HMA Weekly Roundup
Trends in Health Policy
This week's roundup:
- In Focus: Staying Ahead of the Star Rating Curve – A Case Study

- California Lawmakers Pass Spending Proposal to Increase Medi-Cal Reimbursement Rate for Doula Coverage

- Montana Medicaid Director Has ‘Not Had Conversations’ Regarding a Potential Transition to Managed Care

- North Carolina Foster Care Carve-Out Bill Faces Obstacles

- Ohio Medicaid Plan to Offer Members Access to Walgreens Health Corner

- CMS Approves 12-Month Postpartum Medicaid Coverage in District of Columbia, Maine, Minnesota, New Mexico

- Pharmaceutical Company to Pay $233 Million in Medicaid Fraud Settlement

In Focus
Staying Ahead of the Star Rating Curve – A Case Study
This week, our In Focus section highlights a presentation from HMA and Wakely, an HMA company, titled “Staying Ahead of the Star Rating Curve – A Case Study,” which was given at the 12th Medicare Stars, HEDIS, Quality Assurance, & Risk Adjustment Summit on June 15, 2022.
The presentation provided an overview of major changes in the Medicare stars program, which will result in both higher ratings and significantly higher revenues for many Medicare Advantage plans in 2023. However, the presentation indicated the higher ratings reflect temporary changes and not necessarily improvements in quality, adding that Medicare Advantage plans should be cautious about enhancing future benefits based on additional 2023 revenues.
Click here to view the presentation.
For questions please contact Linda Lee, Managing Principal; Christina Byrne, ASA, Consulting Actuary; Ann Pogrebitskiy, ASA, Associate Actuary.
HMA Roundup
California
Lawmakers Pass Spending Proposal to Increase Medi-Cal Reimbursement Rate for Doula Coverage. Kaiser Health News reported on June 21, 2022, that California lawmakers passed a spending proposal, which includes increasing Medi-Cal rates for doulas from an initially proposed $450 per birth to $1,154. Coverage would take effect in January 2023. The bill now heads to Governor Gavin Newsom for signature. Read More
Delaware
Senate Committee Advances Bills to Extend Postpartum Medicaid Coverage to One Year, Mandate Coverage of Annual Mental Health Exams. Delaware Public Media reported on June 15, 2022, that the Delaware Senate Health and Human Services committee advanced a bill that would extend postpartum Medicaid coverage from 60 days to one year. The committee also advanced a bill that would require insurance providers to cover annual mental health checkups. Read More
Florida
Florida Long-Term Managed Care Complaints Increased in May 2022. Florida Politics reported on June 15, 2022, that the Florida Agency for Health Care Administration received 312 calls complaining about the state’s Medicaid long term care program, continuing a trend of increasing calls over the last three months. A majority of the complaints from Medicaid beneficiaries related to problems accessing medical, dental, or transportation benefits. Complaints from providers related to claims processing issues and disputes between providers and plans. Read More
Kentucky
Kentucky Announces Comment Period for Supports for Community Living Waiver Renewal. The Kentucky Department of Medicaid Services announced on June 17, 2022, a public comment period for renewal of the state’s Supports for Community Living 1915(c) home and community-based services (HCBS) waiver. The comment period runs from June 24 to July 24. The current waiver, which is one of Kentucky’s six 1915 HCBS waivers, expires this year. Read More
Lousiana
Louisiana Extends Dental Coverage to Medicaid Beneficiaries in Intermediate Care Facilities. The Center Square reported on June 17, 2022, that Louisiana Governor John Bel Edwards signed legislation to extend Medicaid dental coverage to individuals with developmental disabilities aged 21 or older in state-licensed intermediate care facilities. The change requires approval from the Centers for Medicare & Medicaid Services and an appropriation from the state legislature.
