HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: To Treat Residents with OUD, Nursing Facilities Must Improve Practices and Reduce Stigma

- Medicaid Disenrollment News: Arkansas, Georgia, Kansas, Maryland, Nebraska, New Hampshire, South Carolina

- Florida Raises KidCare Income Eligibility to 300 Percent of Poverty

- CareSource Files Protest Against Iowa Medicaid MCO Awards

- CareSource Forms Alliance with Three Organizations to Bid on Upcoming Kansas Procurement

- New York to Form Healthcare Commission to Improve Medicaid Quality, Reduce Costs

- North Carolina Enacts Law Allowing BCBS-NC, Delta Dental to Shift Assets to Holding Companies

- North Dakota Names Sarah Aker Medicaid Director

- Oklahoma Awards Medicaid Managed Care Contracts to Three Plans

- Pennsylvania Receives 67 Responses to Community HealthChoices RFI

- Texas Awards EVV System Management Services Contract to Accenture, HHAeXchange

- Health Plans Must Pay for Preventive Care Under Temporary Agreement

- CMS Announces New Primary Care Payment Model

- Center for Autism Files for Chapter 11, Assets To Be Acquired by Founder, Former CEO

- Walgreens Sells Remaining Shares of Option Care Health for $330 Million

In Focus
To Treat Residents with OUD, Nursing Facilities Must Improve Practices and Reduce Stigma
This week, our In Focus section highlights a Health Affairs Forefront post, “To Treat Residents With OUD, Nursing Facilities Must Improve Practices and Reduce Stigma,” published June 8, 2023. Health Management Associates (HMA) consultants Dina Besirevic, Kamala Greene Genece, Debbi Witham, David F. Polakoff, and Barry J. Jacobs wrote the article.
The HMA colleagues note that two recent healthcare industry trends are converging to change the admission criteria and clinical practices that some skilled nursing facilities (SNFs) use. Driving one movement is the opioid epidemic in which increased prevalence of fentanyl and its medical complications are spurring the need for posthospital discharge SNF admissions. The other stems from the low occupancy rates in many SNFs since the pandemic. As a result, more SNFs are considering filling beds by admitting individuals with opioid use disorder (OUD) for the first time.
In many respects, this a positive development. The need for skilled nursing care, such as medication-assisted treatment (MAT), for individuals with OUD has never been greater. A March 23, 2023, US Drug Enforcement Administration public safety alert reported that recently analyzed fentanyl samples in 48 of the 50 states had been adulterated with xylazine, or “tranq,” a veterinary sedative added to prolong an opioid high. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), extensive xylazine use commonly causes severe skin wounds requiring weeks of intravenous antibiotics and skilled wound care to prevent amputations. Providing well-managed post-acute care for these patients could lead to improved outcomes.
But admitting and treating individuals with OUD now poses multiple challenges for SNF staffs and administrators. Many of these healthcare workers lack training in OUD pharmacological and support care. Some have stigmatizing attitudes toward individuals with OUD. To address these concerns, SNFs across the country have developed different practice models. Examples include:
- Laguna Honda in San Francisco trains its staff to understand OUD, recognize the signs of resident opioid use, and work closely with nearby OUD providers to provide all OUD treatment.
- At Highbridge Woodycrest Center in the Bronx, NY, the storage and administration of MAT is managed by the SNF staff through a collaborative relationship with a community-based provider, Bronx Care Health System, which prescribes the medications and then delivers them to the facility.
- At other SNFs, SNF physicians and nurse practitioners prescribe buprenorphine with consultation as needed from community-based OUD providers.
HMA’s experts in OUD and SNFs are working collaboratively to assist SNFs interested in exploring the clinical, financial, and operational opportunities and challenges with this emerging line of business. For questions or inquiries, please contact Barry J. Jacobs.
