HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: CMS Releases National Healthcare Expenditure and Enrollment Projections through 2031

- May Medicaid Redeterminations Update: Arizona, Illinois, Indiana, Iowa, West Virginia

- California Lawmakers Introduce Bills to Modernize State Mental Health Services Act

- Florida to Pilot Medicaid Managed Care for Individuals with Developmental Disabilities in 7 Counties

- Idaho Releases EQRO RFP

- Illinois Pauses Enrollment in Health Benefits for Immigrant Adults Program

- Indiana Names Cora Steinmetz as Medicaid Director

- Iowa Contracts With HMA to Study Service Delivery for New Health, Human Services Department

- Kentucky to Study Potential HCBS Waiver Program For Children with Severe Emotional, Intellectual Disabilities

- Montana Disenrolls 15,500 Medicaid Beneficiaries During April Redeterminations

- New Mexico Awards General Dynamics Information Technology $39 Million Contract to Update Medicaid Provider Enrollment System

- Oklahoma Closed Loop Electronic Referral System for SDOH RFP Responses Are Due June 19

- Tennessee Releases Medicaid, CHIP Eligibility Determination System RFI

- Enhanced Medicaid Funds to States for Pausing Disenrollment Top $117 Billion, KFF Finds

- Pennant Group Acquires Bluebird Home Health, Hospice, Home Care Provider

In Focus
CMS Releases National Healthcare Expenditure and Enrollment Projections through 2031
This week, our In Focus section reviews the projected healthcare expenditure and enrollment data from the Centers for Medicare & Medicaid Services (CMS) Office of the Actuary, published June 14, 2023. The Office of the Actuary provides annual updates to historical and projected National Health Expenditure data on Medicare, Medicaid, CHIP, and other public insurance programs, as well as commercial healthcare insurance.
CMS projects that the average annual growth for national healthcare spending from now through 2031 will be 5.4 percent. CMS estimated that the number of insured individuals in the United States was projected to reach a high of 92.3 percent in 2022 and would decrease to 90.5 percent by 2031. CMS projects 93.6 million Medicaid and CHIP members will account for more than $1.2 trillion in annual spending in 2031 and that 76.4 million Medicare beneficiaries will account for more than $1.8 trillion in expenditures that year. A summary of other key takeaways from the actuarial report follows.
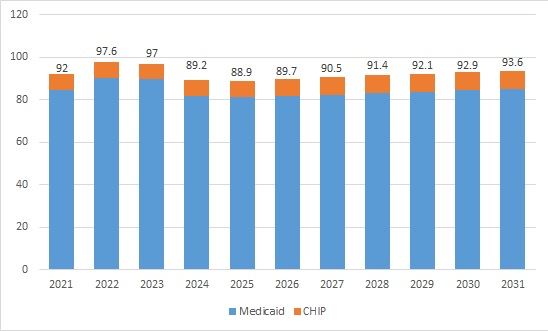
Enrollment Projections
Approximately 92 million people were enrolled in Medicaid and CHIP programs in 2021. Enrollment is projected to have reached a high of 97.6 million in 2022 and is expected to fall between 2023 and 2026 because of Medicaid redeterminations. CMS projects the largest loss in 2024, with 8 million people leaving Medicaid and CHIP that year alone. By 2026, enrollment is projected to hit a low of 89.7 million and start to rise back up in the subsequent years until reaching 93.6 million enrollees in 2031.
Table 1. Historical and Projected Medicaid/CHIP Enrollment (in Millions)
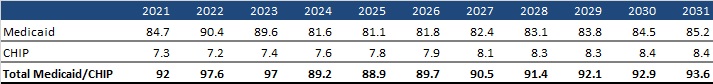
Figure 1. Historical and Projected Medicaid/CHIP Enrollment (in Millions)
Medicare enrollment is projected to continue growing steadily. CMS estimates that Medicare beneficiaries totaled 63.6 million in 2022. By 2031, Medicare enrollment is expected to climb to 76.4 million.
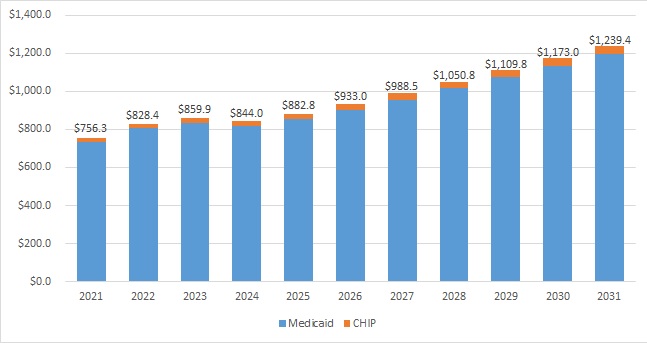
Expenditure Projections
Medicaid expenditures are expected to grow by 5 percent on average in 2022−2031. In 2022, the Medicaid annual growth rate was projected to be −2.1 percent. Following the public health emergency unwinding, average expenditure growth would pick up to 5.6 percent in 2025−2031.
CMS estimated that total Medicaid and CHIP annual spending in 2022 was $828.4 million; by 2031, it is projected to hit $1.2 trillion. For context, private health insurance is projected to reach nearly $2.1 trillion in 2031.
Table 2. Historical and Projected Medicaid/CHIP Expenditures (in Billions)
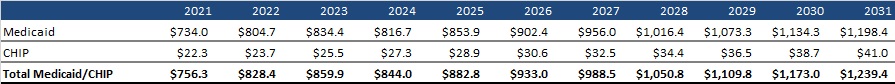