Massachusetts
Massachusetts to Receive $4.6 Million in Medicaid Settlement with Health Plan, Mental Health Subsidiary. The U.S. Attorney’s Office announced on June 21, 2022, that Molina Healthcare and its previously owned mental health subsidiary, Pathways of Massachusetts, will pay $4.6 million to settle allegations that it submitted improper Medicaid claims, among other allegations. Molina owned and operated Pathways of Massachusetts between November 2015 and March 2018. Read More
Montana
Medicaid Director Has ‘Not Had Conversations’ Regarding a Potential Transition to Managed Care. The Montana Free Press reported on June 15, 2022, that Montana Medicaid director Mike Randol told state lawmakers that he has “not had conversations with anyone relative to transitioning Montana to managed care.” Randol, who made the remark during an interim health budget committee meeting, faced questions about a potential transition from several lawmakers, given his experience working in Medicaid managed care states. Instead, he said his immediate priorities included Medicaid reimbursement rates and working on ensuring eligible individuals remain covered when the public health emergency ends. Read More
North Carolina
North Carolina Foster Care Carve-Out Bill Faces Obstacles. The Winston-Salem Journal reported on June 20, 2022, that a bill to carve out foster care services from Medicaid behavioral managed care plans is unlikely to pass the state House during the 2022 legislative session, according to Representative Donny Lambeth (R-Winston-Salem). The Senate passed a version of the bill, including changes from an earlier House version. Read More
Senate Passes Bill to Carve-Out Foster Care Services from Managed Care. The Winston-Salem Journal reported on June 17, 2022, that the North Carolina Senate passed a bill (House Bill 144) that would carve-out foster care services from Medicaid behavioral managed care plans to prepaid health plans operated by health insurers. The bill will now go back to the House to accept or reject changes in the Senate version. Read More
Ohio
Ohio Medicaid Plan to Offer Members Access to Walgreens Health Corner. Walgreens Health announced on June 21, 2022, that eligible members of Centene/Buckeye Health Plans will have access to screenings and other services offered at Walgreen Health Corner locations in northeast Ohio. Walgreens has similar arrangements with two other payers serving commercial members in California and Medicare members in New Jersey. Services include blood pressure checks, BMI assessments and HbA1c tests; scheduling mammography appointments; and test kits for colorectal cancer and diabetic urine screenings. Read More
Wisconsin
Wisconsin Seeks to Extend Medicaid Postpartum Coverage to 90 Days. The Centers for Medicare & Medicaid Services announced on June 21, 2022, that Wisconsin Department of Health Services submitted to federal regulators a Section 1115 waiver request to extend postpartum Medicaid coverage to 90 days, up 30 days from current coverage for individuals with incomes above 100 percent of poverty. Public comments will be accepted through July 21, 2022. Read More
National
Black Medicaid Beneficiaries Have Lower Utilization, Spending than White Beneficiaries, Study Finds. Health Payer Intelligence reported on June 21, 2022, that Black Medicaid beneficiaries had lower utilization and cost than white beneficiaries, according to a JAMA study. However, the study also found that Black enrollees had higher emergency department use and rates of preventive care screenings. Read More
ACA Coincides With Improved Access to Diagnostic, Preventive Testing Among Low-Income Individuals, Study Finds. Health Payer Intelligence reported on June 21, 2022, that access to diagnostic and preventive testing rose among low-income individuals following the implementation of the Affordable Care Act (ACA), according to a study by JAMA Network Open. However, the study found little change in utilization and costs. The study is based on data for 123,100 individuals from the Medical Expenditure Panel Survey from 2011 to 2013 and 2014 to 2016. Read More