HMA Roundup
Arkansas
Disenrollment News Arkansas Disenrolls Nearly 69,000 Medicaid Members During May Redeterminations. The Arkansas Department of Human Services announced on June 8, 2023, that Arkansas disenrolled 68,838 Medicaid beneficiaries following May eligibility redeterminations. More than 41,000 were disenrolled for failing to submit renewal forms or necessary information. Only 8,287 no longer met income thresholds. Total disenrollments over two months is 140,000. Read More
Connecticut
Connecticut Legislature Passes Amendment to Allow Medicaid Coverage of Community Health Worker Services. The CT Mirror reported on June 7, 2023, that the Connecticut legislature passed an amendment to Senate Bill 989, which would allow Medicaid to reimburse for services provided by community health workers. A committee previously passed two bills that would allow coverage for community health workers, but neither made it to the floor for a vote, so the provision was attached to a nursing home bill, SB 989. Read More
Florida
Florida Raises KidCare Income Eligibility to 300 Percent of Poverty. Florida Politics reported on June 13, 2023, that Florida Governor Ron DeSantis signed House Bill 121, which increases Florida KidCare eligibility to 300 percent of the federal poverty level from 200 percent, effective January 1, 2024. Florida KidCare is the umbrella brand for four state health insurance programs serving children: Medicaid, MediKids, Florida Healthy Kids, and the Children’s Medical Services Health Plan. Read More
Florida Medicaid Plans to Distribute Additional $181 Million in Enhanced Federal HCBS Funds. The Florida Agency for Health Care Administration announced on June 8, 2023, that it will provide an additional $181 million in one time payments to Medicaid managed care organizations to distribute to providers for non-waiver home and community-based services (HCBS). The funding will cover services provided from July 1, 2021, and June 30, 2022, for assistive care services, community behavioral health, durable Medicaid equipment, home health visit services, personal care services, and private duty nursing services. The funding is available through the American Rescue Plan Act HCBS Enhanced Funding Opportunity. Read More
Georgia
Georgia Disenrolls 1,659 Medicaid Beneficiaries During May Redeterminations. The Georgia Department of Community Health reported on June 8, 2023, the disenrollment of 1,659 Medicaid beneficiaries during May eligibility redeterminations. According to the state’s May report to the Centers for Medicare & Medicaid Services on the Medicaid unwinding process, the vast majority were disenrolled for procedural reasons, including failure to respond. Seventy-eight were determined ineligible and transferred to the Exchange. Between May and April, the state has disenrolled a total of 3,903 beneficiaries.
Idaho
Idaho Medicaid Spending Increases to $4.7 Billion Annually, With Growth Driven by Prescription Drugs. The Idaho Capital Sun reported on June 9, 2023, that Idaho Medicaid spending increased to $4.7 billion annually, according to the Idaho Department of Health and Welfare. Prescription drugs are one of the main drivers. Read More
Iowa
CareSource Files Protest Against Iowa Medicaid MCO Awards. The Iowa Capital Dispatch reported on June 13, 2023, that CareSource has filed a protest over the Iowa Medicaid managed care contracts awarded last year. Work on the contracts is expected to begin July 1. CareSource alleges a conflict of interest existed because the head of Molina’s Iowa plan was formerly state Medicaid director. Iowa awarded contracts to Molina and Elevance/Anthem. CVS/Aetna Better Health, CareSource, and UCare also submitted bids. Read More
Illinois
Illinois Settles Opioid Lawsuits With Drugmakers and Pharmacies for $518 Million. The Illinois Attorney General Kwame Raoul announced on June 9, 2023, that the state of Illinois has settled with drugmakers Teva and Allergan and pharmaceutical companies CVS and Walgreens for their role in the opioid crisis for a total of $518 million. The state will be paid this amount over 15 years. Read More
Kansas