Figure 2. Historical and Projected Medicaid/CHIP Expenditures (in Billions)
Medicare spending is projected to grow to more than $1.8 trillion in 2031 from $944.2 million in 2022. During this time, average annual expenditure growth is projected to be 7.5 percent. In 2022, spending growth dropped to 4.8 percent compared with 8.4 percent in 2021 because fee-for-service beneficiaries were using fewer emergency department services and as a result of reinstated payment rate cuts associated with the Medicare Sequester Relief Act of 2022.
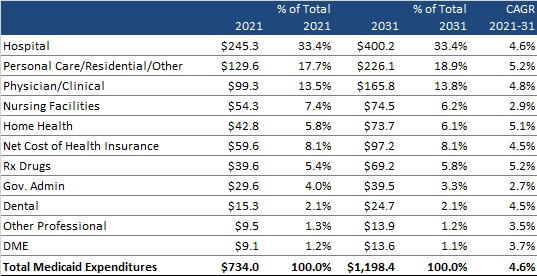
Medicaid Expenditure Projections by Category
CMS provides a historical and projected breakdown of expenditures by category for Medicaid only (CHIP is bundled with Department of Defense and other public spending). Table 3 summarizes the projected change in annual expenditures for several categories of services and other expenditures. It also shows each category’s percentage contribution to total Medicaid expenditures and the compounded annual growth rate (CAGR) in 2021−2031 for each category of spending. Hospital spending, personal care/residential/other, and physician/clinical expenditures are projected to continue to be the largest contributors to overall Medicaid expenditures, together equaling approximately 65 percent of total expenditures in 2021 and a projected 66 percent in 2031.
Table 3. Historical and Projected Medicaid-Only Expenditures by Category, 2021-2031 (in Billions)
HMA Roundup
Arizona
May Medicaid Redeterminations Update: Arizona, Illinois, Indiana, Iowa, West Virginia. The following states have released May redeterminations reports: Arizona, Illinois, Indiana, Iowa, and West Virginia.
- Arizona disenrolled nearly 72,500 Medicaid beneficiaries during the May redeterminations period. The state renewed coverage for about 129,400 beneficiaries.
- Illinois initiated renewals for about 203,800 Medicaid beneficiaries during the May redeterminations period. The state has not begun disenrolling or renewing coverage.
- Indiana disenrolled almost 54,000 Medicaid beneficiaries during the May redeterminations period. The state renewed coverage for nearly 66,000 beneficiaries.
- Iowa disenrolled about 7,000 Medicaid beneficiaries during the May redeterminations period. The state renewed coverage for almost 30,000 beneficiaries.
- West Virginia disenrolled about 25,000 Medicaid beneficiaries during the May redeterminations period. The state renewed coverage for about 21,500 beneficiaries.
California
California Lawmakers Introduce Bills to Modernize State Mental Health Services Act. The Sacramento Bee reported on June 20, 2023, that the California legislature is considering bills (SB 326 and AB 531) sponsored by Senator Susan Talamantes Eggman (D-Stockton) and Assembly Member Jacqui Irwin (D-Thousand Oaks) to modernize the Mental Health Services Act for individuals with serious mental illness and substance use disorders. The proposal would cost almost $4.7 billion and would reform behavioral healthcare funding, focus on outcomes, and provide housing and treatment services in community-based settings. Governor Gavin Newsom has stated his support for the legislation. Read More
California Requests New 1115 Waiver for Reproductive Health Access. The Centers for Medicare & Medicaid Services announced on June 16, 2023, that California submitted a request for a new Section 1115 waiver, the California Reproductive Health Access Demonstration, to improve access to reproductive health care providers for Medi-Cal beneficiaries and other individuals facing access barriers. The federal public comment period is open until July 16. Read More
Delaware
Delaware Extends Postpartum Medicaid Coverage to One Year. The Coastal Point reported on June 20, 2023, that Delaware extended postpartum Medicaid coverage from 60 days to 12 months through a State Plan Amendment, which received federal approval in May. The extension is retroactive to July 2022. Medicaid covers about 41 percent of births in Delaware. Read More
Florida