FTC to Boost Enforcement of Illegal Rebate Practices by PBMs. Fierce Healthcare reported on June 17, 2022, that the Federal Trade Commission (FTC) issued an enforcement policy statement aimed at illegal rebate practices by pharmacy benefit managers (PBMs) and other intermediaries. The FTC may issue fines or penalties to PBMs who are found to be engaging in these practices. Read More
CMS Approves 12-Month Postpartum Medicaid Coverage in District of Columbia, Maine, Minnesota, New Mexico. The Centers for Medicare & Medicaid Services (CMS) announced on June 16, 2022, approval of state plan amendments to expand Medicaid coverage for pregnant women and families to 12 months postpartum in Maine, Minnesota, New Mexico, and the District of Columbia. Read More
MedPAC Recommends CMS Improve Risk Adjustment Process for Medicare Advantage Plan Payments. Fierce Healthcare reported on June 17, 2022, that the Medicare Payment Advisory Commission (MedPAC) issued its biannual report to Congress, which included a recommendation aimed at improving the risk adjustment methodology used by the Centers for Medicare & Medicaid Services (CMS) to determine payments to Medicare Advantage plans. The recommendation would seek to address major cost outliers through redistributions instead of changes in capitated rates. Read More
Hospital Groups Urge CMS to Increase Fiscal 2023 Medicare Inpatient Prospective Payments. Modern Healthcare reported on June 20, 2022, that hospital groups are urging the Centers for Medicare & Medicaid Services (CMS) to increase the Medicare inpatient prospective payments for fiscal 2023 above the 3.2 percent increase included in a proposed rule. According to letters from the American Hospital Association, America’s Essential Hospitals, the Federation for American Hospitals, and Premier, the fiscal 2022 increase of 2.7 percent underpredicted inpatient hospital costs. Read More
Industry News
Pharmaceutical Company to Pay $233 Million in Medicaid Fraud Settlement. The Center Square reported on June 21, 2022, that Mallinckrodt ARD, formerly Questcor Pharmaceuticals, agreed to pay more than $233 million over seven years to settle a whistleblower lawsuit concerning underpayment of Medicaid drug rebates for H.P. Acthar Gel between 2013 and 2020. Funds will go to 50 states, District of Columbia, Puerto Rico, and the federal government. Acthar is used to treat certain chronic inflammatory or autoimmune conditions. Read More
Health Plan Loses Appeal Over Medicare Advantage Overpayments. Bloomberg reported on June 21, 2022, that the U.S. Supreme Court rejected an appeal by UnitedHealth Group seeking to overturn a federal rule requiring health plans to return Medicare Advantage overpayments. United won in district court, but the case was dismissed by the District of Columbia Court of Appeals in August 2021. Read More
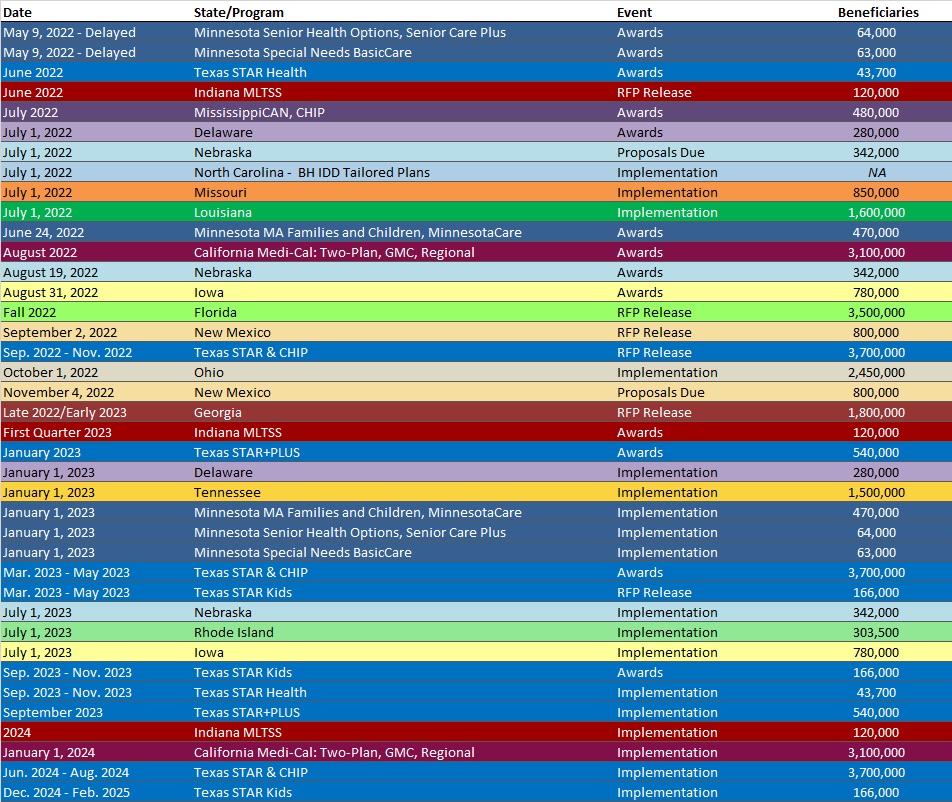
RFP Calendar
Company News
HMA News & Events
Quality Standards in Addiction Care. Across the healthcare landscape, quality standards are in place to ensure patients are receiving safe, appropriate, evidence-based, and standardized care that is tailored to their individual needs and symptomology. A significant gap has long existed in the treatment of SUD, as there was no standardized method to provide treatment based on an individual’s needs at that moment, meaning people seeking treatment often received care that was either too intense or not intense enough, preventing them from attaining sustained recovery. Read More
NEW THIS WEEK ON HMA INFORMATION SERVICES (HMAIS):
Medicaid Data
- Florida Medicaid Managed Care Enrollment is Up 11.3%, 2021 Data
- Georgia Medicaid Managed Care Enrollment is Up 4.4%, Jun-22 Data
- MassHealth Snapshot Enrollment Summary, 2012-22
- New York CHIP Managed Care Enrollment is Down 1.8%, May-22 Data
- New York Medicaid Managed Care Enrollment is Up 1.4%, May-22 Data
Public Documents:
Medicaid RFPs, RFIs, and Contracts:
- Florida Medicaid Managed Care Procurement RFI and Responses, 2022
- Minnesota Mental Health Case Management Services for Uninsured Adults RFP, Jun-22
- Mississippi MississippiCAN and CHIP RFQ and Amendments, 2021-22
- Nevada Medicaid FFS Pharmacy Benefits Manager RFP and Award, 2021