CareSource Forms Alliance with Three Organizations to Bid on Upcoming Kansas Procurement. CareSource announced on June 7, 2023, that it has formed an alliance with three organizations to bid on the upcoming Kansas Medicaid managed care procurement for KanCare 3.0. The organizations are InterHab, Children’s Alliance of Kansas, and Association of Community Mental Health Centers of Kansas. Incumbents are Centene, CVS/Aetna, and United, serving approximately half a million beneficiaries. Elevance/Anthem in alliance with Blue Cross Blue Shield of Kansas also previously stated that it will be bidding. The RFP is expected to be released in the fall of this year. Contracts are worth $4 billion. Read More
Kansas Disenrolls 5,667 Medicaid Beneficiaries During Redeterminations. FOX 4 reported on June 14, 2023, that Kansas has disenrolled 5,667 Medicaid beneficiaries as of June 6. Another 45,820 beneficiaries have 90 days to finish submitting all the necessary forms. Read More
Kentucky
Kentucky Seeks IMD Exclusion Waiver for Short-term Stays for Individuals Experiencing Serious Mental Illness. The Centers for Medicare & Medicaid Services announced on June 14, 2023, that Kentucky has submitted an amendment to its Section 1115 KY HEALTH demonstration to pay for medically necessary short-term inpatient treatment services within institutions for mental diseases for Medicaid-eligible adults with serious mental illness (SMI). The amendment also requests approval to implement a pilot program providing medical respite services aimed at Medicaid adult beneficiaries who are homeless and need additional medical support and care coordination. The federal comment period is open until July 14, 2023. Kentucky is also preparing a Section 1915i waiver to request additional community support services to assist individuals with SMI, substance-use disorder, and health-related social needs. Read More
Maryland
Maryland Disenrolls 34,000 Medicaid Beneficiaries During May Redeterminations. The Frederick News-Post reported on June 13, 2023, that the Maryland Department of Health disenrolled approximately 34,000 Medicaid beneficiaries during May eligibility redeterminations. About 70 percent of those disenrolled were done so for procedural reasons. Read More
Nebraska
Nebraska Disenrolls 659 Medicaid Beneficiaries During May Redeterminations. The Nebraska Department of Health and Human Services reported on June 2, 2023, the disenrollment of 659 Medicaid beneficiaries during May redeterminations. According to the state’s unwinding report to the Centers for Medicare & Medicaid Services, 251 were disenrolled for procedural reasons and 408 were determined ineligible and transferred to the Exchange.
Nevada
Nevada Enacts Bill to Extend Medicaid Postpartum Coverage to One Year. The Nevada Current reported on June 13, 2023, that Nevada Governor Joe Lombardo signed Senate Bill 232 to extend Medicaid postpartum coverage from 60 days to one year. Medicaid covers 55 percent of the births in the state. Read More
New Hampshire
New Hampshire Disenrolls 45,000 During Medicaid Redeterminations. The Keene Sentinel reported on June 12, 2023, that New Hampshire has disenrolled more than 45,000 Medicaid beneficiaries following eligibility redeterminations. Medicaid enrollment in the state reached a high of 251,000 in March, but has since fallen to 199,000, according to state Medicaid director Henry Lipman. Most were disenrolled due to no longer being eligible, but thousands were also disenrolled due to procedural reasons. Read More
New Mexico
New Mexico Settles Opioid Lawsuit with Walgreens for $500 Million. Reuters reported on June 9, 2023, that Walgreens has agreed to pay the state of New Mexico $500 million to settle litigation related to the company’s role in the opioid crisis. New Mexico has recovered more than $1 billion in total settlements from opioid-related lawsuits. Read More
New York
New York Extends Medicaid Postpartum Coverage to One Year. The Centers for Medicare & Medicaid Services (CMS) announced on June 13, 2023, that New York extended Medicaid postpartum coverage from 60 days to 12 months. Up to 26,000 New Yorkers will be eligible for Medicaid for a full year after pregnancy. New York is the 35th state to expand postpartum coverage. Read More