Florida to Pilot Medicaid Managed Care for Individuals with Developmental Disabilities in 7 Counties. Health News Florida reported on June 19, 2023, that Florida Governor Ron DeSantis signed legislation to pilot Medicaid managed care for individuals with developmental disabilities in seven counties: Miami-Dade, Monroe, Hardee, Highlands, Hillsborough, Manatee, and Polk counties. Enrollment is anticipated to begin by January 31, 2024. Read More
Florida to Establish Medicaid Sickle Cell Disease Registry. Florida Politics reported on June 19, 2023, that Florida Governor Ron DeSantis signed legislation requiring the state Agency for Health Care Administration to establish a sickle cell disease registry to better track screening results and outcomes, especially among infants. There were approximately 7,300 Medicaid beneficiaries with sickle cell disease in Florida in 2022. Read More
Florida Governor Signs Fiscal 2024 Budget With $625 Million to Support Behavioral Health, Crisis Services. Health News Florida reported on June 16, 2023, that Florida Governor Ron DeSantis signed a fiscal 2024 budget, including $625 million to support behavioral health and 988 Suicide and Crisis Lifeline services. The budget also includes $290 million to improve prenatal and postpartum care, $3.8 million in premium assistance for families receiving KidCare who were impacted by Hurricane Ian, and $54 million for stand-alone children’s hospitals serving Medicaid beneficiaries. Read More
Idaho
Idaho Releases EQRO RFP. The Idaho Department of Health and Welfare released on June 15, 2023, a request for proposals for a Medicaid external quality review organization (EQRO). The contract will run from August 21, 2023, through August 20, 2027. Proposals are due July 19. External quality reviews are required for Idaho’s behavioral health prepaid ambulatory health plan (PAHP), dental PAHP, and managed care plans serving dual eligibles. The current Idaho EQRO is Telligen. Read More
Illinois
Illinois Pauses Enrollment in Health Benefits for Immigrant Adults Program. Health News Illinois reported on June 20, 2023, that the Illinois Department of Healthcare and Family Services is pausing enrollment in the Health Benefits for Immigrant Adults program, effective July 1, citing rising costs. The program covers individuals aged 42 and older not eligible for Medicaid because of citizenship status. Enrollment in the Health Benefits for Immigrant Seniors program, which covers individuals 65 and older, will remain open but capped at 16,500. Read More
Illinois Increases Medicaid Reimbursement Rates for Providers. Health News Illinois reported on June 20, 2023, that Illinois Governor JB Pritzker signed an omnibus bill raising Medicaid rates 30 percent for substance use disorder treatment, 12 percent for nursing homes, and 10 percent for hospitals. The law also provides an additional $50 million annually for federally qualified health centers. Most of the rate increases will be implemented in January 2024. Read More
Auditor Recommends More Detailed Monitoring of MCOs, PBMs. Health News Illinois reported on June 15, 2023, that the Illinois Office of the General Auditor recommended that state regulators improve monitoring of managed care organizations (MCOs) and their pharmacy benefit managers (PBMs). The audit recommends that the state Department of Healthcare and Family Services monitor reimbursement rates; address conflicts of interest between MCOs, PBMs, and pharmacies; and regularly report to the state legislature. Read More
Indiana
Indiana Names Cora Steinmetz as Medicaid Director. The Indiana Capital Chronicle reported on June 20, 2023, that Cora Steinmetz has been named Medicaid director for the Indiana Family and Social Services Administration (FSSA). Steinmetz will succeed Allison Taylor, who is leaving this summer after eight years on the job. Steinmetz is currently senior operations director for health-related state agencies for Governor Eric Holcomb. Read More
Iowa