- New York Medicaid UR, Quality Improvement, Maternal Mortality Reviews Services Solicitation, Jun-22
Medicaid Program Reports, Data and Updates:
- Florida Medicaid Managed Care Rate Certifications and Related Documents, SFY 2021-22
- Iowa Medicaid MCO Quarterly Performance Data Reports, 2016-22
- New Jersey Medicaid, MLTSS Quality Technical Reports, CY 2020-21
- Texas Behavioral Health in Corrections Presentation to Legislature, Jun-22
- Texas Senate Finance Committee Presentation on Long-Term Care, Jun-22
A subscription to HMA Information Services puts a world of Medicaid information at your fingertips, dramatically simplifying market research for strategic planning in healthcare services. An HMAIS subscription includes:
- State-by-state overviews and analysis of latest data for enrollment, market share, financial performance, utilization metrics and RFPs
- Downloadable ready-to-use charts and graphs
- Excel data packages
- RFP calendar
If you’re interested in becoming an HMAIS subscriber, contact Carl Mercurio.
HMA WELCOMES:
Roxanne Kennedy, DSW, LCSW – Principal
Dr. Roxanne Kennedy is a licensed clinical social worker (LCSW) with more than thirty years of experience providing clinical and administrative services in various behavioral health settings including state agencies, state psychiatric hospitals, managed behavioral health care organizations, community mental health agencies and psychiatric emergency services.
Before joining HMA, Dr. Kennedy served as the chief executive officer and market president for Beacon Health Options of Pennsylvania. In this role, she assured responsiveness to behavioral health plan clients, brought innovation in programming, technology, and recovery principles to PA HealthChoices (Medicaid) members, managed medical loss ratio and led a team of 160 staff.
Dr. Kennedy held several positions at the New Jersey Department of Human Services (DHS) over 15 years. She was responsible for implementing the Substance Abuse Waiver approved by the Centers for Medicare & Medicaid Services (CMS) for the state’s Medicaid program and integrating behavioral health services into at-risk management. She also served as the project lead for the transitioning of mental health and addiction services from cost-related contracts to fee for service. In addition, she was responsible for Medicaid policy and oversight related to behavioral health services for those enrolled in the state’s Medicaid plan and worked to implement New Jersey’s Medicaid expansion benefit to include substance abuse services and other behavioral health services related to the Affordable Care Act. Additionally, she had oversight of the state’s block grant and worked closely with various state agencies to ensure coordinated state and federal funding of behavioral health services.
Dr. Kennedy maintained a private practice providing psychotherapy to individuals and families with mental health and substance abuse issues from 2002 through 2019 and worked for more than 10 years providing crisis services in an emergency department setting.
She completed her Doctorate in Clinical Social Work at University of Pennsylvania, School of Social Policy and Practice, and her dissertation is entitled “Evaluating Integrated Care Models for Individuals with Serious Mental Illness.” Dr. Kennedy also earned both a master’s and bachelor’s degree in social work administration from Temple University and is a LCSW in Pennsylvania.
Allie Franklin, LICSW – Principal
Allie Franklin is a licensed, independent clinical social worker with decades of experience working in public, private, and non-profit behavioral health, healthcare and social service organizations. She has led transformations in integrated care through modernizing processes, systems, workflows, policies, and approaches to achieve outstanding outcomes.
Having worked on the clinical front lines and advancing to senior and executive leadership roles, she brings a perspective of clinical, operational and strategic expertise which gives her the ability to support planning and implementation of solutions ranging from system and organization-wide approaches to day-to-day clinical level work.