New York to Form Healthcare Commission to Improve Medicaid Quality, Reduce Costs. The Empire Center for Public Policy reported on June 14, 2023, that New York Governor Kathy Hochul will form a healthcare commission to examine and recommend reforms to improve Medicaid quality and reduce costs, according to the state’s fiscal 2024 budget report. The report warned that Medicaid spending is currently expected to exceed the global cap due to higher-than-expected enrollment and utilization. Read More
North Carolina
North Carolina Enacts Law Allowing BCBS-NC, Delta Dental to Shift Assets to Holding Companies. The Associated Press reported on June 10, 2023, that North Carolina Governor Roy Cooper signed legislation allowing not-for-profit Blue Cross Blue Shield of North Carolina and Delta Dental to transfer surplus funds to holding companies run by company management. The law limits the amount that can be transferred to 25 percent of assets. Read More
North Dakota
North Dakota Names Sarah Aker Medicaid Director. North Dakota Health and Human Services announced on June 9, 2023, that Sarah Aker was named as director of the Medical Services Division, which oversees Medicaid and the Children’s Health Insurance Program. Aker will take over for interim Medicaid director Krista Fremming. Previously, Aker was the South Dakota Medicaid director. Read More
Oklahoma
Oklahoma Awards Medicaid Managed Care Contracts to Three Plans. The Oklahoma Health Care Authority announced on June 8, 2023, that it has awarded SoonerSelect Medicaid managed care contracts to Centene/Oklahoma Complete Health, CVS/Aetna, and Humana. Centene also won the children’s specialty program contract. Implementation will begin April 2024, with an initial term through June 30, 2024, with five renewal options. Oklahoma’s current Medicaid program, SoonerCare, is fee-for-service. Read More
Pennsylvania
Pennsylvania Receives 67 Responses to Community HealthChoices RFI. The Pennsylvania Department of Human Services Office of Long-Term Living reported on May 31, 2023, that it had received 67 responses to the Community HealthChoices (CHC) request for information (RFI), issued March 6, 2023. CHC is the state’s managed long-term services and supports program. The state will take the responses into consideration when developing the request for applications. Comments spanned a range of topics, including quality improvement for service coordination, covered services, workforce innovation, care integration across payers, person-centered planning, participant direction, quality improvement and transparency, program structure, and increased stakeholder input. Read More
South Carolina
South Carolina Receives Less Than a Third of Medicaid Eligibility Review Forms. The South Carolina Department of Health and Human Services announced on June 8, 2023, that only 30 percent of Medicaid beneficiaries returned eligibility review forms that the state sent out as part of the redeterminations process, which began April 1. Those that return their forms and are no longer eligible will have a 90-day eligibility grace period. Read More
Texas
Texas Awards EVV System Management Services Contract to Accenture, HHAeXchange. The Texas Health and Human Services Commission announced on June 13, 2023, that it has awarded the Electronic Visit Verification (EVV) System Management Services contract to Accenture State Healthcare Services. Accenture is working with EVV system vendor HHAeXchange, with the goal of transitioning to the new system by October 1, 2023. Current system vendors are DataLogic/Vesta and First Data/AuthentiCare. EVV will be required for Medicaid home healthcare services January 1, 2024. Currently it is required for Medicaid personal care services. Read More
Texas Legislature Passes Bill to Extend Medicaid Postpartum Coverage to One Year. KERA reported on June 9, 2023, that the Texas legislature passed House Bill 12 to extend Medicaid postpartum coverage from two months to one year, effective September 1. The bill awaits Governor Greg Abbott’s signature. Read More
Wisconsin