Iowa Contracts With HMA to Study Service Delivery for New Health, Human Services Department. The Gazette reported on June 20, 2023, that the Iowa Department of Health and Human Services has contracted with Health Management Associates (HMA) to study access and care delivery for programs under its newly merged health and human services department. The department is hoping to identify gaps and duplication of services, improve access, better utilize funding, and improve community-based work. Recommendations are expected in October. Read More
Kentucky
Kentucky Increases Medicaid Reimbursement Rates for HCBS, Long-term Care Facilities. The Commonwealth Journal reported on June 15, 2023, that Kentucky increased Medicaid reimbursement rates for home and community-based services (HCBS) and long-term care facilities. Long-term care facilities will receive an additional $99.6 million in fiscal 2024. The HCBS adjustment will be for services that were delivered from January 1, 2022, to May 1, 2023, at an additional cost of $13 million. Read More
Kentucky to Study Potential HCBS Waiver Program For Children with Severe Emotional, Intellectual Disabilities. The Kentucky Cabinet for Health and Family Services announced on June 15, 2023, that it will conduct a feasibility study for a potential Medicaid home and community-based services (HCBS) program serving children with severe emotional disabilities or intellectual disabilities and related conditions like autism spectrum disorder. Responses are due on July 2. Read More
Louisiana
Louisiana Health Secretary Outlines Impact of Proposed Budget Cuts Before State Senate Committee. The Times-Picayune/The New Orleans Advocate reported on June 20, 2023, that services for individuals who are elderly or have behavioral health issues could be reduced by up to $700 million in state and federal funds because of budget cuts proposed this month, according to Louisiana Department of Health secretary Stephen Russo in testimony before the Senate Health and Welfare Committee. The reduction in state funds to the department totals $100 million. Read More
Montana
Montana Disenrolls 15,500 Medicaid Beneficiaries During April Redeterminations. The Montana Free Press reported on June 20, 2023, that Montana disenrolled about 15,500 Medicaid beneficiaries during April redeterminations. About 72 percent were disenrolled for failing to provide requested information. The state renewed coverage for about 9,100 beneficiaries. Read More
Montana Increases Medicaid Reimbursement Rates for Providers. The Montana Free Press reported on June 14, 2023, that Montana Governor Greg Gianforte signed a budget bill that includes increasing Medicaid reimbursement rates for providers. According to an analysis from the Legislative Fiscal Division, the rate increases will require an increase of $339.4 million in combined state and federal funds for fiscals 2024 and 2025. Read More
New Mexico
New Mexico Awards General Dynamics Information Technology $39 Million Contract to Update Medicaid Provider Enrollment System. StateScoop reported on June 20, 2023, that the New Mexico Human Services Department awarded General Dynamics Information Technology a $39 million contract to replace the Medicaid system for provider enrollment, credentialing, training, and reporting. The new system is expected to be implemented by the third quarter of 2024, and the contract lasts for four years with the option for four more. Read More
New Mexico Surveys Rural Providers Looking for Funds to Expand Clinical Services. The New Mexico Human Services Department announced on June 15, 2023, it is surveying rural health care providers interested in developing or expanding clinical services, with $80 million allocated to the initiative. The surveys will show the scope of services needed in communities and how many facilities and providers may apply for funding. Survey responses are due July 30 and applications will open in September. Read More
North Carolina