Prior to joining HMA, she served the as the behavioral health service line administrator for the University of Washington’s Harborview Medical Center, the region’s only Level One Trauma Center. This role encompassed inpatient behavioral healthcare, emergency psychiatric services, a full outpatient clinic, and scattered site integrated behavioral health and primary care. As a part of her service line’s Center of Excellence, the Behavioral Health Institute, she managed a project to bring together multiple stakeholders to redesign Washington’s (WA) behavioral health crisis system in preparation for 988 crisis line rollout.
In her role as the associate vice president of clinical operations for a Medicaid managed care organization in Pierce County, WA, Allie led a multi-disciplinary team of executives and community stakeholders through the development and implementation of a detailed plan to integrate mental health services with substance use disorder services to create a behavioral health organization. Allie has also served as the chief executive officer for one of WA state’s two largest suicide hotlines where she led the transformation necessary to meet NCQA call quality standards.
With a passion for whole person wellness, for developing high performing teams, and helping clinical staff understand how their work impacts the financial bottom line, Allie has a unique combination of experiences across the care continuum. She has helmed projects ranging from crisis care and inpatient treatment to outpatient and integrated primary care models.
Her perspective, gained from leading on both sides of the payer relationship, gives her the ability to support system transformation to help build approaches that achieve high quality and affordability. She has a long track record of leading teams to achieve high quality results including reductions in average lengths of stay, re-hospitalization rates, improved customer and staff satisfaction, as well as developing dashboards that help providers, payers, and stakeholders understand the impacts of the work they do and the quality initiatives that they support.
Allie earned a Master of Science in Social Work from the University of Texas at Arlington, a Bachelor of Social Work from Missouri State University and is currently earning an Executive Master of Health Administration from the University of Central Florida. She served in the United States Air Force, reaching the rank of Captain, serving as Chief of Mental Health for Columbus Air Force Base, and as a clinical member of the international critical incident crisis response team.
Olivia Reding – Senior Consultant
An experienced researcher and project manager focused on maternal and child health, behavioral health, and health equity, Olivia Reding supports innovative public health research and delivery system reform efforts.
Olivia has led stakeholder engagement activities, work plan development, and strategic planning to improve and sustain contracts and pursue growth opportunities. She has also developed high-quality, engaging, and informative resources for national dissemination, as well as collected and analyzed quantitative and qualitative data to inform research opportunities and policy recommendations.
Prior to joining HMA, Olivia served as research project manager with IBM, where she supported contracts with a range of federal agencies including the Centers for Medicare and Medicaid Services, Agency for Healthcare Research and Quality and U.S. Food and Drug Administration. This work primarily centered on providing targeted technical assistance to Medicaid and Children’s Health Insurance Program agencies to improve maternal and child health, behavioral health, payment and care delivery, and data analytic capacity. Prior to her time at IBM, Olivia served as a research assistant at Boston Medical Center, where she contributed to studies focused on improving opioid prescribing practices and reducing injection drug use.
Olivia earned a Master of Public Health degree from Boston University with concentrations in epidemiology and maternal and child health, and a bachelor’s degree in economics and Spanish from Colgate University. She is also a certified Project Management Professional.
Susan Esparza, MS, APRN, FNP-C – Senior Consultant
Susan Esparza is a passionate and innovative healthcare executive with experience mentoring and leading teams and colleagues to attain organizational goals. She is a healthcare quality data expert who has sound knowledge and experience with Healthcare Effectiveness Data and Information Set (HEDIS), National Committee for Quality Assurance (NCQA), risk adjustment, and quality measures.
She joins HMA after serving as vice president of medical management with Troy Medicare where she developed and executed a unique pharmacy-centric model for rural and underserved counties. She also implemented a state management program for chronic complex conditions.
A family nurse practitioner, Susan brings clinical experience and a real-world view of the healthcare system to her consulting and is a member of several professional organizations and boards.
Her work with HEDIS has included leading strategic initiatives, incorporating information technology capabilities to create and analyze data, and utilizing quality measures to identify, review, and advise on improvement processes and new program implementations. She has helped organizations improve measures and align with quality and accreditation requirements.
Susan is an effective communicator and team-builder, with the ability to develop strategic plans to resolve complex issues and related concerns and has elevated colleagues to meet organizational goals.
She earned a Master of Science from Georgia State University, a bachelor’s degree from Mercer University, and a post-master certificate of Family Nurse Practitioner from the University of South Carolina. She holds a Lean Six Sigma Green Belt certification and is an advanced practice registered nurse and family nurse practitioner.