Wisconsin Awards $5.1 Million in Grants to Not-for-profit Dental Clinics. The Wisconsin Department of Health Services announced on June 12, 2023, that it has awarded $5.1 million in grants to 14 not-for-profit dental clinics in an effort to increase access for Medicaid beneficiaries, the uninsured, and individuals with disabilities. Read More
National
Health Plans Must Pay for Preventive Care Under Temporary Agreement. Modern Healthcare reported on June 13, 2023, that a federal appeals court approved an agreement that keeps in place Affordable Care Act mandates requiring health plans to cover preventive care at no cost to patients until the legal battle over the requirement plays out. Read More
HHS Announces New Flexibilities to Slow Medicaid Disenrollments. The U.S. Department of Health and Human Services (HHS) announced on June 12, 2023, new flexibilities to minimize the number of Medicaid and Children’s Health Insurance Program beneficiaries disenrolled during eligibility redeterminations. New flexibilities include allowing health plans to help Medicaid members complete renewal forms, allowing states to delay procedural terminations for one month to allow additional outreach, and allowing pharmacies and community-based organizations to facilitate reinstatement of coverage based on presumptive eligibility criteria. The flexibilities are noted in an HHS announcement and in a letter to state governors. Read More
Medicare to Fine Drug Makers for Price Hikes Outpacing Inflation on 43 Drugs. Reuters reported on June 9, 2023, that the Centers for Medicare & Medicaid Services will fine drug makers that increase prices on 43 Medicare drugs by more than the rate of inflation. Fines covering 27 drugs were imposed earlier this year. Read More
Chamber of Commerce Challenges Medicare Drug Negotiation Program in Federal Lawsuit. Reuters reported on June 9, 2023, that the U.S. Chamber of Commerce filed a federal lawsuit in Ohio, challenging the Medicare drug price negotiation program. Pharmaceutical company Merck is also seeking a federal injunction to block the program. Read More
States Turn to Dental Therapists to Increase Access to Oral Health for Underserved Populations. KFF Health News reported on June 9, 2023, that states are turning to dental therapists to increase access to oral care, specifically in underserved areas for rural residents, Medicaid beneficiaries, and Native Americans. Currently, over a dozen states license dental therapists, and eight are considering allowing licensure as well. Dental therapists offer basic oral care traditionally provided by dentists. Read More
Medicaid Beneficiaries in Nursing Homes Can Sue State Agencies, Supreme Court Rules. Modern Healthcare reported on June 8, 2023, that the U.S. Supreme Court upheld a ruling allowing Medicaid beneficiaries in nursing homes to sue state agencies for breaking federal law. The case, which now goes back to district court, involved a family suing Indiana-based Health and Hospital Corporation of Marion County. Read More
CMS Announces New Primary Care Payment Model. The Centers for Medicare & Medicaid Services (CMS) announced on June 8, 2023, that it will test its new Making Care Primary (MCP) payment model in eight states: Colorado, Massachusetts, Minnesota, New Jersey, New Mexico, New York, North Carolina, and Washington. The program provides payments to practices for building infrastructure, making primary care services more accessible, and better coordinating care with specialists. The MCP model will run from July 1, 2024, to December 31, 2034. Read More
HRSN Interventions Cost Double What Federal Programs Cover. Becker’s Payer Issues reported on June 6, 2023, that interventions for health related social needs cost on average $60 per person per month in primary care practices, of which only $27 is federally reimbursed, according to a study published in JAMA Internal Medicine. The study analyzed data from more than 19,000 patients who were seen at primary care practices between 2015 and 2018. Read More
Industry News