North Carolina to Receive $1 Billion in Additional Federal Funds from Medicaid Expansion. North Carolina Public Radio reported on June 14, 2023, that North Carolina will receive $1 billion in additional federal funds from Medicaid expansion. The state House is considering a budget bill that would use about 25 percent of the funds to increase Medicaid reimbursement rates for mental health providers. The state Senate has a budget bill that directs the money to be spent on other health care projects, including new hospital construction and new health sciences training facilities at community colleges and universities. The final budget agreement will be released in the next few weeks. Read More
Oklahoma
Oklahoma Closed Loop Electronic Referral System for SDOH RFP Responses Are Due June 19. The Oklahoma Healthcare Authority released a request for proposals (RFP) for a Closed Loop Electronic Referral System (CLERS) to address social determinants of health (SDOH), with responses due on June 19, 2023. Unite Us is the incumbent. Read More
Tennessee
Tennessee Releases Medicaid, CHIP Eligibility Determination System RFI. The Tennessee Department of Finance and Administration released on June 9, 2023, a request for information (RFI) for a Medicaid and Children’s Health Insurance Program (CHIP) eligibility determination system. Deloitte is the current incumbent. Responses are due on August 8. Read More
Texas
Texas Extends Medicaid Postpartum Coverage to One Year. CNN reported on June 18, 2023, that Texas Governor Greg Abbott signed House Bill 12, extending Medicaid postpartum coverage from 60 days to one year. Extended Medicaid coverage is not available for women who terminate their pregnancy through elective abortion. Read More
National
MedPAC Recommends Addressing Price of Medicare Part B Drugs, Telehealth Rates in Report to Congress. MHealth Intelligence reported on June 20, 2023, that the Medicare Payment Advisory Commission (MedPAC) released its 2023 report to Congress, which recommends capping the payment rate for Medicare Part B drugs under the accelerated approval program and establishing a payment rate for groups of similar drugs. The report also recommends monitoring the impact of telehealth on healthcare access, quality, and cost. Read More
Enhanced Medicaid Funds to States for Pausing Disenrollment Top $117 Billion, KFF Finds. Kaiser Family Foundation (KFF) reported on June 16, 2023, that states received over $117 billion in enhanced federal funding after pausing Medicaid disenrollments during the public health emergency (PHE), according to a KFF analysis. The analysis also found that non-expansion states, which account for only 22 percent of Medicaid spending, received 27 percent of the funding. Read More
Application Period for FFS Medicare Shared Savings Program ACOs Closes. Modern Healthcare reported on June 16, 2023, that the 2024 provider application period has closed for fee-for-service (FFS) Medicare Shared Savings Program accountable care organizations (ACOs). The Centers for Medicare & Medicaid Services wants all Medicare beneficiaries to be served by value-based programs by 2030. Read More
Breakdowns of Opioid Settlement Payouts to Local Governments Are Made Public. KFF Health News reported on June 16, 2023, that breakdowns of specific opioid settlement payout amounts to local governments in 2022 and 2023 have been made public. KFF Health News spearheaded the effort to obtain the records. Read More
MACPAC Recommends Automatic Adjustments for DSH Payments to Offset FMAP Changes in June Report to Congress. The Medicaid and CHIP Payment and Access Commission (MACPAC) recommended on June 15, 2023, automatic adjustments to disproportionate share hospital (DSH) payments so DSH funding would not change as a result of fluctuations in state federal matching rates. MACPAC made the recommendation in its June report to Congress on Medicaid and the Children’s Health Insurance Program. MACPAC also reported on strategies to make integrated care the standard for dual eligibles, improving access to Medicaid coverage for individuals leaving carceral settings, and barriers to home and community-based services. Read More