Judith Hutman – Principal
Working at the intersection of healthcare policy and technology for more than 20 years, Judith Hutman has deep experience and expertise supporting state and federal government projects and programs. She has led systems integration, worked translating policy into technology solutions, and modernized processes to better serve clients and patients.
Before joining HMA, she oversaw program delivery for a portfolio of federal health and human services projects for ManTech International supporting the Centers for Medicare and Medicaid Services (CMS), Health Resources and Services Administration, and the Food and Drug Administration.
Judith has led a variety of healthcare information technology (IT) projects including independent testing of the Federally Facilitated Exchange (HIX) at www.healthcare.gov and systems integration and project governance for Health Information Exchange (HIE). In addition, she oversaw the state Medicaid Management Information System (MMIS) replacement, and stakeholder engagement and interoperability testing for the Office of the National Coordinator for Health IT (ONC) Nationwide Health Information Network (NwHIN) Exchange and Direct. She also led technology modernization and cloud migration for mission-critical government healthcare applications and public health bio surveillance programs.
Having worked on translating policy into technology solutions, she brings strong program delivery skills combined with domain knowledge to successfully translate between business needs and technology solutions.
Judith has strong analytical and communication skills, and the ability to collaborate with a diverse range of stakeholders to navigate and translate complex health IT programs and data. She has established business process transformation and project governance frameworks that support focus on business objectives and actionable plans.
She is a project management professional with a certification from the Project Management Institute as well as certified cloud practitioner with Amazon Web Services.
Deena Pourshaban, MPH, PCMH, CCE – Senior Consultant
With expertise in practice transformation, program design and management, and strengthening primary care workforce, Deena Pourshaban has worked across the healthcare landscape focusing on public health and Patient Centered Medical Home (PCMH) management.
Before joining HMA, she served in several, more increasingly senior roles with Elevation Health Partners where she was a program director for the Los Angeles Practice Transformation Network (LAPTN), a four-year Centers for Medicare and Medicaid Services (CMS)-funded project aimed at preparing Federally Qualified Health Centers for value-based payment (VBP) and improving care for patients.
Deena was also involved in projects to implement data collection and use data to improve operations, achieve successful quality improvement measures, integrate social determinants of health (SDOH), and implement alternative payment models and VBP models.
She also served in positions with organizations including Kaiser Permanente, the Los Angeles County Department of Public Health, and the University of California, Los Angeles Medical Center, Department of Neurosurgery as well as abroad in internship and analyst roles in Uganda and Panama.
Focused on quality and improving metrics, she has experience analyzing projects related to HEDIS and public health metric interventions. In addition, Deena has experience conducting interviews and managing focus groups as well as preparing reports and recommendations to aide in project goal setting, strategic planning, and communications for a variety of stakeholders.
She will continue work supporting the Population Health Management Initiative (PHMI), a collaboration in California between the Department of Healthcare Services, the California Primary Care Association and Kaiser Permanente. She will lead the Enhanced Specialty Access workstream looking to implement strategies to increase specialty access for Medi-Cal patients.
Deena earned a Master of Public Health in biostatistics and epidemiology from the University of Southern California and a bachelor’s degree in human biology from the University of California, San Diego.
Jamie Titak, MBA – Senior Consultant
A healthcare technology expert, strategic planner, and healthcare executive, Jamie Titak has deep experience in electronic health records, healthcare informatics data, and integrating technology into operations.
Before joining HMA, Jamie served as corporate vice president with New York Life Insurance where she organized and led cross-functional initiatives to develop key strategic capabilities and introduce the use of digital health data for underwriting. Leading a pilot project, she evaluated new digital health data sources and developed partnerships with vendors and stakeholders.
Seeking to fill a gap in the market, Jamie founded the healthitmhealth.com to provide healthcare informatics data. It was used and cited by multiple organizations including the University of California and Epic Systems.
Jamie also has significant experience managing large scale projects and establishing complex integrations between health records, lab systems and information technology (IT) exchanges. She is proficient in several programming languages including JavaScript, CSS, SQL, XSLT, CACHE, HTML and has several healthcare IT certifications.
She earned a Master of Business Administration in quantities finance, corporate finance and economics from New York University, Stern School of Business as well as a bachelor’s degree with quadruple majors in mathematics, psychology, biochemistry and neuroscience from Indiana University.