Center for Autism Files for Chapter 11, Assets To Be Acquired by Founder, Former CEO. The Wall Street Journal reported on June 12, 2023, that Blackstone-owned Center for Autism and Related Disorders (CARD) has filed for Chapter 11 bankruptcy protection and has agreed to sell substantially all its assets to founder and former chief executive Doreen Granpeesheh. Read More
Walgreens Sells Remaining Shares of Option Care Health for $330 Million. Modern Healthcare reported on June 9, 2023, that Walgreens has sold its remaining shares in Option Care Health for $330 million. In March, Walgreens sold $476.6 million worth of shares. Option Care Health and UnitedHealth Group are separately vying to acquire Amedisys. Read More
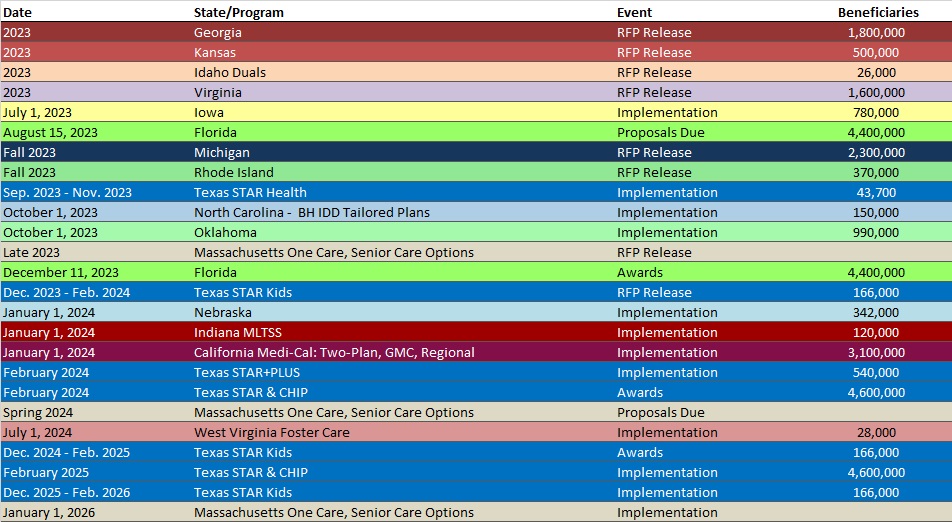
RFP Calendar
HMA News & Events
Upcoming HMA Webinars:
1115 Justice Waivers: Connecting Community Partners to Improve Transitions of Care. Part 3 of HMA’s webinar series, 1115 Medicaid Justice Demonstration Waivers: Bridging Healthcare, will focus on optimizing key partnerships before, during and after transition from a carceral setting into the community to ensure the best outcomes for individuals eligible for 1115 approved waiver services. Thursday, June 15, 2 pm ET. Click here to register.
Opportunities for State Regulators to Shape Policy and Regulation of Treatment for Substance Abuse Disorder. New federal regulations encourage significant changes to how opioid treatment is provided, with the goal of expanding access and improving patient-centered care. State regulators will need to adapt their regulatory practices and work closely with Medicaid agencies and treatment providers so the new regulations can achieve their intended goals. This webinar will discuss how State Opioid Treatment Authorities (SOTAs), licensing entities, and state Medicaid agencies will need to work together to craft updated regulations, facility licensing, and reimbursement practices that advance person-centered care. Tuesday, June 20, 3 pm ET. Click here to register.
Wakely, an HMA Company, White Paper:
The Impact of Social Risk Factors on Medicare Star Rating Performance: Differentiation in HEDIS and Medication Adherence Performance. With the release of the Contract Year 2024 Policy and Technical Changes to the Medicare Advantage and Medicare Prescription Drug Benefit Programs Final Rule on April 5, 2023, CMS has outlined changes in the Star Rating program intended to incentivize MAOs to focus on improving care for enrollees with social risk factors. This whitepaper examines the variation in Stars measure performance between enrollees with and without social risk factors. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
Medicaid Enrollment:
- California SNP Membership at 494,112, Mar-23 Data
- Georgia Medicaid Managed Care Enrollment is Up 1.6%, Jun-23 Data
- Illinois SNP Membership at 23,135, Mar-23 Data
- Iowa SNP Membership at 36,943, Mar-23 Data
- Kansas SNP Membership at 22,852, Mar-23 Data
- Kentucky SNP Membership at 87,070, Mar-23 Data
- Maine SNP Membership at 36,458, Mar-23 Data
- New York SNP Membership at 555,478, Mar-23 Data
- North Carolina SNP Membership at 174,713, Mar-23 Data
- Oregon Medicaid Managed Care Enrollment is Up 2.9%, May-23 Data
- Oregon SNP Membership at 42,342, Mar-23 Data
- South Carolina SNP Membership at 94,375, Mar-23 Data
- Wisconsin SNP Membership at 87,537, Mar-23 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Pennsylvania Community HealthChoices RFI and Responses, 2023
Medicaid Program Reports, Data, and Updates:
- Arkansas Health and Opportunity for Me (ARHOME) Waiver Documents, 2021-23
- Florida PHE Medicaid Redeterminations Monthly Report to CMS, Apr-23
- Georgia PHE Medicaid Unwinding Monthly Report to CMS, May-23
- Kentucky HEALTH Section 1115 Demonstration Waiver Documents, 2020-23
- Nebraska PHE Medicaid Unwinding Monthly Report to CMS, May-23
- New Hampshire PHE Medicaid Redeterminations Monthly Reports to CMS, Apr-23
- New Hampshire Medicaid Redeterminations Presentation, May-23
- New Mexico External Quality Review Reports, 2016-21
- New York Enacted Budget Financial Plan, FY 2024
- Texas Timeline for Transition to HHAeXchange EVV System, Jun-23
- Texas Medicaid PHE Unwinding Operational Plan, Jun-23
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