Many States Use Member Surveys to Monitor Compliance with Network Adequacy Standards for MCOs, KFF Finds. Kaiser Family Foundation (KFF) released on June 15, 2023, a survey showing that 34 out of 37 responding Medicaid managed care states use member surveys to monitor compliance with network adequacy requirements. The survey also found that nine of 38 responding Medicaid managed care states issued penalties for non-compliance with network adequacy standards in the past three years, and many states have not yet altered requirements to account for telehealth. Read More
U.S. Senators Introduce Bill to Regulate PBMs, Lower Drug Costs for Medicare Part D Beneficiaries. Modern Healthcare reported on June 14, 2023, that U.S. Senators Robert Menendez (D-NJ) and Marsha Blackburn (R-TN) introduced a bill to the Senate Finance Committee that would ban pharmacy benefit managers (PBMs) from incorporating fees, rebates, and other costs into prescription drug prices for Medicare Part D plans. Read More
Industry News
University of Pittsburgh Medical Center, Washington Health System to Merge. Modern Healthcare reported on June 20, 2023, that not-for-profit University of Pittsburgh Medical Center (UPMC) and Washington Health System have signed a letter of intent to merge. The deal calls for Washington Health to be integrated into UPMC. Financial terms were not released. Read More
Pennant Group Acquires Bluebird Home Health, Hospice, Home Care Provider. The Pennant Group announced on June 16, 2023, the acquisition of Bluebird Home Health, Bluebird Hospice, and Bluebird Home Care in Idaho. Subsidiaries of the Pennant Group operate 98 home health and hospice agencies and 51 senior living communities nationwide. Read More
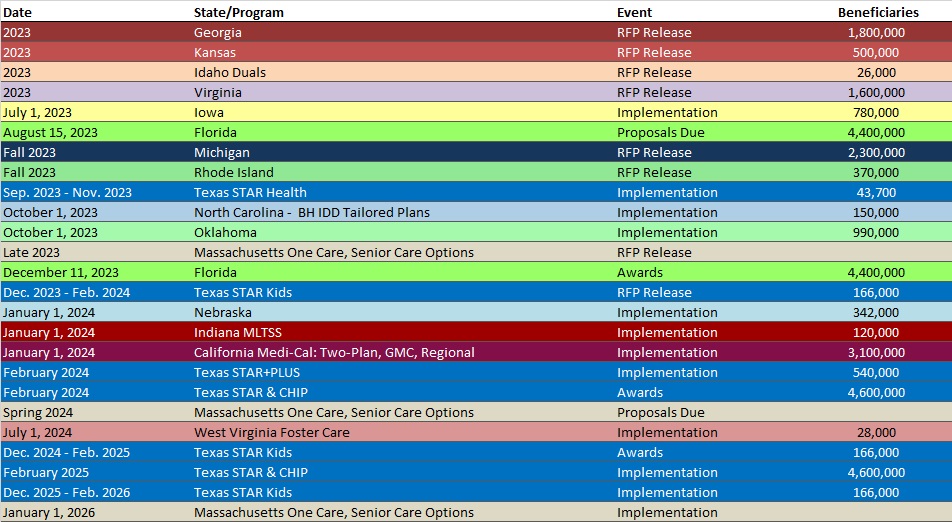
RFP Calendar
Company Announcements
Award-Winning Hospital to Speak on the Benefits of Artificial Intelligence at HFMA 2023 Conference. MCG Health will host experts from Mary Washington Healthcare at the HFMA 2023 Annual Conference (June 25-28, 2023) in Nashville, TN. The session will explore current hospital challenges and how the Mary Washington team successfully navigated these obstacles to reduce denials, improve hospital throughput, and apply unique AI technologies to optimize their utilization review workflow. Read More
HMA News & Events
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- Minnesota SNP Membership at 55,527, Mar-23 Data
- Mississippi Medicaid Managed Care Enrollment is Up 1.8%, May-23 Data
- North Carolina Medicaid Managed Care Enrollment is Up 2.4%, May-23 Data
- North Dakota Medicaid Expansion Enrollment is Up 5.3%, Apr-23 Data
- Texas SNP Membership at 456,989, Mar-23 Data
- Utah SNP Membership at 20,522, Mar-23 Data
- Virginia SNP Membership at 94,561, Mar-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- California CalAIM 1115 Demonstration Independent Evaluations RFI, Jun-23
- Idaho External Quality Review Organization RFP, Jun-23
- Oklahoma Closed Loop Electronic Referral System RFP, May-23
- Tennessee Eligibility and Determination System (TEDS) RFI, Jun-23
Medicaid Program Reports, Data, and Updates:
- Alaska Medicaid Enrollment Dashboard, May-23
- Arizona Medicaid Eligibility Renewals Dashboard, Jun-23
- Arkansas PHE Medicaid Redeterminations Monthly Report to CMS, May-23
- Idaho Medicaid Dental External Quality Reviews, 2019-22
- Idaho Medicaid IBHP External Quality Review Reports, 2019-22
- Idaho Medicaid Managed Care Quality Strategy Reports, 2018-23
- Idaho MMCP External Quality Review Reports, 2018-21
- Illinois Administration of Pharmacy Benefit Managers Performance Audit, May-23
- Illinois PHE Medicaid Redeterminations Baseline and Monthly Reports to CMS, May-23
- Indiana PHE Medicaid Redeterminations Monthly Report to CMS, May-23
- Iowa PHE Medicaid Redeterminations Monthly Report to CMS, May-23
- Kansas PHE Medicaid Redeterminations Monthly Report to CMS, May-23
- Mississippi PHE Medicaid Redeterminations Monthly Report to CMS, May-23
- North Dakota PHE Medicaid Redeterminations Monthly Report to CMS, May-23
- South Dakota DSS Medicaid Redeterminations Report, Apr-23
- West Virginia PHE Medicaid Redeterminations Monthly Report to CMS, May-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio at [email protected].
