovery Audit Contractor program to examine their cost effectiveness. Currently, 16 states participate in the program. According to CMS, states should set up their own audits based on the specific needs of their programs. Read More
Department of Justice Charges Individuals for $2.5 Billion in Healthcare Fraud. The Hill reported on June 28, 2023, that the Department of Justice has charged 78 people for fraudulent claims to Medicare and other government insurance programs totaling $2.5 billion. The elderly and disabled were targeted through telemedicine and pharmaceutical schemes. California, Florida, Georgia, Indiana, Kentucky, Louisiana, Michigan, New Jersey, New York, Ohio, Pennsylvania, South Carolina, Texas, Washington, and Wisconsin are prosecuting the cases. Read More
Industry News
Molina to Acquire Bright Health Medicare Advantage Subsidiaries. Molina Healthcare announced on June 30, 2023, a definitive agreement to acquire Bright Health Company of California subsidiaries Brand New Day and Central Health Plan of California for approximately $510 million. Both companies combined provide Medicare Advantage coverage to approximately 125,000 members. Read More
Addus HomeCare to Acquire Tennessee Quality Care. Addus HomeCare Corporation announced on June 29, 2023, a definitive agreement to acquire Tennessee Quality Care, a home health, hospice, and private duty nursing service provider. Tennessee Quality Care has 17 locations across 50 Tennessee counties. The transaction is expected to close in the third quarter of 2023. Read More
Autism Behavioral Institute Receives Funding from Decathlon Capital Partners. Behavioral Health Business reported on June 29, 2023, that Autism Behavioral Institute, an applied behavioral analysis provider, will receive revenue-based funding from Decathlon Capital Partners. Autism Behavioral Institute will use the funding to expand into new markets and add new payer partners. Read More
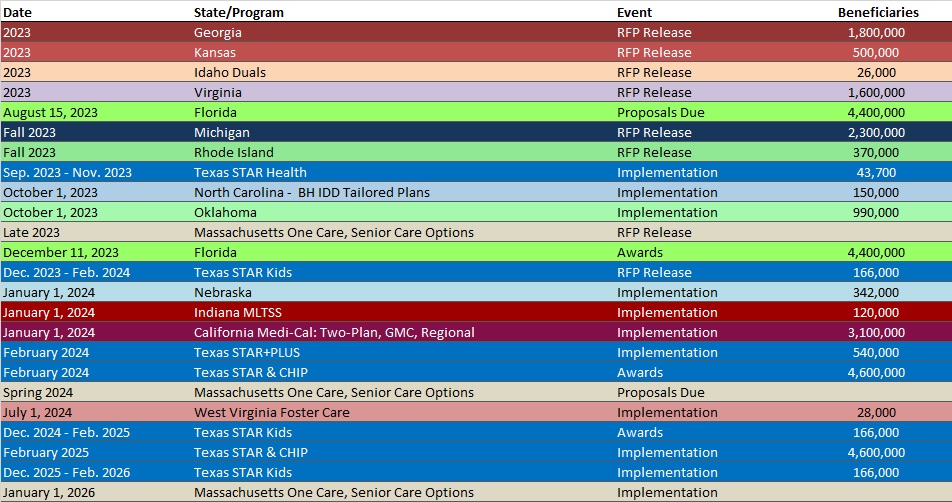
RFP Calendar
Company Announcements
MCG White Paper:
An Evidence-Based Approach to Emergency Department Patients with Intermediate-Risk Chest Pain. In this new white paper download, MCG Health’s Associate Vice President and Managing Editor, William Rifkin, MD, FACP, explores an evidence-based approach to emergency department (ED) patients presenting with intermediate-risk chest pain. Topics covered include: (1) Appropriate risk assessment; (2) Next steps for intermediate-risk patients; and (3) Revascularization vs. Medical Therapy. Read More
HMA News & Events
Upcoming HMA Webinar:
Medicaid 1115 Justice Waiver Opportunities: Medication Assisted Treatment for Substance Use Disorder in Carceral Settings. HMA’s webinar series, 1115 Medicaid Justice Demonstration Waivers: Bridging Healthcare, focuses on helping stakeholders optimize care for persons in carceral settings and during their transition back to the community. Part 4 will focus on access to medication assisted treatment (MAT) for substance use disorder (SUD) during and after transition from a carceral setting into the community, to ensure continuity of care for those leaving incarceration to reduce overdose and recidivism. Click here to register.
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- California Medicaid Managed Care Enrollment is Up 6.5%, Mar-23 Data
- Georgia Medicaid Managed Care Enrollment is Up 0.8%, Jul-23 Data
- Maryland SNP Membership at 30,324, Mar-23 Data
- Nebraska SNP Membership at 17,461, Mar-23 Data
- New Jersey SNP Membership at 86,971, Mar-23 Data
- New York Medicaid Managed Care Enrollment is Up 1.4%, Mar-23 Data
- Ohio SNP Membership at 174,736, Mar-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Minnesota Medical Assistance, MinnesotaCare Integrated Health Partnerships RFP, Jul-23
- Ohio Medicaid Enterprise System Alternate Payment Model Logic and Reporting Tool RFP, Jun-23
Medicaid Program Reports, Data, and Updates:
- New Mexico PHE Medicaid Redeterminations Monthly Reports to CMS, May-23
- Washington Apple Health Medicaid Redeterminations Data Report, Jun-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
